Last Updated on November 26, 2025 by Bilal Hasdemir
We are seeing a big change in how we treat abdominal aortic aneurysms. Endovascular repair of abdominal aortic aneurysm is a new, less invasive way compared to old open surgery. It uses an abdominal aortic stent graft to block blood flow to the aneurysm. This helps lower the risk of the aorta bursting.
Studies show EVAR is now the top choice for most patients. It has a lower death rate in the first few months after surgery. The National Center for Biotechnology Information says EVAR greatly lowers the chance of the aorta bursting. It’s a key treatment for the right patients.
Key Takeaways
- EVAR is a minimally invasive alternative to traditional open surgical repair for abdominal aortic aneurysm.
- The procedure involves deploying an abdominal aortic stent graft to exclude the aneurysm from blood flow.
- EVAR has a lower short-term mortality rate compared to open surgical repair.
- The risk of rupture is significantly reduced with EVAR.
- EVAR is indicated for patients with suitable anatomy and reasonable life expectancy.
Understanding Abdominal Aortic Aneurysms
Abdominal aortic aneurysms (AAAs) are a serious health issue that needs to be understood well. An AAA happens when the aorta, the main blood vessel, gets too big. This is in the lower part of the aorta.
What Is an Abdominal Aortic Aneurysm?
An abdominal aortic aneurysm means the aorta gets bigger than 3 cm. It often doesn’t show symptoms, which makes it a hidden danger. If it bursts, it can be very dangerous.
Risk Factors and Prevalence
There are risk factors for getting AAAs. These include:
- Being older
- Smoking
- Having a family history of AAA
- Being a man
- Having other vascular diseases
AAAs get more common with age, mainly in men over 65. Knowing these risks helps find and manage them early.
Symptoms and Detection Methods
Most AAAs don’t show symptoms and are found by chance during tests. Symptoms might be:
- Pain in the abdomen or back
- A mass in the abdomen that can be felt
- Clots breaking loose and going to other parts of the body
Tests like ultrasound, CT scans, and MRI can find AAAs. Early detection is important to stop rupture and manage the condition well.
The Fundamentals of Endovascular Repair of Abdominal Aortic Aneurysm
EVAR, or endovascular aneurysm repair, is a new way to treat abdominal aortic aneurysms. It’s a less invasive method that uses a stent graft to fix the aneurysm from inside the aorta.
Definition and Basic Principles
EVAR is a procedure where a stent graft is put in through the femoral arteries. It seals off the aneurysm sac from blood flow. This stops it from getting bigger and bursting.
The main ideas behind EVAR are:
- It’s done through small cuts in the femoral arteries.
- A stent graft is used to block off the aneurysm.
- It keeps blood flowing to important organs.
Historical Development of EVAR
The idea of EVAR started in the early 1990s. It was a big step forward in treating abdominal aortic aneurysms. Over time, stent graft technology and imaging methods have gotten better.
Important milestones include:
- The first EVAR success.
- Improvements in stent graft design and materials.
- Better imaging for planning and checking up after the procedure.
Current State of Practice in the United States
Now, EVAR is a common choice for treating abdominal aortic aneurysms in the U.S. The current practice is marked by:
- Advanced stent graft technologies.
- More EVARs for both ruptured and unruptured aneurysms.
- Better choices for who gets EVAR, based on their body and health.
