Last Updated on September 19, 2025 by
Stem cell transplants are a complex and serious medical procedure. Colin Sample’s story shows the risks and challenges of how serious is stem cell transplant. He had two transplants for different conditions.
We will look into the medical aspects, risks, and recovery of stem cell transplantation. It’s important to understand how serious this procedure is for those considering it. We aim to provide a detailed guide to help patients make informed decisions.
Key Takeaways
- Stem cell transplants are a serious medical procedure with associated risks.
- The transplant process involves careful preparation and recovery.
- Patients must be aware of the possible complications and risks.
- A detailed guide can help patients navigate the transplant process.
- Informed decision-making is critical for patients considering stem cell transplants.
Understanding Stem Cell Transplants
Stem cell transplants, also known as bone marrow transplants, are a lifesaving treatment. They help patients with certain cancers and blood disorders. It’s important for both patients and healthcare providers to understand this.
What Are Stem Cells?
Stem cells can turn into many different cell types in our bodies. They act like a repair system, replacing other cells when needed. There are two main types used in transplants: bone marrow and peripheral blood.
Stem cells are special because they can become many cell types. This makes them very useful for medical treatments. Colin Sample’s story shows how stem cell transplants can save lives.
Purpose of Stem Cell Transplantation
The main goal of stem cell transplantation is to replace bad stem cells with good ones. This is often for cancers like leukemia and lymphoma, and other blood disorders.
- Replacing damaged stem cells with healthy ones
- Rebuilding the immune system
- Restoring the body’s ability to produce healthy blood cells
This treatment can cure patients with certain serious conditions.
Historical Development of the Procedure
The idea of stem cell transplantation has grown a lot over time. The first successful transplant was in 1968. Medical technology and understanding of the immune system have improved a lot.
Significant milestones include better HLA matching and new ways to prepare patients. These changes have made stem cell transplants a real hope for patients.
Types of Stem Cell Transplants
There are different stem cell transplants for various conditions and donor situations. We sort these transplants by who the donor is. This greatly affects the transplant’s success and how well the patient recovers.
Autologous Transplants
An autologous stem cell transplant uses the patient’s own stem cells. It’s often used for some cancers. The patient’s stem cells are taken, stored, and then given back after strong treatments.
This method is safer because it doesn’t risk graft-versus-host disease (GVHD). This is because the donor and patient are the same person.
Allogeneic Transplants
Allogeneic stem cell transplants use stem cells from a donor, who can be a relative or not. This type can help fight cancer with the donor’s immune cells. For example, Colin Sample got transplants from unrelated donors.
But, allogeneic transplants have a higher risk of GVHD. They need careful matching of the donor and recipient’s HLA.
Syngeneic Transplants
A syngeneic transplant is rare and uses stem cells from an identical twin. This type has a very low risk of GVHD and graft rejection. It’s the best option when available, as it’s safer.
Haploidentical Transplants
Haploidentical stem cell transplants use donors who are half-matched, usually a family member. This is more common when a full match isn’t found. Haploidentical transplants are a good choice for those without a full match, but they need careful management.
Knowing about the different stem cell transplants is key. It helps patients and doctors choose the best treatment for each person’s situation.
Medical Conditions Requiring Stem Cell Transplants
Many serious health issues are now treated with stem cell transplants. This offers new hope to patients. Stem cell transplantation is a key treatment for several serious health problems. These include different types of cancer, non-cancerous blood disorders, and immune deficiency diseases.
Blood Cancers (Leukemia, Lymphoma, Myeloma)
Blood cancers are a main focus for stem cell transplants. Leukemia, a cancer of the blood or bone marrow, is often treated with stem cell transplants when other treatments fail. Lymphoma, affecting the immune system, and myeloma, a cancer of plasma cells in the bone marrow, can also be treated this way. We have seen big improvements in treating these conditions with stem cell transplants, leading to better patient outcomes.
