Last Updated on November 26, 2025 by Bilal Hasdemir

Major abdominal surgery is a big medical procedure. It happens inside the belly. It’s when doctors do surgery without touching the chest, like removing parts of the gut or organs. Discover what is considered major abdominal surgery. Learn the key criteria and how these critical procedures might differ for women.
For women, these surgeries can be different. This is because they might affect the reproductive system. At Liv Hospital, they focus on the patient. They make sure even the toughest abdominal surgeries are done with great care.
Key Takeaways
- Major abdominal surgery involves intra-peritoneal operations without primary thoracic involvement.
- Procedures include luminal resection or removal of solid organs associated with the GI tract.
- Women may face unique considerations, especially when reproductive organs are involved.
- Liv Hospital provides a patient-centered approach for complex abdominal surgeries.
- Understanding the distinction between major and minor procedures is key to making informed choices.
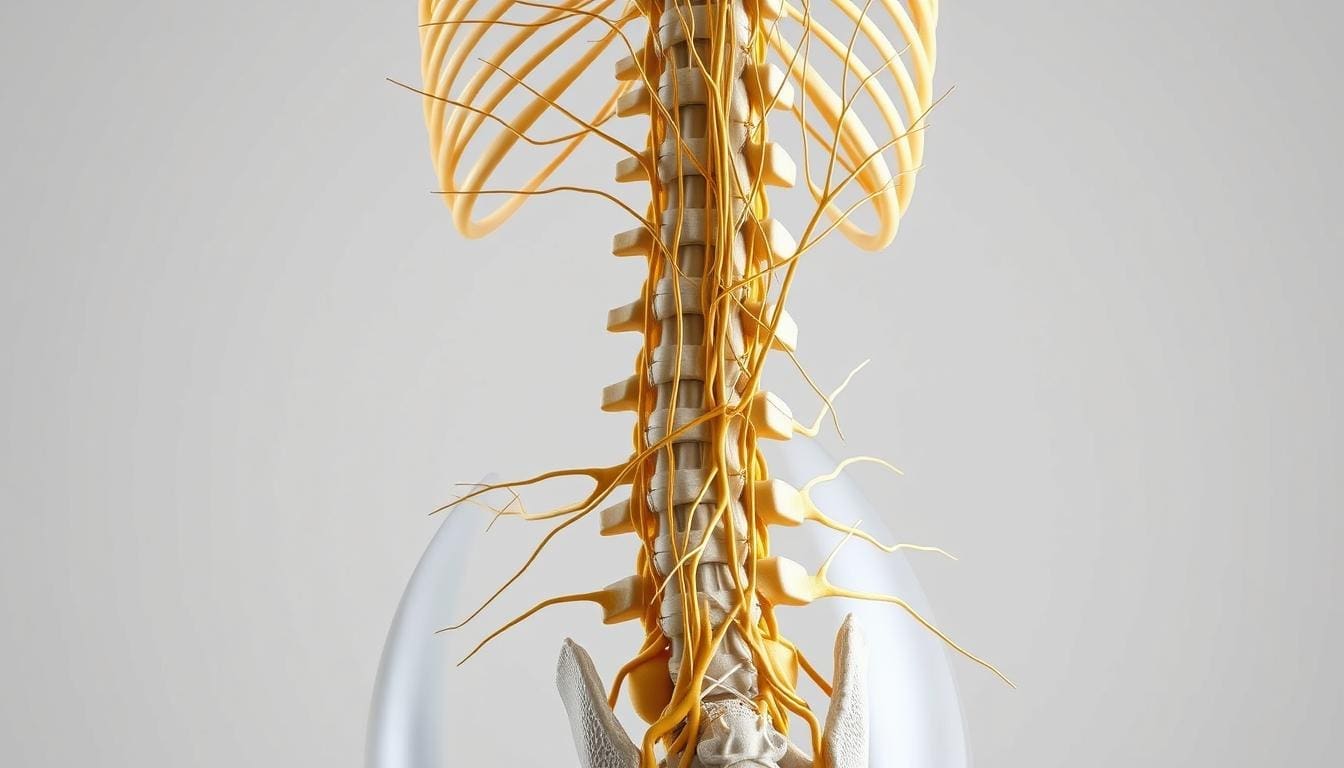
Defining Major Abdominal Surgery

Major abdominal surgery is a complex procedure with big incisions and long recovery times. It’s a big deal for patient care.
These surgeries are risky and take a long time to recover from. Knowing this helps doctors and patients prepare better.
Clinical Definition and Scope
Major abdominal surgery includes many procedures in the abdomen. It can involve the stomach, intestines, liver, and pancreas.
