Nearly 40% of adults in the United States are vitamin D-deficient, highlighting the importance of understanding what does vitamin D do in our health.
Vitamin D activation is a complex process that turns vitamin D into its active form, calcitriol, primarily through the liver and kidneys, which play key roles in vitamin D metabolism and synthesis essential for bone health and immune function.
Key Takeaways
- The liver and kidneys are critical for vitamin D activation.
- Vitamin D is essential for bone health and immune function.
- A deficiency in vitamin D can lead to various health issues.
- Understanding vitamin D metabolism is vital for appreciating its role in the body.
- Vitamin D synthesis involves multiple steps and organs.
The Sunshine Vitamin: An Overview
The term “sunshine vitamin” refers to vitamin D. It is made in the skin when we get sunlight. Vitamin D is important for strong bones and overall health.
The Molecular Structure of Vitamin D
Vitamin D’s molecular structure is key to its function. It’s a secosteroid, a special type of steroid. Its unique structure lets it work with specific receptors in our bodies.
This helps it do its job. Knowing the molecular structure of vitamin D helps us understand its role in health and disease.
Different Forms: Vitamin D2 vs. D3
Vitamin D comes in two main types: Vitamin D2 (ergocalciferol) and Vitamin D3 (cholecalciferol). Vitamin D3 is more important for humans. It’s made in our skin when we get sunlight.
Vitamin D2 comes from fungi and fortified foods. Both types need to be activated to work in our bodies.
What Does Vitamin D Do in the Human Body?
Vitamin D is vital for our bodies. It helps with bone health and our immune system. Knowing its role helps us see why it’s key for our health.
Primary Functions and Benefits
Vitamin D keeps our bones strong by controlling calcium levels. It helps bones grow and stay dense, which is good for our skeletons. It also boosts our immune system, which may lower the risk of some diseases.
Vitamin D does more than just help bones. It can also lower the risk of heart disease and some cancers. It might even help with mood and brain function.
Vitamin D’s Role in Calcium Homeostasis
Vitamin D is key in keeping calcium levels right in our bodies. It helps our gut absorb calcium better. This ensures we have enough calcium for our muscles and nerves.
Without enough vitamin D, our bodies can’t absorb calcium well. This can lead to weak bones or other health issues.
Sources of Vitamin D: Natural and Supplemental

To keep vitamin D levels right, knowing where it comes from is key. Vitamin D can be found in both natural and supplement forms.
The skin makes vitamin D when it’s exposed to sunlight. How much vitamin D is made depends on skin color, age, and the time of day.
Sunlight Exposure and Cutaneous Synthesis
Sunlight makes vitamin D in the skin. The amount made changes with the strength of UVB rays. Peak synthesis happens when the sun is high in the sky, between 10 am and 4 pm.
Dietary Sources and Supplements
Vitamin D also comes from food and supplements. Fatty fish like salmon and fortified dairy products are good sources. Vitamin D supplements come in D2 and D3 forms, with D3 being more effective.
It’s important to know how to balance these sources. This is true for people who don’t get much sun or are at risk of not having enough vitamin D.
The Vitamin D Activation Pathway: A Multi-Organ Process
The process of activating vitamin D involves several organs working together. It starts in the skin and moves through the liver and kidneys. This journey ends with the creation of calcitriol, the active form of vitamin D.
From Cholesterol to Pre-Vitamin D in the Skin
The journey of vitamin D starts with cholesterol in the skin. Here, it turns into pre-vitamin D when exposed to UVB rays from the sun. This pre-vitamin D quickly becomes vitamin D3 (cholecalciferol).
Min D depends on skin color, age, and how much skin is exposed.
Vitamin D3 then goes to the liver for the first step of its activation. This step is key to the activation of vitamin D in the kidneys.
The Two-Step Activation Process
The activation of vitamin D is a two-step hydroxylation process. The first step happens in the liver, where vitamin D becomes 25-hydroxyvitamin D (calcidiol). This is done by the enzyme vitamin D 25-hydroxylase.
The second step is in the kidneys, where calcidiol is turned into 1,25-dihydroxyvitamin D (calcitriol). This is done by the enzyme 1α-hydroxylase. Calcitriol is the active form of vitamin D.
This two-step process is vital for controlling calcium levels and bone health. Knowing how vitamin D is activated helps us see its role in keeping bones strong and overall health.
The Liver: First Critical Organ in Vitamin D Activation
The liver is key in making vitamin D active. This nutrient is vital for strong bones and a healthy immune system. It gets activated in the liver after being obtained from food, supplements, or sunlight.