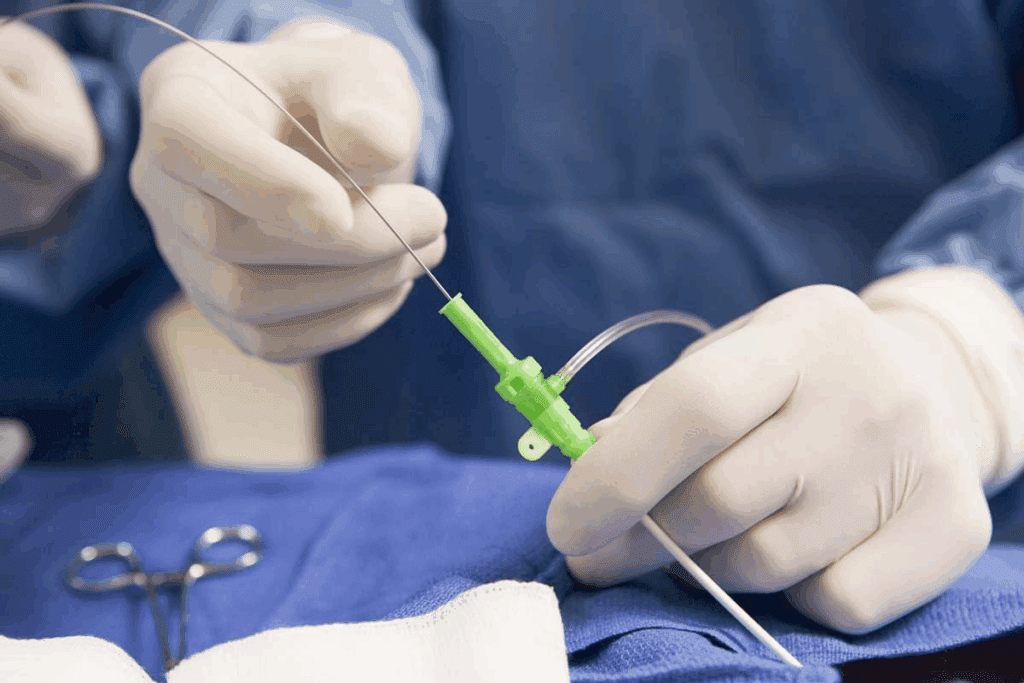
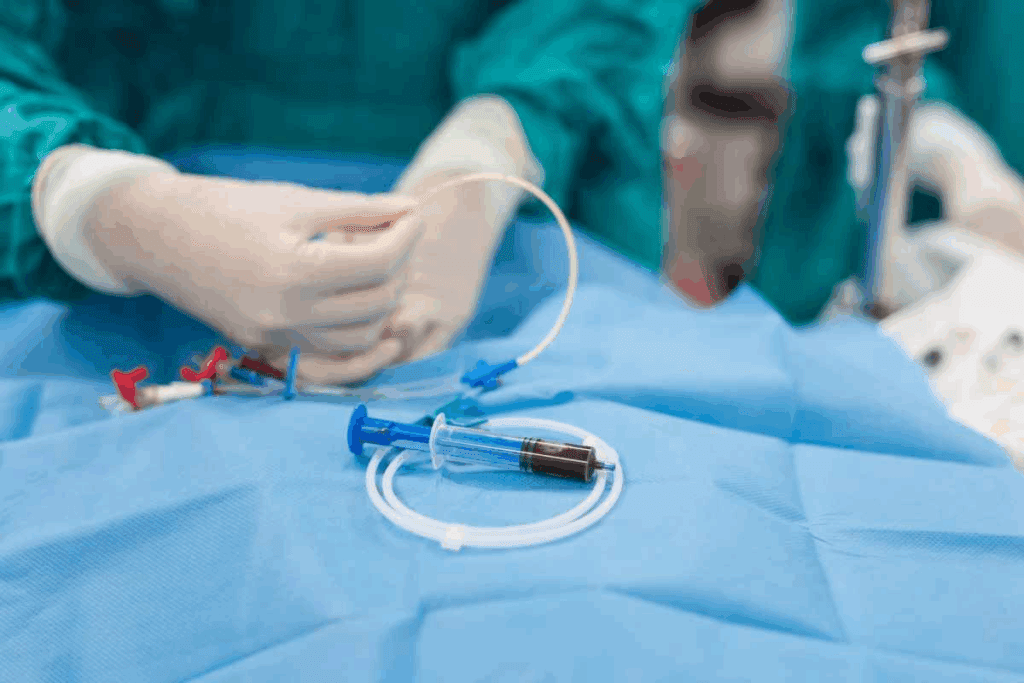
How Abdominal Aortic Stent Graft Procedures Work
The process of abdominal aortic stent grafting includes several key steps. It starts with planning and ends with the stent graft deployment. This method is a big step forward in treating abdominal aortic aneurysms (AAAs).