These surgeries are varied, using different methods for each case. About 5 million older adults will have major surgery in the next five years, with a 13.8% chance.
Distinction Between Major and Minor Procedures
Major surgeries have big incisions, long recovery times, and more risks. Minor procedures are simpler, with quicker recovery and less risk.
Knowing the difference helps patients prepare better for surgery. It’s key to understanding what to expect.
| Characteristics | Major Abdominal Surgery | Minor Surgical Procedures |
| Complexity | High | Low |
| Recovery Time | Lengthy | Short |
| Risk of Complications | Higher | Lower |
Impact on Patient Care and Recovery
Major abdominal surgery affects patient care and recovery a lot. Patients need thorough preparation and care after surgery to avoid problems and recover well.
Doctors can improve care by understanding the surgery’s impact. This helps patients get better and reduces risks.
What Is Considered Major Abdominal Surgery: Standard Classification

Doctors and patients need to know about major abdominal surgery. This type of surgery is complex and treats many abdominal issues.
Intra-peritoneal Operations Without Thoracic Involvement
Intra-peritoneal operations are a big part of major abdominal surgery. They happen inside the peritoneal cavity, where important organs like the stomach and liver are. Examples include exploratory laparotomy and intra-peritoneal lavage.
Luminal Resection Procedures of the GI Tract
Luminal resection procedures deal with the GI tract. They are key to treating diseases like colorectal cancer. Procedures such as colectomy and gastrectomy are major because they affect digestion.
Solid Organ Removal (Liver, Pancreas, Spleen)
Surgeries to remove organs like the liver or pancreas are complex. They are done for diseases or cancer. For example, a pancreatectomy removes part or all of the pancreas.
Understanding major abdominal surgery is key. It includes intra-peritoneal operations, GI tract surgeries, and organ removal. Each is complex and needs a lot of skill and care after surgery.
Common Types of Major Abdominal Surgeries
There are many types of major abdominal surgeries. Each one is for a different health issue in the abdominal area. These surgeries help fix problems with organs inside the belly.
Gastrointestinal Tract Procedures
Gastrointestinal tract procedures are very common. They include:
- Colectomy: This is when part or all of the colon is removed. It’s often for colon cancer or severe diverticulitis.
- Gastrectomy: This surgery removes part or all of the stomach. It’s usually for stomach cancer or severe gastric ulcers.
These surgeries are big deals. They need a lot of planning before and after to make sure they go well.
Hepatobiliary and Pancreatic Surgeries
Hepatobiliary and pancreatic surgeries deal with the liver, bile ducts, and pancreas. These complex surgeries include:
- Hepatectomy: This is when part of the liver is removed. It’s often for liver tumors.
- Pancreatectomy: This surgery removes part or all of the pancreas. It’s for pancreatic cancer or chronic pancreatitis.
These surgeries need a very skilled team because they’re so complex.
Urological Abdominal Operations
Urological abdominal operations are for the urinary tract organs in the abdomen. Examples are:
- Nephrectomy: This is when a kidney is removed. It’s often for kidney cancer or severe kidney damage.
- Cystectomy: This surgery removes the bladder. It’s usually for bladder cancer.
These surgeries are key to treating many urological problems. They need very precise techniques.
Female-Specific Major Abdominal Surgeries
Major abdominal surgery for women includes operations on the female reproductive system. These surgeries treat various gynecological issues, from benign to cancerous conditions.
Hysterectomy and Its Variations
Hysterectomy, the removal of the uterus, is common among women. It comes in different types, like total, subtotal, and radical hysterectomy. The choice depends on the condition, such as fibroids or cancer.
A total hysterectomy removes the whole uterus and cervix. It’s often for uterine cancer or severe fibroids. Subtotal hysterectomy keeps the cervix, removing the uterus’s top part. Radical hysterectomy removes more, including the cervix, vagina, and tissues, for cervical cancer.
Oophorectomy and Ovarian Procedures
Oophorectomy removes one or both ovaries. It’s done alone or with a hysterectomy. The decision is based on cysts, cancer, or other issues.
There are laparoscopic and open surgery options for oophorectomy. The choice depends on the patient’s condition and the surgeon’s advice. Younger women might choose to keep their ovaries to preserve hormones and fertility.
Surgeries for Gynecological Cancers
Major surgeries treat gynecological cancers like cervical, ovarian, and uterine. They remove the cancerous organ(s) and surrounding tissues and lymph nodes. The extent depends on the cancer’s stage and type.
Surgery might be combined with chemotherapy and radiation for better results. The surgical method can be minimally invasive or open surgery.
Anatomical and Physiological Differences in Women
Major abdominal surgery in women works best when we understand their unique body differences. These differences can change how well surgery goes and how fast they recover.
