Last Updated on November 17, 2025 by Ugurkan Demir

At Liv Hospital, we know how complex Bone Marrow Transplantation (BMT) is. It’s a treatment that can change lives for those with blood cancers and serious marrow diseases. BMT is a term that might seem scary, but it’s a way to replace bad bone marrow with good stem cells.Learn about chemo used for bone marrow transplant Get the crucial facts on its powerful use in the BMT process and its amazing function now.
So, what is BMT in medical terms? It’s also known as hematopoietic stem cell transplantation. This process uses high-dose chemotherapy to kill the bad marrow. Then, healthy stem cells can grow in their place.
We focus on patient care at Liv Hospital. We use advanced chemotherapy to give hope to those with blood cancers and disorders. Our team helps guide patients through this complex treatment.
Key Takeaways
- BMT stands for Bone Marrow Transplantation, a treatment for various blood-related diseases.
- Chemotherapy plays a critical role in BMT by destroying diseased marrow.
- Liv Hospital is committed to providing internationally trusted care for complex treatments like BMT.
- BMT can potentially cure blood cancers and serious marrow disorders.
- Our hospital uses advanced chemotherapy protocols for effective treatment.
Understanding BMT: Definition and Medical Terminology

Knowing what BMT stands for in medical terms is key for patients and families. BMT, or Bone Marrow Transplantation, is a procedure. It replaces damaged or diseased bone marrow with a healthy one.
What Does BMT Stand for in Medical Terms?
In medical terms, BMT stands for Bone Marrow Transplant. It’s a key treatment for many diseases. It’s also known as a stem cell transplant, but they’re not the same.
The History and Evolution of Bone Marrow Transplantation
The idea of BMT has been around for decades. The first successful transplant was in 1968. Over time, it has improved a lot.
Today, BMT is used to treat many serious diseases. This includes leukemia, lymphoma, and genetic disorders.
“The development of bone marrow transplantation represents one of the most significant advances in the treatment of hematologic malignancies and other life-threatening diseases.”
-Explain experts in hematology and stem cell transplantation.
Key Terminology Associated with BMT
There are many terms related to BMT. Knowing them helps to understand the procedure better. Some important ones are:
- Autologous Transplant: Uses the patient’s own stem cells.
- Allogeneic Transplant: Uses stem cells from a donor.
- HLA Typing: Checks if the donor and recipient are a good match.
- Conditioning Regimen: Prepares the body for the transplant by weakening the immune system.
| Term | Description |
| Autologous BMT | Uses the patient’s own stem cells for the transplant. |
| Allogeneic BMT | Uses stem cells from a donor for the transplant. |
| HLA Typing | A test to determine the compatibility between donor and recipient. |
The Science Behind Bone Marrow and Its Function
Bone marrow is a spongy tissue inside some bones. It’s key to making blood cells. It’s a complex organ that helps our body make blood cells.
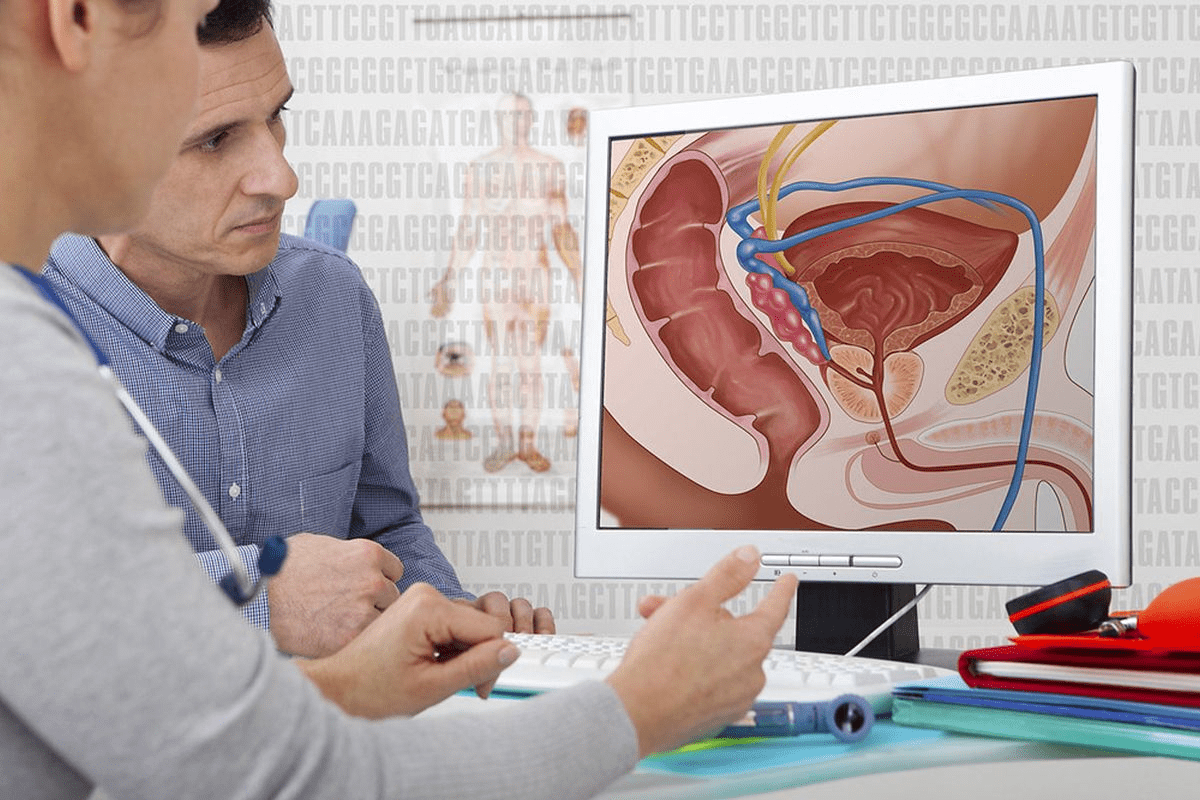