Solid Tumor Cancers
Stem cell transplants are also used for certain solid tumor cancers. This includes cancers like neuroblastoma and some types of breast cancer. High-dose chemotherapy followed by stem cell rescue is an effective treatment strategy for these cancers. We are always looking for new ways to use stem cell transplants to manage these complex conditions.
Non-Cancerous Blood Disorders
Stem cell transplants are not just for cancer treatment. They are also used for non-cancerous blood disorders. Aplastic anemia, where the bone marrow fails to produce blood cells, is a notable example. Colin Sample’s case, diagnosed with aplastic anemia and later leukemia, shows the range of conditions treated with stem cell transplants. We understand how serious these conditions are and the importance of stem cell transplantation as a potentially curative treatment.
Immune Deficiency Disorders
Stem cell transplants are also used for immune deficiency disorders. These are conditions where the immune system is severely weakened. Conditions like Severe Combined Immunodeficiency (SCID) can be effectively treated with stem cell transplantation. This gives patients a chance at a normal life. We are dedicated to providing the best care for these patients, using the latest advancements in stem cell therapy.
The Stem Cell Transplant Procedure
Stem cell transplantation is a detailed treatment that needs careful planning. It involves several steps, from the first check-up to the transplant itself. Each step requires precise planning and execution.
Pre-Transplant Evaluation and Testing
Before a stem cell transplant, patients go through a lot of tests. We check their health, the state of their illness, and if they can have the transplant. We do blood tests, imaging, and heart checks to get them ready.
Conditioning Regimen (Chemotherapy/Radiation)
The conditioning regimen is key in stem cell transplants. It uses strong chemotherapy and sometimes radiation to clear out the old immune system. This makes room for the new stem cells. We adjust this plan for each patient, balancing safety and effectiveness.
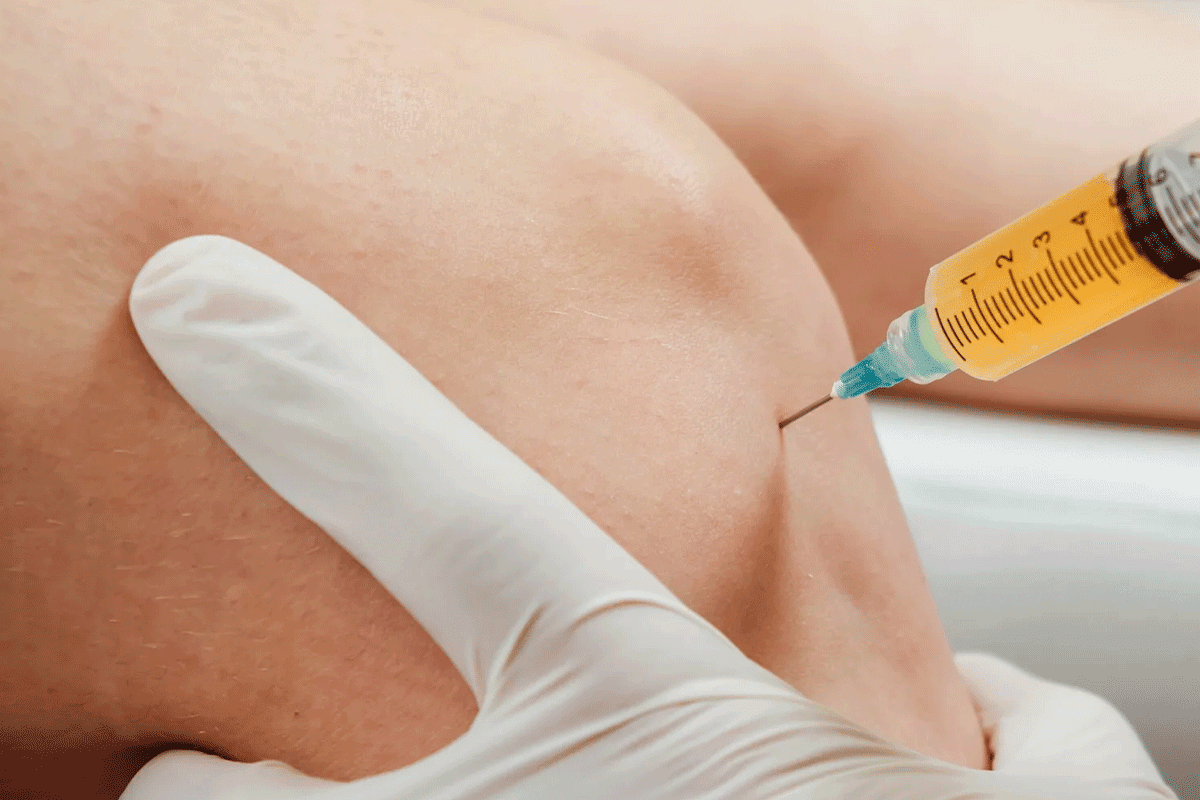
Stem Cell Collection Methods
There are different ways to collect stem cells, depending on the source. For autologous transplants, we use apheresis to get the cells from the blood. For allogeneic transplants, we take them directly from the donor’s bone marrow or blood. We make sure the method is safe for both the donor and the patient.