Pre-Procedure Planning and Imaging
Before starting the abdominal aortic stent graft procedure, detailed images are taken. These images help figure out the aneurysm’s size, shape, and location. This step is vital for picking the right stent graft size and type.
CT scans and angiography are used to get this information. They show the aneurysm’s details and the patient’s blood vessel layout. This info helps choose the best stent graft and plan the procedure.
Step-by-Step Procedure Overview
The stent graft procedure starts by accessing the femoral arteries in the groin. The stent graft is then guided to the aneurysm site using fluoroscopic imaging.
Once in place, the stent graft is deployed. This lets blood flow through it, bypassing the aneurysm. This action reduces pressure on the aneurysm wall, preventing it from growing or rupturing.
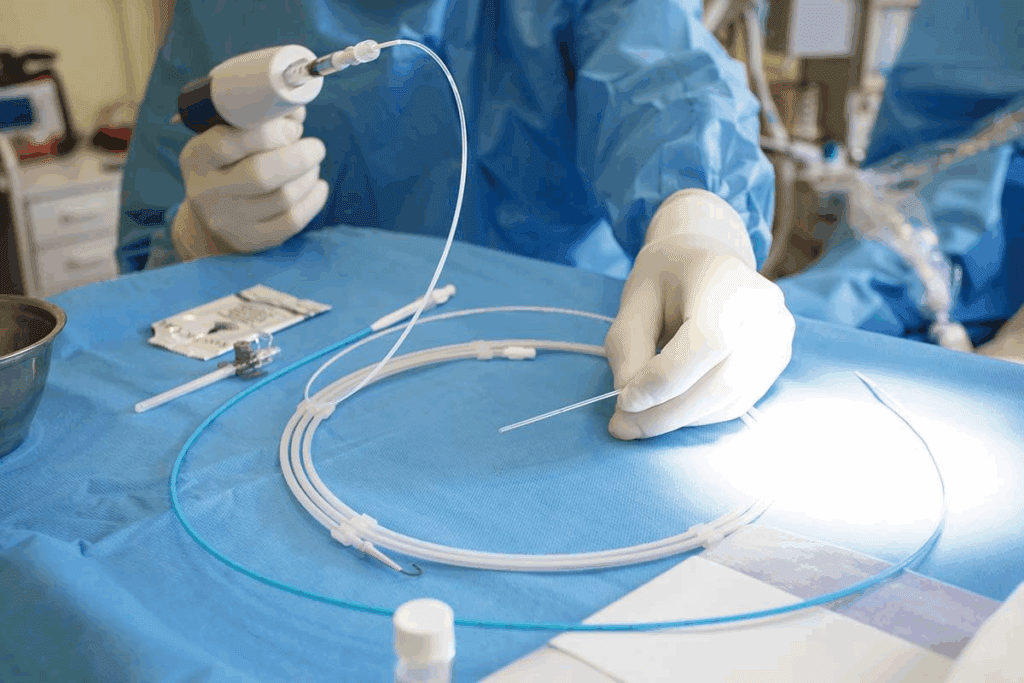
Types of Stent Grafts Used in AAA Repair
There are different stent grafts for AAA repair, like bifurcated, aorto-uni-iliac, and fenestrated ones. The right stent graft depends on the patient’s anatomy and the aneurysm’s specifics.
| Type of Stent Graft | Description | Indications |
| Bifurcated Stent Graft | Designed to accommodate the bifurcation of the aorta into the iliac arteries. | Suitable for most AAA patients with normal aortic bifurcation anatomy. |
| Aorto-Uni-Iliac Stent Graft | Used when there is a need to occlude one iliac artery or in cases of complex anatomy. | Indicated for patients with complex iliac artery anatomy or previous surgical interventions. |
| Fenestrated Stent Graft | Custom-made to include fenestrations that align with the patient’s visceral arteries. | Ideal for patients with aneurysms that involve major branch vessels. |
The endovascular repair of AAA using stent grafts has changed how we treat abdominal aortic aneurysms. It offers a less invasive option compared to traditional surgery. As technology gets better, we can look forward to even more improvements in stent graft design and results.