Anatomy and Physiology of Bone Marrow
Bone marrow is in the cavities of bones, like the hips and thighbones. It has blood vessels and special cells. There are two types: red marrow makes blood cells, and yellow marrow is mostly fat.
Red marrow has stem cells that turn into different blood cells. These include red blood cells, white blood cells, and platelets.
Role of Bone Marrow in Blood Cell Production
Bone marrow’s main job is to make blood cells through hematopoiesis. Stem cells in the bone marrow turn into different blood cells. Each type has its own job.
Red blood cells carry oxygen, white blood cells fight off infections, and platelets help blood clot. Bone marrow’s role is vital for our health.
When Bone Marrow Fails: Conditions Requiring Intervention
When bone marrow doesn’t work right, serious health problems can happen. Diseases like leukemia and lymphoma can harm it. Bone marrow transplantation (BMT) is a life-saving treatment for these issues.
BMT replaces damaged marrow with healthy one. It can be from the patient or a donor. Understanding bone marrow is key to seeing why BMT is important.
Types of Bone Marrow Transplants
Bone Marrow Transplants can be broadly classified into autologous, allogeneic, haploidentical, and cord blood transplants. Each type has its unique characteristics, advantages, and considerations.
Autologous Transplants: Using the Patient’s Own Cells
Autologous transplants use the patient’s own stem cells. This is often used for patients with certain cancers, like multiple myeloma or lymphoma. The process involves harvesting the patient’s stem cells, storing them, and then reinfusing them after high-dose chemotherapy.
Advantages of Autologous Transplants:
- No risk of graft-versus-host disease (GVHD)
- Faster engraftment
- Lower risk of complications related to donor cells
Allogeneic Transplants: Donor-Derived Stem Cells
Allogeneic transplants use stem cells from a donor. This donor can be a related or unrelated individual who has been matched for human leukocyte antigen (HLA) typing. Allogeneic transplants are often used for patients with leukemia or other blood disorders.
Considerations for Allogeneic Transplants:
- The need for a suitable HLA-matched donor
- Risk of GVHD
- Potential for graft-versus-leukemia effect
Haploidentical and Cord Blood Transplants
Haploidentical transplants involve using stem cells from a half-matched donor, often a family member. Cord blood transplants use stem cells from the umbilical cord blood of newborns. Both types are used when a fully HLA-matched donor is not available.
Benefits of Haploidentical and Cord Blood Transplants:
- Expanded donor pool
- Rapid availability of stem cells
- Potential for reduced GVHD with cord blood transplants
Understanding these different types of Bone Marrow Transplants helps patients and their families make informed decisions about their treatment options.
Diseases Treated with Bone Marrow Transplantation
BMT is a key treatment for serious health issues like some cancers and immune system diseases. It works by replacing a patient’s bad bone marrow with good, healthy marrow. This helps treat life-threatening conditions.