Hepatic Hydroxylation of Vitamin D
The liver starts vitamin D’s activation by adding a hydroxyl group. This makes 25-hydroxyvitamin D a necessary step for further activation. The enzyme CYP2R1, mainly found in the liver, does this conversion.
This initial step is vital. It ensures vitamin D can be used by the body. It shows how important the liver is for vitamin D and overall health.
Production of 25-hydroxyvitamin D (Calcidiol)
The liver’s work results in 25-hydroxyvitamin D, or calcidiol. This is a key indicator of vitamin D levels in the body. The liver’s role in creating 25-hydroxyvitamin D is a critical part of vitamin D’s activation journey.
Knowing the liver’s role in vitamin D production is key. It helps us understand the complex process of vitamin D activation. This is important for keeping bones strong and the immune system healthy.
The Kidneys: Second Critical Organ for Complete Activation
The kidneys are key in the final step of vitamin D activation. They take the vitamin D from the liver and make it active.
This step is vital for vitamin D’s functions, like absorbing calcium and keeping bones healthy. The kidneys use the enzyme renal 1α-hydroxylase to turn 25-hydroxyvitamin D into 1,25-dihydroxyvitamin D (calcitriol).
Renal 1α-Hydroxylase Enzyme Function
The renal 1α-hydroxylase enzyme is responsible for changing 25-hydroxyvitamin D into calcitriol. It’s controlled by parathyroid hormone (PTH) and the body’s calcium needs.
Renal 1α-hydroxylase activity is a critical control point in vitamin D metabolism, ensuring the active form of vitamin D is made as needed.
Conversion to 1,25-dihydroxyvitamin D (Calcitriol)
The kidneys convert 25-hydroxyvitamin D to 1,25-dihydroxyvitamin D (calcitriol) in the final step. Calcitriol is the active form of vitamin D. It works on tissues like the intestine, bone, and kidney to manage calcium and phosphate.
This shows how important kidney function is for vitamin D and bone health. If the kidneys don’t work properly, vitamin D activation can be off, leading to bone diseases.
Biochemical Mechanisms of Vitamin D Activation
Understanding how vitamin D is activated is key to its health benefits. This process involves several steps and specific enzymes and factors.
Key Enzymes in the Activation Process
The first step in vitamin D activation occurs in the liver. Here, 25-hydroxylase turns vitamin D into 25-hydroxyvitamin D (calcidiol). The second step happens in the kidneys, where 1α-hydroxylase converts calcidiol into 1,25-dihydroxyvitamin D (calcitriol). These enzymes are vital for vitamin D’s activation.
Regulatory Factors Controlling Activation
Vitamin D’s activation is controlled by several factors. Parathyroid hormone (PTH) and calcium levels are among them. When calcium is low, PTH helps make more calcitriol. This keeps calcium levels balanced and supports bone health.
Fibroblast growth factor 23 (FGF23) also plays a role. It helps control how much 1α-hydroxylase is made in the kidneys. This ensures vitamin D is activated just right for the body’s needs.
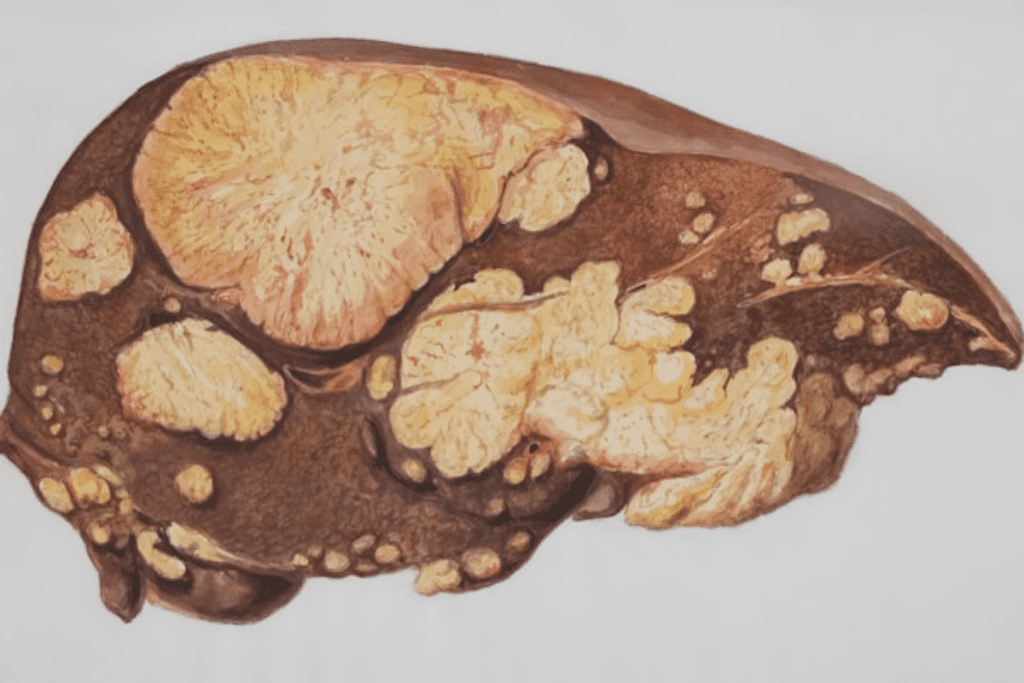
When Activation Fails: Liver Disorders and Vitamin D
Liver disorders can greatly affect how the body uses vitamin D. The liver is key in turning vitamin D into its active form, 25-hydroxyvitamin D.