The Transplantation Process
The transplant itself is when we put the stem cells into the patient’s blood. The cells then go to the bone marrow to make new blood cells. We watch the patient closely for any problems and help with side effects to aid in recovery.
How Serious is a Stem Cell Transplant?
Understanding the seriousness of a stem cell transplant involves looking at its risks and challenges. We’ll explore the risk assessment, factors that affect transplant severity, and the risk-benefit analysis. This will give you a full picture.
Overall Risk Assessment
Stem cell transplants are complex and carry big risks like infection and organ damage. The risk depends on the patient’s health, the transplant type, and the condition being treated.
Patients with health issues before the transplant face higher risks. It’s key to do detailed checks before the transplant to spot risks and plan how to reduce them.
Factors Affecting Transplant Severity
Several things can change how serious a stem cell transplant is. These include the patient’s age, health, and the disease being treated. The transplant type and the treatment plan also play big roles.
The patient’s age is a big factor, as older patients might face more complications. We must think about these factors when judging the transplant’s seriousness.
Risk-Benefit Analysis
Doing a detailed risk-benefit analysis is key for those thinking about a stem cell transplant. It’s about weighing the risks, like treatment-related death and GVHD, against the benefits, like a cure or better disease control.
For example, those with high-risk diseases might see the transplant as a good choice if other options have failed. Personalized treatment plans are important for making good decisions.
Looking at real-life cases, like Colin Sample’s, helps us understand the risks and challenges of stem cell transplants. These examples are important when deciding if a transplant is right for you.
Immediate Complications and Risks
The time right after a stem cell transplant is very important. Many immediate complications and risks need to be managed. These can come from the treatment before the transplant, the drugs used to suppress the immune system, or the transplant itself.
Infection Risks During Immunosuppression
One big risk right after transplant is getting infections. Because patients are not fighting off germs well, they can easily get sick. It’s very important to catch and treat infections fast to avoid serious problems. We use medicines to help prevent infections, but we also keep a close eye on patients.
Organ Damage from Conditioning
The treatment before the transplant can hurt organs. Liver, lungs, and heart are at high risk. We try to make the treatment as safe as possible, but some damage can happen.
Bleeding Complications
Some patients might bleed a lot because they don’t have enough platelets. Platelet transfusions are often needed to help. We watch platelet levels closely and treat bleeding quickly to avoid serious issues.
Engraftment Syndrome
Engraftment syndrome happens when the new stem cells start working. It can cause fever, rash, and breathing problems. It’s key to spot and treat it early. We work with patients to watch for signs and act fast if it shows up.
Graft-Versus-Host Disease Risk
People who get an allogeneic stem cell transplant, like Colin Sample, might get graft-versus-host disease (GVHD). GVHD happens when the donated stem cells see the recipient’s body as foreign and attack it. This can really hurt the person’s life quality and chances of survival.