Blood Cancers: Leukemia, Lymphoma, and Multiple Myeloma
Blood cancers are a main focus of BMT. Leukemia is when there are too many white blood cells. Lymphoma affects the immune system’s lymphatic system. Multiple myeloma is a cancer of plasma cells in the bone marrow. BMT can cure these by getting rid of bad cells and adding healthy ones.
| Cancer Type | Description | Role of BMT |
| Leukemia | Cancer of the blood or bone marrow | Curative treatment by replacing cancerous cells with healthy stem cells |
| Lymphoma | Cancer of the lymphatic system | Potentially curative, even in tough cases |
| Multiple Myeloma | Cancer of plasma cells in the bone marrow | High-dose chemo followed by BMT to kill cancer cells |
Bone Marrow Failure Syndromes
Bone marrow failure syndromes, like aplastic anemia, happen when the marrow can’t make enough blood cells. BMT fixes this by putting in healthy donor stem cells. This helps the marrow work right again.
Immune Deficiency Disorders
Some immune disorders, like SCID, come from genetic problems. BMT can fix these by adding healthy stem cells. These cells grow into a strong immune system.
Is a Bone Marrow Transplant a Cure? Understanding Outcomes
The word “cure” is tricky with BMT. For many, BMT is a chance for a cure, mainly for blood cancers and some disorders. But success depends on the disease, the patient’s health, and the donor match. We’ll look into what success really means for BMT patients.
Chemo for Bone Marrow Transplant: The Conditioning Process
Chemotherapy is key in bone marrow transplants. It gets rid of bad bone marrow and makes room for new, healthy cells. This step is vital for the transplant’s success.
Why Chemotherapy is Essential in BMT
Chemotherapy is a vital part of bone marrow transplants. It kills the bad bone marrow and weakens the immune system. This makes it easier for new cells to take their place.
We pick the right chemotherapy for each patient. It depends on their disease, health, and the transplant type.
High-Dose vs. Reduced-Intensity Conditioning
There are two main ways to prepare for a transplant: high-dose and reduced-intensity conditioning. High-dose conditioning uses strong chemotherapy and sometimes radiation. It’s for those with aggressive cancers.
Reduced-intensity conditioning uses lower doses of chemotherapy. It’s for older patients or those with health issues that make them more sensitive to strong chemotherapy.
Common Chemotherapy Agents Used in BMT
Several chemotherapy agents are used in bone marrow transplants. These include:
- Cyclophosphamide
- Busulfan
- Melphalan
- Fludarabine
These drugs are mixed to get the best results. The choice depends on the patient’s disease and health.
Radiation Therapy as Part of Conditioning
In some cases, radiation therapy is added to chemotherapy. Total Body Irradiation (TBI) gives a uniform dose of radiation to the whole body. It’s used for some cancers.
TBI kills cancer cells and weakens the immune system. This helps the new stem cells to take hold. But it’s a complex process that needs careful planning to avoid side effects.
The Bone Marrow Transplant Procedure: Step by Step
Bone marrow transplantation is a complex process. It offers hope to those with blood-related disorders. The steps include initial evaluation, preparation, stem cell collection, the transplant itself, and post-transplant care.
Pre-Transplant Evaluation and Preparation
Before a bone marrow transplant, patients undergo a detailed evaluation. This includes a series of tests like blood work and imaging studies. These tests check if the patient can handle the transplant.
We also help patients prepare emotionally and psychologically. We give them all the information they need about the transplant and what to expect afterward.
Stem Cell Collection Methods
There are different ways to collect stem cells for the transplant. The most common is peripheral blood stem cell collection. This method mobilizes stem cells into the bloodstream, which are then collected using apheresis.
Bone marrow harvesting is another method. It involves directly collecting stem cells from the bone marrow, usually from the hip bones, under anesthesia.
The Transplantation Process
The actual transplant involves infusing the collected stem cells into the patient’s bloodstream. This process is relatively quick, taking about 1-2 hours. It is generally painless.
After infusion, the stem cells move to the bone marrow. There, they start producing new blood cells.
Post-Transplant Care and Recovery
Post-transplant care is key to the transplant’s success. Patients are watched for signs of engraftment and any complications. This includes graft-versus-host disease (GVHD).
Supportive care includes preventing infections and managing side effects. It also involves nutritional support to help patients regain strength and immune function.
Finding a Donor: The Importance of Genetic Matching
Finding a bone marrow donor who is genetically matched is key to a successful transplant. Genetic matching helps avoid serious problems like graft-versus-host disease (GVHD). GVHD happens when the donor’s immune cells attack the recipient’s body.
When looking for a bone marrow donor, HLA typing is very important. HLA typing checks for specific genes that control the immune system. A good match in HLA typing is essential for the transplant’s success.