Comparing EVAR to Open Surgical Repair
EVAR and open surgical repair are two ways to treat abdominal aortic aneurysms. They differ in mortality rates, recovery times, and costs. It’s important for patients and doctors to understand these differences to make the best choice.
Mortality Rate Differences
Research shows EVAR has a lower death rate right after surgery compared to open repair. This is a big plus for those at high risk for surgery complications.
- EVAR: Lower perioperative mortality
- Open Repair: Higher perioperative mortality, mostly in high-risk patients
Recovery Time and Hospital Stay
EVAR leads to shorter hospital stays and quicker recovery times. This is because it’s a less invasive procedure.
Key benefits of EVAR include:
- Shorter hospital stay
- Faster recovery
- Less invasive
Long-Term Outcomes After 15 Years
Even though EVAR has short-term benefits, long-term survival rates are similar to open repair after 15 years. It’s important for EVAR patients to have ongoing monitoring for risks like endoleaks and graft migration.
Cost Considerations Between Approaches
The cost of EVAR versus open repair can differ a lot. EVAR might cost more upfront for the stent graft. But, it often leads to lower overall costs because of shorter hospital stays and less intensive care.
- Initial costs: EVAR may be higher due to device costs
- Overall costs: EVAR can be lower due to reduced hospital stay and care
In conclusion, choosing between EVAR and open surgical repair depends on many factors. These include the patient’s health, the aneurysm’s anatomy, and personal preferences. Both methods have their roles in treating abdominal aortic aneurysms.
Patient Selection: Who Is a Candidate for Endovascular AAA Repair?
To benefit from endovascular repair, patients must meet specific criteria. These criteria include their anatomical characteristics, medical history, and overall health. We carefully evaluate these factors to determine the most appropriate treatment approach for each individual.
Anatomical Requirements for Successful EVAR
The success of EVAR largely depends on the patient’s anatomical suitability. Key factors include:
- The size and shape of the abdominal aortic aneurysm
- The presence of sufficient aortic neck length and diameter
- The condition and accessibility of the iliac arteries
- The absence of significant calcification or thrombus in the aortic neck
Advanced imaging techniques, such as CT angiography, play a key role in assessing these anatomical factors.
Medical Risk Assessment Factors
We conduct a thorough medical risk assessment to identify patients who are likely to benefit from EVAR. This includes evaluating:
- Cardiac function and history of cardiovascular disease
- Pulmonary function and history of respiratory conditions
- Renal function and history of kidney disease
- Other comorbidities that may impact surgical risk
By carefully assessing these factors, we can determine whether EVAR or an alternative treatment approach is more suitable for the patient.
Age and Life Expectancy Considerations
Age and life expectancy are important considerations when evaluating a patient’s candidacy for EVAR. While EVAR is generally considered for patients with a life expectancy of at least 1-2 years, individual factors may influence this decision.
We take into account the patient’s overall health, the presence of comorbid conditions, and the procedure’s benefits and risks. This helps us make an informed decision.
Potential Complications of Abdominal Aortic Aneurysm Stenting
Endovascular repair of abdominal aortic aneurysms (EVAR) is a less invasive method. Yet, it comes with possible complications. It’s vital to grasp these issues to better care for our patients.
Immediate Procedural Complications
During EVAR, immediate issues can arise. These include bleeding or hematoma at the access site and arterial injury. Also, there’s a risk of embolization, where debris can travel to other parts of the body.
To lessen these risks, we focus on careful planning and precise technique. Our team works with patients to identify and reduce risks.
Endoleaks: Types and Management
Endoleaks are a major issue with EVAR. They happen when blood leaks into the aneurysm sac around the stent graft. There are different types, each needing its own management plan.
| Type | Description | Management |
| Type I | Leak at the attachment site | Additional stenting or open repair |
| Type II | Retrograde flow from branches | Observation or embolization |
| Type III | Leak through graft fabric or junctions | Additional stenting or graft replacement |
| Type IV | Porosity of graft material | Observation or additional stenting |
| Type V | Endotension without visible leak | Close surveillance or intervention |
Knowing the type of endoleak is key to choosing the right treatment. We closely monitor and manage any endoleaks that occur.