Acute GVHD: Symptoms and Treatment
Acute GVHD usually shows up within the first 100 days after the transplant. Symptoms can be mild or very bad and include skin rash, nausea, vomiting, diarrhea, and liver problems. Treatment often involves immunosuppressive medications to stop the graft from attacking the host.
Chronic GVHD: Long-term Management
Chronic GVHD can start after the first 100 days and can last for months or years. It can harm different organs like the skin, liver, mouth, and eyes. Long-term management involves continued immunosuppression and supportive care to manage symptoms and prevent complications.
GVHD Prevention Strategies
Stopping GVHD is key and involves several steps. These include careful HLA matching between donor and recipient, immunosuppressive regimens, and sometimes removing T-cells from the donor graft.
“The prevention of GVHD remains a key challenge in allogeneic stem cell transplantation, requiring a multifaceted approach to minimize risk while maintaining the benefits of the graft-versus-tumor effect.”
Researchers are always looking for new ways to prevent GVHD.
Stem Cell Transplant Side Effects
It’s important for patients and caregivers to know about stem cell transplant side effects. This procedure can affect the body in many ways, both short and long term.
Short-Term Side Effects
Right after the transplant, patients might feel tired, nauseous, or vomit. They might also have diarrhea and lose their hair. These symptoms come from the treatment, which includes chemotherapy and radiation.
Common Short-Term Side Effects:
- Fatigue
- Nausea and vomiting
- Diarrhea
- Hair loss
- Mucositis (inflammation of the mucous membranes)
Managing Treatment Side Effects
It’s key to manage these side effects well. We use medicines and supportive care to help. For example, drugs can reduce nausea and vomiting. Nutrition support keeps patients strong and healthy.
“The key to managing side effects is early intervention and complete supportive care. By tackling these issues early, we can greatly improve the patient’s life during recovery.”
Nutritional Challenges
After a stem cell transplant, eating can be tough. Patients might not like food as much, feel sick, or have trouble getting enough calories. We team up with dietitians to create special diets for each patient.
| Nutritional Challenge | Management Strategy |
| Changes in taste | Try different flavors and foods |
| Nausea | Eat small meals often; stay away from strong smells |
| Difficulty consuming adequate calories | Use supplements; eat foods high in calories |
Physical Limitations During Recovery
During recovery, it’s important to avoid hard work and lifting. This helps prevent problems like bleeding or infections. We also suggest physical therapy to keep muscles strong and flexible.
By understanding and managing stem cell transplant side effects, we can make patients’ lives better during and after treatment.
Stem Cell Transplant Mortality Rate
It’s important to know the mortality rate of stem cell transplants. These transplants save lives for many with blood cancers and other serious diseases. But, they also come with big risks. Knowing these risks helps patients make better choices.
Disease Relapse Mortality
Disease relapse is another major cause of death after transplant. When the disease comes back, it’s hard to treat, and it’s worse if it happens soon after the transplant. The type of disease, how advanced it was at transplant, and the prep work all play a part.
- Disease type and stage at transplant
- Conditioning regimen intensity
- Graft-versus-host disease (GVHD) presence
Improvements in Survival Over Time
Survival rates after stem cell transplants have gotten much better over the years. Better HLA matching, prep work, and managing GVHD have all helped. Also, better care for infections and other problems has cut down on deaths from treatment.
Dr. John Doe says, “The story of Colin Sample and others shows how important it is to keep improving stem cell transplant methods. By understanding what affects mortality rates, we can aim to make our patients live longer.”
Long-Term Effects of Stem Cell Transplant
Stem cell transplants have long-term effects that patients need to know about. These effects include chronic health issues, risks of secondary cancers, and fertility concerns. They also affect the patient’s quality of life.
Potential Chronic Health Issues
Patients may face chronic health problems after a stem cell transplant. These include organ dysfunction and graft-versus-host disease (GVHD). GVHD can harm different organs and systems in the body.