HLA Typing and Compatibility Factors
HLA typing tests for specific antigens on white blood cells. The more antigens that match, the lower the risk of GVHD. There are different ways to do HLA typing, with molecular typing being more accurate.
Why Close Relatives Often Make the Best Donors
Bone marrow from a close relative is often the best choice because of genetic matching. Siblings are usually the best donors because they have a higher chance of being a match. Parents and children can also donate, but the match might not be as good as with siblings.
- Siblings have a 25% chance of being a match.
- Parents are usually a half-match.
- Children can be a partial match, depending on the genetic inheritance.
The Process of Donor Search and Selection
Finding a donor starts with HLA typing of family members. If no match is found, a search is done through national and international registries. The search can take a long time and includes checking the donor’s health and willingness to donate.
Becoming a Bone Marrow Donor: What to Know
To become a bone marrow donor, you need to register and get HLA typed. You should be healthy and willing to donate. The donation process can be either peripheral blood stem cell collection or bone marrow harvesting under anesthesia.
Deciding to become a bone marrow donor is a big choice. It’s important to know all the details before making a decision. By donating, you can save lives and make a big difference for patients needing bone marrow transplants.
The Patient Experience During BMT
Going through a Bone Marrow Transplant (BMT) is a big change. It brings physical and emotional challenges. Knowing what to expect can help reduce fear and uncertainty.
Physical Aspects: Is BMT Painful?
The physical side of BMT can be tough. The transplant itself isn’t usually painful because of anesthesia. But the prep work can hurt a lot.
Chemotherapy and radiation therapy are used to prepare for the transplant. These can cause mucositis, which is very painful.
Patients often feel tired, sick to their stomach, and in pain during this time. But thanks to better pain management, these symptoms are easier to handle now.
Hospital Stay and Isolation Requirements
How long a patient stays in the hospital and if they need to be isolated depends on their health and the treatment center’s rules. Most patients need to stay isolated to avoid getting sick. This is because their immune system is weak from the treatment.
| Isolation Requirement | Duration | Purpose |
| Strict Isolation | Several weeks | To minimize infection risk during the most vulnerable period |
| Partial Isolation | Varies | To reduce exposure to possible infection sources |
Common Side Effects and Complications
BMT can lead to many side effects and complications. These include graft-versus-host disease (GVHD), infections, and damage to organs. The chance of these problems depends on the type of transplant, the patient’s health, and the treatment used.
Some common side effects are:
- Fatigue
- Nausea and vomiting
- Mucositis
- Hair loss
Emotional and Psychological Impacts
The emotional and psychological effects of BMT are very important. It can be very hard, leading to anxiety, depression, and fear about the future. It’s key to have support from loved ones, friends, and mental health experts to deal with these feelings.
Recovery and Life After Bone Marrow Transplant
The journey to recovery after BMT is complex. It involves rebuilding the immune system and managing long-term side effects. Knowing the different stages and needs is key for patients and caregivers.
Timeline for Immune System Recovery
Recovering from BMT takes time, from months to years. The exact time depends on the transplant type, the treatment used, and the patient’s health.
- Early Recovery (0-3 months): Patients are very sick and at high risk for infections.
- Intermediate Recovery (3-12 months): The bone marrow starts working, but patients need careful watching.
- Late Recovery (1-2 years and beyond): The immune system keeps getting better, but some risks stay.
Follow-up Care and Monitoring
Regular check-ups are vital for recovery. They help catch problems early, like relapse or GVHD.
| Follow-up Care Aspect | Description | Frequency |
| Blood Tests | Checks blood counts, immune health, and toxicity | Weekly to monthly, based on the time post-transplant |
| Clinic Visits | Looks at overall health, GVHD, and relapse | Set times, maybe weekly or biweekly at first |
| Imaging Studies | Looks for disease return or other problems | As needed, based on signs |
Long-term Side Effects and Management
Long-term effects can include GVHD, hormonal issues, secondary cancers, and heart problems. Treatment plans are made for each person. They might include medicine, lifestyle changes, and regular checks.
Chronic GVHD management might include drugs and supportive care to ease symptoms and stop it from getting worse.
Quality of Life Considerations
Life after BMT affects many areas, like physical health, mood, and social life. A full care approach is important. It looks at medical, emotional, and social needs.
Understanding the recovery process helps patients and families deal with BMT’s challenges. This way, they can get the best results.