Impact of Hepatic Diseases on Vitamin D Metabolism
Hepatic diseases can make it hard for the liver to turn vitamin D into its active form. This can lead to lower levels of 25-hydroxyvitamin D, which shows how much vitamin D is in the body.
Liver dysfunction can also mess with how vitamin D is bound in the body. It’s important to understand this to help manage vitamin D levels in people with liver problems.
Clinical Implications and Management Strategies
Impaired vitamin D activation in liver disorders has big implications. People with chronic liver diseases often have low vitamin D levels. This can make bone diseases worse and might even make liver problems worse.
To manage this, doctors should keep an eye on 25-hydroxyvitamin D levels in these patients. They might need to give vitamin D supplements. But how well supplements work depends on how bad the liver disease is. Personalized care and monitoring are essential for managing vitamin D levels in these patients.
Kidney Function and Vitamin D Activation Disorders
Kidney function is key for vitamin D activation, important for bone and immune health. The kidneys convert 25-hydroxyvitamin D into 1,25-dihydroxyvitamin D, the active form. This step is vital for calcium balance and overall body function.
Chronic Kidney Disease and Vitamin D Deficiency
Chronic kidney disease (CKD) hampers vitamin D activation due to kidney issues. This can cause vitamin D deficiency, worsening bone problems, and affecting other areas. In CKD, the kidneys can’t convert 25-hydroxyvitamin D to 1,25-dihydroxyvitamin D well. This leads to a deficiency, causing secondary hyperparathyroidism and bone disease.
Treatment Approaches for Impaired Renal Activation
For CKD, treatments include vitamin D supplements and active vitamin D analogs. It’s also important to watch calcium levels to avoid problems. Some main strategies are:
- Vitamin D supplementation
- Use of active vitamin D analogs
- Monitoring of calcium levels
The aim of these treatments is to fix vitamin D levels, protect bones, and stop CKD complications. Effective management of vitamin D disorders in CKD needs a full plan, including supplements and monitoring.
Extra-Renal Vitamin D Activation: Beyond the Kidneys
Vitamin D activation is not just a job for the kidneys. It also affects local tissue health and immune function. The kidneys make 1,25-dihydroxyvitamin D (calcitriol), but other tissues can activate vitamin D too.
Local Tissue Activation of Vitamin D
The skin, immune cells, and some organs can activate vitamin D. This local activation helps nearby cells. It improves local immune responses and tissue health.
For example, immune cells like macrophages and dendritic cells can make 1,25-dihydroxyvitamin D. This boosts their fight against infections. A study found, “The local production of 1,25-dihydroxyvitamin D in immune cells can significantly impact the body’s response to pathogens.”
Implications for Immune Function and Disease
Local vitamin D activation is key for immune function and disease prevention. It affects genes involved in immune response and cell growth.
A researcher noted, “Extra-renal vitamin D activation is vital for local immune homeostasis and preventing autoimmune diseases.” This shows why vitamin D is important for health and disease prevention.
In summary, extra-renal vitamin D activation is essential for local tissue health and immune function. It opens up new ways to treat diseases linked to vitamin D deficiency.
Factors Affecting Vitamin D Activation Efficiency
Many things can change how well vitamin D works in our bodies. This includes things we can’t control, like our genes and the environment. Knowing about these factors helps us keep our vitamin D levels right.
Age, Genetics, and Environmental Influences
Getting older affects how well our skin makes vitamin D from sunlight. Our genes also play a big part. Some people’s genes make it harder for their bodies to use vitamin D.
- Age-related decline in cutaneous synthesis
- Genetic variations affecting the vitamin D binding protein
- Environmental factors like UV radiation and diet
Medications That Alter Vitamin D Metabolism
Some medicines can change how our bodies use vitamin D. This includes drugs for seizures, steroids, and some HIV treatments.