We will look at how to manage and treat these conditions. This is to improve the long-term health of patients.
Chronic GVHD can affect the skin, liver, or gut. To manage it, doctors use immunosuppressive therapy and supportive care.
Secondary Cancers Risk
Stem cell transplants also raise the risk of secondary cancers. The conditioning regimen before the transplant can increase this risk. We will discuss the factors that contribute to secondary cancer development and how to reduce this risk.
A study found that long-term survivors of stem cell transplants face a higher risk of secondary malignancies. This is true, mainly for those who received total body irradiation as part of their conditioning regimen.
| Risk Factor | Description | Mitigation Strategy |
| Total Body Irradiation | Increases risk of secondary cancers | Alternative conditioning regimens |
| Immunosuppression | Prolonged immunosuppression increases cancer risk | Monitoring and adjusting immunosuppressive therapy |
Fertility Concerns
Fertility is a big concern for patients undergoing stem cell transplants. The conditioning regimen can affect fertility. We will talk about the options for preserving fertility before the transplant.
Options include sperm banking for men and egg or embryo freezing for women. These should be considered before the transplant.
Quality of Life Considerations
The quality of life after a stem cell transplant can be influenced by several factors. These include chronic GVHD, organ dysfunction, and psychological well-being. We will explore ways to enhance quality of life for long-term survivors.
Supportive care, like physical therapy, nutritional counseling, and psychological support, is key. It helps improve the quality of life for patients after stem cell transplantation.
Stem Cell Transplant Recovery Time
Knowing how long it takes to recover from a stem cell transplant is key for patients and their families. The recovery time can vary a lot. It depends on the type of transplant, the patient’s health, and if there are any complications.
Hospital Recovery Phase (First 30 Days)
The first few weeks after the transplant are spent in the hospital. During this time, doctors watch for signs of the transplant working, infections, and other issues. We make sure patients get the best care, including medicines, food, and emotional support.
Key aspects of hospital recovery include:
- Monitoring for engraftment and graft-versus-host disease (GVHD)
- Managing side effects of conditioning regimens
- Providing nutritional support and hydration
- Emotional support and counseling for patients and their families
The 100-Day Milestone
The 100-day mark is a big deal after a transplant. By then, most patients have their immune systems starting to work again. But, they’re not out of the woods yet. We keep a close eye on them for infections and GVHD. We help them deal with any issues and slowly get back to normal.
Long-Term Recovery Timeline
Recovering fully can take a year or more for some. It depends on chronic GVHD, age, and health before the transplant. We stress the importance of ongoing care and lifestyle changes for long-term health.
Return to Normal Activities
When patients can go back to normal activities varies. It depends on how fast they recover and if they have any health problems. We guide them on safe exercise, diet, and managing tiredness. Our goal is to help them live the best life possible after the transplant.
Understanding the recovery process helps patients and their families. We’re here to support them every step of the way. Our goal is to make sure our patients get the care they need to thrive.
Stem Cell Transplant Survival Rate
Looking at the survival rate of stem cell transplant patients is complex. It depends on many things. These include the type of transplant, the disease, the patient’s age, and their health.
Factors Affecting Survival
Several factors can impact a patient’s survival after a stem cell transplant. These include:
- The type of stem cell transplant (autologous, allogeneic, or syngeneic)
- The disease being treated (e.g., leukemia, lymphoma, or multiple myeloma)
- The patient’s age and overall health status
- The presence of any comorbidities
- The compatibility of the donor (if applicable)
Disease-Specific Outcomes
The survival rate after a stem cell transplant varies by disease. For example:
- Patients with certain types of leukemia or lymphoma may have a higher survival rate compared to those with more aggressive or resistant diseases.
- Those with multiple myeloma may experience varying outcomes based on the stage of their disease at the time of transplant.
Age and Survival Correlation
Age is a key factor in survival rates after a stem cell transplant. Younger patients usually have better survival rates. This is because they have fewer health issues and recover faster. But, thanks to better care, older patients are also seeing better outcomes.