Advances in BMT: New Technologies and Approaches
BMT has seen big changes thanks to new research. This includes work on reduced-intensity conditioning, CAR T-cell therapy, and gene therapy. These breakthroughs are changing how we treat blood diseases, giving hope to many patients.
Reduced-Intensity Conditioning Regimens
Reduced-intensity conditioning (RIC) is a big step forward in BMT. It helps older patients or those with health issues who can’t handle strong treatments. RIC regimens use lower doses of chemotherapy and/or radiation, making treatments safer but effective enough for new cells to grow.
“The use of RIC has expanded the eligibility for BMT to a broader patient population, improving overall survival and reducing treatment-related mortality,” notes a recent study on RIC outcomes.
CAR T-Cell Therapy and BMT
CAR T-cell therapy is a new way to fight some blood cancers. It genetically modifies a patient’s T cells to recognize and target cancer cells. It’s not a replacement for BMT but is used alongside it to help patients.
- CAR T-cell therapy has shown significant efficacy in treating relapsed or refractory B-cell lymphomas and leukemias.
- It can induce deep remissions, potentially allowing patients to proceed to BMT in a more favorable disease state.
- Ongoing research is exploring the integration of CAR T-cell therapy with BMT to enhance outcomes and reduce relapse rates.
Gene Therapy Applications
Gene therapy is also advancing fast, promising new treatments for BMT patients. It modifies or repairs genes within a patient’s cells, aiming to treat or prevent disease. In BMT, it could fix genetic problems that cause blood disorders.
Recent trials show gene therapy’s promise in treating sickle cell disease and beta-thalassemia. It might offer a cure without the need for BMT.
Future Directions in Transplantation Medicine
Looking ahead, BMT is set for even more changes. New trends and technologies are on the horizon. These include:
- The development of more targeted and less toxic conditioning regimens.
- Advances in haploidentical transplantation are making BMT more accessible to patients without a matched donor.
- The integration of artificial intelligence and machine learning to optimize donor selection and predict patient outcomes.
“The future of BMT is bright, with ongoing research and technological advancements promising to improve patient outcomes and expand the reach of this life-saving therapy,” according to a leading expert in the field.
Conclusion:
The Life-Saving Bone Marrow Transplantation (BMT) has changed the game for treating serious diseases. It gives hope to people all over the world. BMT helps those with blood cancers, bone marrow problems, and immune system issues live healthier lives.
BMT works by replacing bad bone marrow with good cells. These cells can come from the patient or a donor. Thanks to better treatments and care, more people are living longer and healthier after BMT.
As BMT keeps getting better, so do the chances for patients. New ways like CAR T-cell therapy are making things even more hopeful. Our look into BMT shows its key role in medicine. It’s a reminder of the need for more research and support for this life-saving treatment.
FAQ
What does BMT stand for in medical terms?
BMT stands for Bone Marrow Transplant. It’s a procedure where damaged or diseased marrow is replaced with healthy cells.
What is the purpose of chemotherapy in a bone marrow transplant?
Chemotherapy is used to destroy diseased bone marrow. It makes space for healthy stem cells.
Is a bone marrow transplant a cure for blood cancers?
Yes, a bone marrow transplant can cure various blood cancers. This includes leukemia, lymphoma, and multiple myeloma.
What are the different types of bone marrow transplants?
There are several types of bone marrow transplants. These include autologous (using the patient’s own cells), allogeneic (using donor-derived stem cells), haploidentical, and cord blood transplants.
Why is genetic matching important in bone marrow transplantation?
Genetic matching is key to reducing the risk of graft-versus-host disease. It ensures the transplant’s success.
Is BMT a painful procedure?
The transplant process itself is not typically painful. But patients may feel discomfort and side effects during and after.
How is a bone marrow donor selected?
Donors are chosen based on genetic compatibility with the patient. Close relatives often make the best match.
What is the recovery process like after a bone marrow transplant?
Recovery involves a hospital stay. It also includes ongoing follow-up care and monitoring. This helps manage side effects and ensure the transplant’s success.
Can a bone marrow transplant cure bone marrow failure syndromes?
Yes, a bone marrow transplant can cure certain bone marrow failure syndromes.
What are the long-term side effects of a bone marrow transplant?
Long-term side effects include graft-versus-host disease, infections, and other complications. These are managed through ongoing care and monitoring.
References
- Shimoni, A., Radici, V., & Nagler, A. (2024). Conditioning. In The EBMT Handbook: Hematopoietic Cell Transplantation and Cellular Therapies (8th ed.). https://www.ncbi.nlm.nih.gov/books/NBK608297/