Long-Term Device-Related Issues
Long-term problems can include stent graft migration and device failure. These issues can be serious, sometimes requiring more surgery or even open repair.
We stress the importance of long-term follow-up and surveillance. Regular imaging helps catch issues early, allowing for timely action.
By understanding and tackling EVAR complications, we aim to improve outcomes for those undergoing this procedure.
Post-EVAR Care and Follow-Up Requirements
After EVAR, care is complex. It includes watching the patient closely right after the procedure, regular check-ups, and handling any problems that come up. Good follow-up care is key to the success of the repair and to tackle any issues.
Immediate Post-Procedure Monitoring
Right after EVAR, patients are watched closely in a recovery area. We look for signs of endoleak, stent graft migration, or other problems. They usually stay in the hospital for a few days for observation.
Key aspects of immediate post-procedure care include:
- Monitoring vital signs and renal function
- Assessing for signs of endoleak or stent graft migration
- Managing post-procedure pain and discomfort
- Ensuring adequate hydration and renal perfusion
Long-Term Surveillance Imaging Protocols
Long-term checks are vital to catch any late problems, like endoleaks or stent fractures. We use CT angiography or duplex ultrasound at set times.
| Imaging Modality | Frequency | Purpose |
| CT Angiography | At 1, 6, and 12 months, then annually | To assess stent graft position and detect endoleaks |
| Duplex Ultrasound | Annually or as needed based on CT findings | To monitor aneurysm size and detect endoleaks |
Managing Late Complications
After EVAR, problems like endoleaks or stent graft migration can happen. We handle these based on how serious they are and the patient’s health.
Strategies for managing late complications may involve:
- Reintervention with additional stent grafting or embolization
- Close surveillance with regular imaging
- Open surgical conversion in selected cases
Advanced Techniques in Aortic Stent Surgery
Advanced techniques in aortic stent surgery have changed how we treat complex abdominal aortic aneurysms. These new methods have opened doors for patients who were once not good candidates for standard EVAR.
Fenestrated and Branched Stent Grafts
Fenestrated and branched stent grafts are big steps forward in EVAR. These custom-made devices fit complex aortic shapes, including aneurysms near major arteries.
These grafts keep blood flowing to important organs like the kidneys and intestines. They also block the aneurysm from blood flow. Branched grafts go further by adding branches to directly feed these arteries.
Chimney and Snorkel Techniques for Complex Anatomy
For cases where standard grafts don’t work, chimney and snorkel grafts are used. These methods add extra stent grafts to keep blood flowing to side arteries.
The chimney technique is popular for its ability to extend the graft’s reach. It keeps blood flowing to key arteries, leading to good results for complex aneurysms.
Emerging Technologies in Endovascular AAA
The world of endovascular AAA repair is always growing, with new tech on the horizon. We’re seeing better stent graft materials, improved delivery systems, and new designs. These advancements aim to make the procedure easier and better for patients.
One exciting area is the development of biodegradable stent grafts and drug-eluting stents. They could lower the risk of long-term problems and make repairs last longer.
As these new methods and technologies get better, we’ll see even more progress in treating abdominal aortic aneurysms. This brings new hope to those with complex conditions.
When Traditional Open Surgical Repair Remains Necessary
EVAR is a common treatment for AAA, but not always the best choice. We look at when open surgical repair is needed. This includes complex anatomy, young patients, and emergency ruptures.
Anatomical Limitations for Endovascular Approaches
Not every patient can have EVAR due to their body’s shape. Complex aortic anatomy makes it hard to seal with a stent graft. Open surgery is more reliable in these cases.
Patients with hostile aortic neck anatomy or iliac artery disease also need open repair. We choose the best treatment based on each patient’s needs.