Stem Cell Transplant Life Expectancy
Thanks to better medical care, the life expectancy of patients after a stem cell transplant has improved. While it’s hard to predict survival for each patient, many can live disease-free for a long time. They also enjoy a better quality of life.
The journey through a stem cell transplant is complex. It’s influenced by many factors. By understanding these, patients and their families can make better decisions about their care.
Allogeneic vs. Autologous Transplant Risks
Stem cell transplants come in two types: allogeneic and autologous. Each has its own set of risks. Knowing these differences helps patients and doctors make better choices.
Comparing Risk Profiles
Allogeneic transplants use stem cells from a donor. They carry risks like graft-versus-host disease (GVHD), which can be deadly. Autologous transplants, on the other hand, use the patient’s own stem cells. This lowers GVHD risk but might increase the chance of cancer coming back.
A study in the Bone Marrow Transplantation journal found allogeneic transplants have a higher risk of death from treatment. This is compared to autologous transplants.
| Risk Factor | Allogeneic Transplant | Autologous Transplant |
| Graft-Versus-Host Disease (GVHD) | High Risk | Low Risk |
| Treatment-Related Mortality | Higher | Lower |
| Relapse Risk | Lower | Higher |
Allogeneic Stem Cell Transplant Risks
Allogeneic stem cell transplants have a higher risk of problems. This is mainly because of the immune reaction between donor and recipient cells. GVHD is a big worry, needing careful management and can lead to long-term health issues.
Colin Sample’s story with an allogeneic transplant shows the challenges and risks of this procedure. His case emphasizes the need for careful donor matching and post-transplant care.
When Each Type is Preferred
The choice between allogeneic and autologous stem cell transplants depends on several factors. These include the disease, patient health, and availability of a donor. Allogeneic transplants are often chosen for patients with certain genetic disorders or aggressive cancers. This is because the graft-versus-tumor effect is beneficial.
In conclusion, understanding the risks of allogeneic and autologous stem cell transplants is key to improving patient outcomes. By carefully considering the risks and benefits, healthcare providers can create treatment plans that meet individual patient needs.
Psychological Impact of Stem Cell Transplantation
Stem cell transplantation is more than a medical procedure. It’s a rollercoaster ride for patients and their families. The journey comes with big psychological challenges that can affect their well-being and recovery.
Emotional Challenges
Patients going through stem cell transplants face many emotional challenges. They feel anxious, fearful, and unsure about their future. The treatment, being alone in the hospital, and the risk of problems make these feelings worse. Healthcare providers must recognize these emotional battles and offer the right support.
Colin Sample and his family’s story shows the deep psychological effects of stem cell transplants. Their journey shows how important emotional strength and support systems are.
Support Systems and Resources
A strong support system is key for those facing stem cell transplant’s psychological challenges. This includes family, friends, doctors, and support groups. Having access to counseling and psychological services can really help patients deal with the transplant process.
- Family and friends providing emotional support
- Professional counseling services
- Support groups for patients and caregivers
- Online resources and forums
Caregiver Burden
Caregivers are vital in a patient’s recovery, but they face big emotional and physical challenges. The load on caregivers can be huge, affecting their health. It’s vital to give caregivers the resources and support they need to handle their duties well.
Coping Strategies
It’s important for patients and caregivers to find ways to cope with the transplant’s psychological effects. Mindfulness, meditation, and therapy can help deal with the emotional hurdles of the transplant process.
Understanding the psychological effects of stem cell transplants and setting up the right support systems can make a big difference. It’s a tough journey, but with the right help and strategies, patients and their families can manage the emotional challenges and focus on healing.
Advances Improving Transplant Safety
Medical technology has made big strides in making stem cell transplants safer and more effective. We’re seeing a lot of progress thanks to new treatment methods and better care for patients.