Pelvic Anatomy and Surgical Implications
The women’s pelvic area is more complex and different from men’s. This affects how surgeons do surgery. Knowing these differences is key for surgeons to perform major abdominal surgeries well.
Hormonal Influences on Surgical Outcomes
Hormones in women can change how they heal and recover from surgery. For example, estrogen affects how tissues heal. Surgeons need to think about these hormonal changes when planning surgery.
- Hormonal changes can impact wound healing.
- Estrogen levels may influence the risk of certain complications.
- Hormonal fluctuations can affect recovery times.
Reproductive System Considerations
The reproductive system in women makes surgery more complex. Surgeons must think about how surgery might affect fertility, menstrual cycles, and reproductive health. They aim to do effective surgery while trying to keep reproductive functions intact.
Surgical Approaches and Techniques
Surgical methods for major abdominal surgery have changed. Now, women have many options that fit their needs and health. The right surgical method is key to a smooth recovery and good results.
Open Surgery vs. Minimally Invasive Techniques
Major surgeries can be done in two ways: open surgery or minimally invasive surgery. Surgery Open surgery uses a big cut to get into the belly. Minimally invasive surgery uses small cuts, a camera, and special tools.
Minimally invasive surgery is popular because it hurts less, you stay in the hospital less, and you get better faster. But it’s not right for everyone. It depends on your health, the surgery, and the doctor’s skills.
| Surgical Technique | Benefits | Limitations |
| Open Surgery | Direct access, suitable for complex cases | Larger incision, longer recovery |
| Minimally Invasive Surgery | Smaller incisions, less pain, quicker recovery | Limited visibility requires specialized training |
| Robotic-Assisted Surgery | Enhanced precision, improved visualization | High cost, limited availability |
Robotic-Assisted Procedures for Women
Robotic surgery is a big step forward. It gives doctors better control and a view. For women, it’s great for surgeries in the reproductive area.
Robotic systems help with precise cuts and stitching. This might lower risks and improve results. But it’s expensive and not everywhere.
Gender-Specific Technical Adaptations
Surgeons can tailor techniques for women’s unique anatomy and health. For example, surgeries in the female reproductive system need to know the pelvic area.
Doctors use special methods to protect tissues and get the best results. These custom approaches are key to the right care for women’s health.
Preoperative Preparation and Assessment
Preparation before major abdominal surgery is key. It needs a special plan for women, focusing on their unique needs.
General Preparation Guidelines
Good prep starts with checking the patient’s health. This includes looking at their medical history, doing a physical exam, and running lab tests. Getting the patient ready before surgery helps avoid risks and makes recovery easier.
Here are some steps to follow:
- Check if the patient is getting enough nutrients
- Look at their heart health
- Test their lung function
- Check how well their blood clots
A study in the Journal of the American College of Surgeons says, “Making sure patients are healthy before surgery can lower complications.”
“Preoperative optimization of modifiable risk factors can significantly reduce postoperative complications.”
Journal of the American College of Surgeons
Women-Specific Preoperative Considerations
Women need special care before major surgery. This includes checking their menstrual cycle and reproductive health. It also means talking about how surgery might affect their fertility.
A study in the American Journal of Obstetrics and Gynecology stresses the need to think about reproductive health for women before surgery.
Reproductive Status and Fertility Preservation Options
Talking about fertility is important for women of childbearing age. They should know how surgery might affect their ability to have children. They might also want to explore ways to save their fertility, like freezing eggs or preserving ovarian tissue.
| Fertility Preservation Option | Description | Considerations |
| Egg Freezing | Cryopreservation of eggs for future use | Requires ovarian stimulation and egg retrieval |
| Ovarian Tissue Preservation | Freezing of ovarian tissue for possible future use | Good for prepubertal girls or when time is short |
In summary, getting ready for major surgery in women needs a detailed plan. It must cover their overall health and their reproductive and fertility concerns.
Recovery and Postoperative Care Differences
Women facing major abdominal surgery often face unique recovery challenges. These challenges need special postoperative care. The recovery process is shaped by many factors, like the surgery type, the patient’s health, and gender-specific considerations.
Standard Recovery Protocols
Standard recovery plans for major abdominal surgery include pain management and monitoring for complications. Effective pain management is key and may involve various medications and techniques. Patients are also watched for signs of infection, bleeding, or other issues during recovery.
Postoperative care instructions cover wound care, dietary advice, and activity levels. Patients learn how to care for their wounds and watch for signs. They also get guidance on gradually returning to normal activities.
Female-Specific Recovery Challenges
Women may face special recovery challenges after major abdominal surgery, including hormonal fluctuations and reproductive health impacts. The surgery can alter hormonal balances, which is important to understand for recovery support.