- Anticonvulsants: Phenobarbital and phenytoin
- Glucocorticoids: Prednisone and other corticosteroids
- Antiretroviral drugs: Certain HIV medications
Doctors can help manage vitamin D levels better. This is important for people who are older, have certain genes, or take certain medicines.
Testing Vitamin D Status: What Blood Tests Reveal
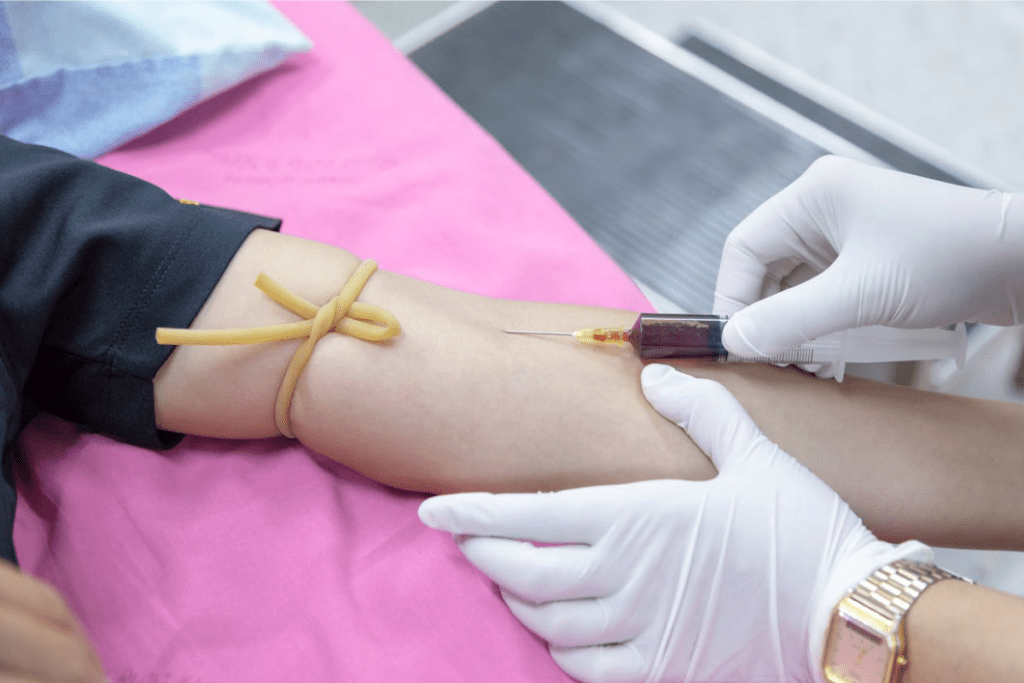
Vitamin D status can be accurately assessed through specific blood tests. These tests are key to understanding an individual’s vitamin D levels. They help guide the right health interventions.
Measuring 25-hydroxyvitamin D vs. 1,25-dihydroxyvitamin D
There are two main forms of vitamin D measured in the blood: 25-hydroxyvitamin D and 1,25-dihydroxyvitamin D. The 25-hydroxyvitamin D test is the most common. It shows both dietary intake and skin synthesis.
In contrast, 1,25-dihydroxyvitamin D is the active form. But its levels can change due to parathyroid hormone and calcium levels.
Interpreting Test Results and Optimal Levels
Understanding vitamin D test results is important. It involves knowing the different units and optimal levels. A 25-hydroxyvitamin D level between 20-40 ng/mL is generally adequate.
Levels below 12 ng/mL show deficiency. But optimal levels can vary. This depends on age, health status, and sunlight exposure.
Healthcare providers consider these factors. They use them to interpret test results. They then suggest the right supplements or other treatments.
Vitamin D Supplementation Strategies
Vitamin D supplements need to be tailored for each person. This includes looking at organ function and the type of supplement. Knowing these details helps fix deficiencies and boost health.
Dosage Recommendations Based on Organ Function
The right amount of vitamin D depends on organ health, like the liver and kidneys. These organs are key in making vitamin D work. For example, people with kidney disease might need different amounts.
Doctors should check organ health before suggesting vitamin D supplements. This step is important to find the right dose. It makes sure the supplement works well and is safe.
Different Forms of Vitamin D Supplements
Vitamin D supplements are mainly D2 (ergocalciferol) and D3 (cholecalciferol). Both can increase vitamin D levels, but D3 is often better for keeping levels steady over time. The choice between D2 and D3 depends on health needs and dietary choices.