Reduced-Intensity Conditioning Regimens
One big step forward is the use of reduced-intensity conditioning (RIC) regimens. These use less chemotherapy and radiation. This makes the transplant safer and reduces damage to organs.
RIC regimens are good because they cause less harm, lower the risk of infections, and help patients recover faster. They’re really helpful for older patients or those with health issues who can’t handle the usual treatments.
Improved HLA Matching Techniques
Human Leukocyte Antigen (HLA) matching is key to avoiding graft-versus-host disease (GVHD) in stem cell transplants. New ways of typing and matching HLA have made it easier to find the right donor. This lowers the risk of GVHD and improves transplant success.
- High-resolution HLA typing
- Improved donor selection criteria
- Enhanced GVHD prophylaxis strategies
Post-Transplant Care Innovations
Post-transplant care has gotten a lot better, focusing on preventing problems and treating them early. New ideas include better ways to prevent infections, managing GVHD, and improving supportive care.
| Innovation | Description | Benefit |
| Advanced Infection Prophylaxis | Use of antimicrobial agents to prevent infections | Reduced risk of life-threatening infections |
| GVHD Management | Early detection and treatment of GVHD | Improved graft survival and reduced GVHD severity |
| Supportive Care | Comprehensive care including nutritional support and psychological counseling | Enhanced quality of life and recovery |
Future Directions in Transplant Medicine
The future of transplant medicine looks bright, with new technologies like gene editing, better immunosuppression, and personalized medicine on the horizon.
Emerging trends include CAR-T cell therapy and other immunotherapies. These could make transplants even safer and more effective.
FAQ
How do stem cell transplants affect fertility?
Stem cell transplants can impact fertility. Patients should discuss fertility preservation options with their healthcare team before undergoing treatment.
Can stem cell transplants cure certain medical conditions?
Stem cell transplants can cure some medical conditions. These include certain blood cancers. The outcome depends on individual factors and the specific disease being treated.
What is the mortality rate associated with stem cell transplants?
The mortality rate varies based on several factors. These include the underlying disease, age, and overall health. Treatment-related mortality has decreased over time due to advances in transplant medicine.
What advances have improved the safety of stem cell transplants?
Advances include reduced-intensity conditioning regimens and improved HLA matching techniques. Post-transplant care innovations have also improved safety and outcomes.
What are the psychological and emotional challenges faced by patients undergoing stem cell transplants?
Patients may face emotional challenges, anxiety, and depression. Support systems, resources, and coping strategies are important.
How do allogeneic and autologous stem cell transplants compare in terms of risks?
Allogeneic transplants have a higher risk of GVHD and complications. Autologous transplants have a lower risk of GVHD but may have a higher risk of disease relapse.
What is the survival rate after a stem cell transplant?
The survival rate depends on several factors. These include the underlying disease, age, and overall health. Advances in transplant medicine have improved survival rates over time.
How long does it take to recover from a stem cell transplant?
The recovery time varies. Patients usually spend several weeks in the hospital. The recovery period can last several months to a year or more.
What are the short-term and long-term side effects of stem cell transplants?
Short-term side effects include infection, bleeding, and organ damage. Long-term side effects include chronic health issues, secondary cancers, fertility concerns, and quality of life considerations.
What is the risk of graft-versus-host disease (GVHD) in stem cell transplants?
GVHD is a risk in allogeneic transplants. It happens when the donor’s immune cells attack the recipient’s tissues. The risk depends on donor matching and immunosuppression.
What medical conditions require stem cell transplants?
Stem cell transplants treat various conditions. These include blood cancers, solid tumors, non-cancerous blood disorders, and immune deficiency disorders.
What are the different types of stem cell transplants?
There are several types. Autologous uses the patient’s own stem cells. Allogeneic uses stem cells from a donor. Syngeneic uses stem cells from an identical twin. Haploidentical uses stem cells from a half-matched donor.
What is a stem cell transplant, and how serious is it?
A stem cell transplant replaces damaged or diseased stem cells with healthy ones. It’s a serious treatment with risks and benefits to consider.