Young Patients and Long-Term Durability Concerns
Young patients with AAA worry about the repair lasting a long time. EVAR is less invasive, but stent grafts may not last as long. Open repair is known for its durability, making it better for those living longer.
We look at the patient’s age, health, and body shape to decide the best treatment.
Emergency Situations and Ruptured Aneurysms
In emergencies, like ruptured aneurysms, open surgery is usually the best choice. Rapid surgical intervention is key to prevent more harm and improve chances of survival.
EVAR might be used in some emergencies, but open repair is the standard for many ruptured AAAs. We are ready to handle these urgent cases, providing quick and effective care to save lives.
Conclusion: The Future of Abdominal Aortic Aneurysm Treatment
The treatment of abdominal aortic aneurysms (AAA) has changed a lot with Endovascular Aneurysm Repair (EVAR). We can expect more improvements in EVAR technology and techniques. This will lead to better results and more treatment options.
New stent grafts and devices are being made to avoid complications and reduce the need for more surgeries. Now, EVAR can be done without open surgery, thanks to new tech. For more on AAA treatment’s future, check out the latest endovascular therapies.
EVAR is getting better, which means better results for patients, shorter recovery times, and more options for complex cases. The growth of new stent grafts and other tech will shape AAA treatment’s future.
FAQ
What is an abdominal aortic aneurysm?
An abdominal aortic aneurysm is a swelling of the main blood vessel leading from the heart to the abdomen. It happens when the aorta’s wall weakens, causing it to bulge outward.
What is endovascular repair of abdominal aortic aneurysm (EVAR)?
EVAR is a minimally invasive surgery for abdominal aortic aneurysms. It involves placing a stent graft in the aorta to prevent further growth and rupture.
How is EVAR different from open surgical repair?
EVAR is less invasive than open surgery. It doesn’t require a big cut in the abdomen. Instead, small cuts in the groin are used to access the aorta.
What are the benefits of EVAR compared to open surgical repair?
EVAR leads to shorter hospital stays and less pain. Recovery is quicker. It also has fewer complications and lower mortality rates.
Who is a candidate for EVAR?
Patients with suitable anatomy for stent graft placement are candidates for EVAR. The decision is based on the aneurysm’s size, location, and the patient’s health.
What are the possible complications of EVAR?
EVAR complications include endoleaks, stent graft migration, and device failure. Endoleaks happen when blood leaks into the aneurysm sac around the stent graft.
What is the role of imaging in EVAR?
Imaging is key in EVAR. It helps plan the procedure, guide stent graft placement, and monitor for complications after the procedure.
How often do patients need to undergo surveillance imaging after EVAR?
Patients need regular surveillance imaging after EVAR. The frequency depends on individual factors and the stent graft type used.
Can EVAR be used to treat ruptured abdominal aortic aneurysms?
EVAR can treat ruptured aneurysms in emergency situations. Suitability depends on patient factors and stent graft availability.
What are fenestrated and branched stent grafts?
Fenestrated and branched stent grafts treat complex aneurysms involving branch vessels. They preserve blood flow to vital organs while excluding the aneurysm.
What is the future of EVAR and abdominal aortic aneurysm treatment?
EVAR’s future includes advancements in stent graft technology, imaging, and techniques. These will improve outcomes, reduce complications, and treat more patients.
What is an abdominal aortic stent graft?
An abdominal aortic stent graft is a device for treating aneurysms. It’s a tube-like structure made of fabric and metal placed inside the aorta to prevent growth and rupture.
How does an abdominal aortic stent graft procedure work?
The procedure involves small groin incisions to access the aorta. The stent graft is then guided to the aneurysm site. Once in place, it expands to fit the aorta’s walls, excluding the aneurysm.
References:
- Moll, F. L., Powell, J. T., Fraedrich, G., Verzini, F., Haulon, S., Waltham, M., … Böckler, D. (2011). Management of abdominal aortic aneurysms clinical practice guidelines of the European society for vascular surgery. European Journal of Vascular and Endovascular Surgery, 41(1), S1-S58. Retrieved from https://www.ejves.com/article/S1078-5884(10)00494-7/fulltext