Women may also deal with emotional challenges like anxiety or depression during recovery. Emotional support from healthcare providers, family, and friends is critical for helping women manage these feelings.
Hormonal and Reproductive Considerations
Hormonal changes after major abdominal surgery can significantly affect women’s recovery. For example, surgeries removing the ovaries can cause sudden menopause, needing careful hormone replacement therapy (HRT) management. Healthcare providers must consider these hormonal changes when planning postoperative care.
Reproductive considerations are also key for women of childbearing age. Surgeries affecting reproductive organs can impact fertility. Discussing fertility preservation options should be part of both preoperative and postoperative care.
Potential Complications and Risk Factors
Surgeons and patients need to know about the risks of major abdominal surgery. This is true, given the special needs of women’s bodies.
Universal Complications of Major Abdominal Surgery
Major abdominal surgery can lead to several common problems. These include infections, bleeding, and reactions to anesthesia. Also, there can be issues with breathing or the heart. A good plan before and after surgery can help manage these risks.
Common Complications:
- Infection
- Bleeding or hemorrhage
- Adverse reactions to anesthesia
- Respiratory complications
- Cardiac issues
Female-Specific Complications and Risks
Women may face extra risks during major abdominal surgery. These can include problems with hysterectomy, oophorectomy, or surgeries for gynecological cancers. Knowing these risks helps doctors give better care.
| Complication | Description | Mitigation Strategy |
| Adhesions | Tissue adhesions can occur, potentially leading to bowel obstruction. | Minimally invasive techniques, careful handling of tissues. |
| Hormonal Changes | Surgeries like oophorectomy can lead to significant hormonal changes. | Hormone replacement therapy (HRT), careful patient selection. |
Evidence-Based Risk Mitigation Strategies
Using proven strategies is key to reducing surgery risks. This includes making sure patients are healthy before surgery, using less invasive methods, and following ERAS protocols.
“The implementation of ERAS protocols has been shown to significantly reduce complications and improve recovery times in patients undergoing major abdominal surgery.”
– Journal of Surgical Research
By knowing the risks and using proven ways to reduce them, doctors can help patients have better outcomes from major abdominal surgery.
Conclusion: Advancing Gender-Specific Approaches to Major Abdominal Surgery
The field of surgery is growing, and gender-specific methods are key for better results in major abdominal surgery, mainly for women. New surgical techniques and understanding female patients’ unique needs are leading this change.
Studies reveal that women’s bodies react differently to surgery, and recovery is influenced by hormones. Healthcare teams can now tailor care to meet women’s specific needs during major abdominal surgery.
Gender-specific care goes beyond surgery techniques. It also includes better pre-op prep, post-op care, and managing complications. This approach helps healthcare providers improve care and lower the risk of bad outcomes.
To move forward, we need more research, education, and training. By focusing on these areas, we can make sure women get the best care and achieve the best results.
FAQ
What is considered major abdominal surgery?
Major abdominal surgery includes complex procedures with big cuts. These surgeries often take a long time to recover from. They involve the stomach, liver, pancreas, and other organs.
How does major abdominal surgery differ for women?
Women face special challenges in major abdominal surgery. This is because surgeries on reproductive organs, like the uterus and ovaries, affect their health greatly.
What are the different types of major abdominal surgeries?
There are many types of major abdominal surgeries. These include operations on the stomach, liver, and pancreas. There are also surgeries for the urinary system and specific ones for women, like hysterectomy and oophorectomy.
What is the distinction between major and minor abdominal surgery?
Major surgeries are more complex and risky. They also take longer to recover from than minor surgeries.
What are the risks associated with major abdominal surgery?
Major surgeries carry risks like infection and bleeding. There are also risks related to anesthesia. Women face additional risks due to hormonal and reproductive health.
How do anatomical and physiological differences in women affect major abdominal surgery?
Surgeons must understand the female body to perform surgeries well. This includes the pelvic area, hormones, and reproductive system.
What are the preoperative considerations specific to women undergoing major abdominal surgery?
Women need special attention before surgery. This includes their reproductive status and options for preserving fertility. It also involves addressing their hormonal and reproductive health.
How do recovery and postoperative care differ for women after major abdominal surgery?
Women face unique challenges during recovery. This includes dealing with hormonal and reproductive health issues, in addition to standard care.
What are the evidence-based strategies to mitigate risks in major abdominal surgery?
To reduce risks, careful planning and precise surgery are key. Postoperative care must also be tailored to each patient, including gender-specific needs.
What is the significance of gender-specific approaches to major abdominal surgery?
Gender-specific care is vital for better patient outcomes. It addresses the unique needs of women in major abdominal surgery