Vitamin D Cofactors: Optimizing Activation
Vitamin D works better with certain nutrients that help it get activated. These nutrients are key for vitamin D to be used by the body.
Magnesium’s Essential Role in Vitamin D Metabolism
Magnesium is vital for vitamin D to become active. It helps in the steps that turn vitamin D into its active form. Studies show that not enough magnesium can mess up vitamin D’s work.
Magnesium’s role in vitamin D activation shows why we need to eat foods rich in magnesium or take supplements.
Vitamin K, Zinc, and Other Supporting Nutrients
Other nutrients like vitamin K and zinc also help with vitamin D. Vitamin K helps calcium go to bones and teeth. Zinc is important for many body processes, including vitamin D activation.
Ensuring adequate intake of these nutrients is key to better vitamin D activation and health.
Current Research on Vitamin D Activation
The study of vitamin D is moving fast, with new findings on how it works. As we learn more about vitamin D, we see its uses in treating diseases.
Emerging Understanding of Activation Pathways
New studies have shown how vitamin D gets activated. Vitamin D activation pathways are not just in the liver and kidneys. Many tissues can activate vitamin D, affecting cell function and disease.
Local activation of vitamin D is seen in tissues like the immune system. It helps control immune responses. This is key to understanding vitamin D’s role in health and disease.
Novel Therapeutic Approaches for Activation Disorders
Scientists are exploring novel therapeutic approaches for vitamin D-related disorders. For example, targeting enzymes in vitamin D metabolism could help treat vitamin D deficiency or insensitivity.
“The chance for vitamin D-based treatments to tackle many health problems is huge. Ongoing research will likely reveal new and creative ways to treat.”
As research digs deeper into vitamin D activation, we’re getting closer to effective treatments. Knowing how vitamin D works is key to using it to help people.
Conclusion: The Liver-Kidney Axis in Vitamin D Health
The liver and kidneys are key to vitamin D health. They work together to make vitamin D active. Knowing how they function is important for good vitamin D levels.
The liver starts vitamin D’s activation, and the kidneys finish it. This shows how important the liver-kidney axis is. Problems with these organs can affect vitamin D levels.
Understanding the connection between the liver, kidneys, and vitamin D helps us stay healthy. We can eat right, get enough sunlight, and use supplements when needed. This includes vitamin D, magnesium, and vitamin K.
In short, the liver, kidneys, and vitamin D are closely linked to health. By supporting this balance, we can keep our vitamin D levels right and avoid health issues.
FAQ
What is the role of vitamin D in the human body?
Vitamin D helps control calcium levels. It supports bone health and boosts the immune system.
How is vitamin D activated in the body?
Vitamin D gets activated in two steps. First, it’s changed in the liver to 25-hydroxyvitamin D. Then, in the kidneys, it becomes 1,25-dihydroxyvitamin D, or calcitriol.
Which organs are critical for vitamin D activation?
The liver and kidneys are key to vitamin D activation.
What is the difference between vitamin D2 and D3?
Vitamin D2 comes from fungi. Vitamin D3 is made in the skin when exposed to sunlight and is found in animal foods.
How can vitamin D deficiency be addressed?
To fix vitamin D deficiency, you can get more sunlight, eat foods rich in vitamin D, or take supplements. The right amount depends on your health and how well your organs work.
What are the cofactors that support vitamin D metabolism?
Magnesium, vitamin K, and zinc help vitamin D work right.
How does liver function impact vitamin D activation?
Liver problems can stop vitamin D from being activated. This can lead to a deficiency. It’s important to understand how liver diseases affect vitamin D.
What is the impact of chronic kidney disease on vitamin D activation?
Chronic kidney disease can cause vitamin D deficiency because the kidneys can’t activate it. Knowing how to treat this is key to managing related health issues.
How is vitamin D status tested?
Vitamin D levels are checked by measuring 25-hydroxyvitamin D. This shows how much vitamin D your body has.
What are the emerging areas of research on vitamin D activation?
Researchers are looking into new ways vitamin D is activated. They’re also exploring how it can help with certain diseases.
How does age affect vitamin D activation efficiency?
Older people might need more vitamin D because their bodies make less of it. This is because aging affects how well vitamin D is activated.
Can vitamin D be activated locally in tissues?
Yes, vitamin D can be activated in different tissues. This affects the immune system and might play a role in some diseases.
Reference
- Holick, M. F. (2017). Vitamin D deficiency. New England Journal of Medicine, 357(3), 266-281.https://doi.org/10.1056/NEJMra070553



































