Anemia is a complex condition that affects millions of people worldwide. It includes over 400 distinct conditions, but seven main types are widely recognized. Understanding these types is essential for accurate diagnosis and effective management. Understand the anemic meaning and learn about the 7 types of anemia, including which ones are the most serious for your long-term health.
We will look at the different forms of anemia, including their causes and characteristics. Anemia can come from many factors, like iron deficiency, chronic diseases, or genetic disorders. For a full look at anemia, including its types and causes, check out .
It’s important to know the different types of anemia for effective patient care. We’ll go into the details of each type, giving insights into their diagnosis and treatment.
Key Takeaways
- Anemia encompasses over 400 distinct conditions.
- Seven main types of anemia are widely recognized.
- Understanding anemia types is key for diagnosis and management.
- Anemia can result from iron deficiency, chronic diseases, or genetic disorders.
- Effective patient care requires recognizing the different types of anemia.
Understanding Anemia: An Overview
The term ‘anemic’ is often used, but what does it really mean to be anemic, and how does it affect the body? Anemia is a condition where there’s not enough red blood cells. These cells are key for carrying oxygen around the body.
What Happens in the Body During Anemia
During anemia, the body’s tissues and organs don’t get enough oxygen. This leads to various health problems. Anemia can be caused by not making enough red blood cells, losing too many, or having them destroyed too fast.
Being anemic means our body can’t carry enough oxygen. This can cause fatigue, weakness, and shortness of breath. Knowing what anemic means helps us understand its impact on our health.
Common Symptoms and Warning Signs
It’s important to recognize anemia symptoms early. Common signs include:
- Persistent fatigue and weakness
- Pale skin
- Shortness of breath
- Dizziness or lightheadedness
- Cold hands and feet
These symptoms can change based on the type and severity of anemia. If you or someone you know shows these signs, seeing a doctor is key.
Knowing what it means to be anemic and spotting symptoms early can help. It leads to better medical care and a better life.
The Anemic Meaning: Definition and Basic Concepts
It’s important to know what anemia is. Anemia is when you don’t have enough red blood cells. These cells carry oxygen to all parts of your body.
Medical Definition of Being Anemic
To be anemic, your hemoglobin or red blood cell count must be low. Hemoglobin is a protein in red blood cells that carries oxygen. There are different types of anemia, like iron deficiency anemia and anemia from chronic diseases.
Key indicators of anemia include:
- Low hemoglobin levels
- Reduced red blood cell count
- Symptoms such as fatigue, weakness, and shortness of breath
How Anemia Affects Daily Life
Anemia can really change your life. It affects how you feel physically and mentally. Symptoms can be mild or severe, like feeling tired, dizzy, or having trouble focusing.
|
Aspect of Life |
Impact of Anemia |
|---|---|
|
Physical Activity |
Reduced stamina and endurance |
|
Mental Health |
Increased stress, anxiety, and depression |
|
Work and Productivity |
Decreased productivity and efficiency |
Knowing what causes anemia is key to managing it. Causes can be nutritional deficiencies, chronic diseases, or genetic disorders.
By recognizing the signs and understanding the causes, you can get the right medical care. You can also make lifestyle changes to better manage your condition.
Global Impact of Anemia
Anemia is a big health problem worldwide. It affects not just people but also communities and healthcare systems. This shows how important it is to address anemia globally.
Prevalence Statistics Worldwide
Anemia is a major public health issue everywhere. Iron deficiency anemia is the most common type. It affects about 1.2 billion people globally, leading to a lot of health problems.
In low- and middle-income countries, anemia is even more common. This is because of poor nutrition, limited healthcare access, and high infection rates.
Most Affected Populations
Some groups face anemia more often. These include pregnant women, kids under five, and people with chronic diseases. Pregnant women need more iron, and kids need more nutrients for growth.
People with chronic diseases can also get anemia. This is because their conditions can make it hard for their bodies to get enough nutrients.
Iron Deficiency Anemia: The Most Common Type

Iron deficiency anemia is the most common type of anemia, affecting millions worldwide. It happens when the body lacks enough iron to make hemoglobin. Hemoglobin is a protein in red blood cells that carries oxygen.
Causes and Risk Factors
Several factors lead to iron deficiency anemia. Inadequate dietary intake of iron is a big cause. This is true for those who eat mostly plants, as plant iron is harder for the body to absorb.
Other risk factors include chronic blood loss. This can happen from heavy periods, internal bleeding, or giving blood often. Conditions like celiac disease or stomach surgery can also make it hard for the body to absorb iron.
Symptoms and Diagnosis
Symptoms of iron deficiency anemia vary but often include fatigue, weakness, and shortness of breath. In severe cases, it can cause heart problems.
To diagnose, doctors use blood tests to check hemoglobin levels and iron stores. They also do physical exams and ask about your medical history to find the cause.
“Iron deficiency anemia is a significant public health concern, specially in developing countries where access to iron-rich foods and healthcare may be limited.”— World Health Organization
Treatment Approaches
Treatment for iron deficiency anemia often includes iron supplements. Eating more iron-rich foods is also advised. These include red meat, poultry, fish, beans, and fortified cereals.
In some cases, intravenous iron therapy is needed for those who can’t take pills or have severe deficiency. It’s also important to address the cause, like managing chronic blood loss, for effective treatment.
Vitamin B12 Deficiency Anemia
Vitamin B12 deficiency anemia happens when the body doesn’t have enough Vitamin B12. This vitamin is key for making healthy red blood cells. Without it, the body can’t make enough red blood cells, leading to health problems.
Role of B12 in Red Blood Cell Production
Vitamin B12 is vital for making red blood cells. It helps create DNA, which is needed for cell division and making red blood cells. Without enough Vitamin B12, the body makes big, abnormal red blood cells. These cells can’t work right, causing anemia.
Understanding Vitamin B12’s role in making red blood cells is key. We’ll look at how not having enough Vitamin B12 affects the body and how to fix it.
Identifying and Treating B12 Deficiency
To find Vitamin B12 deficiency anemia, blood tests are used. These tests check Vitamin B12 levels and for anemia. Symptoms include feeling tired, weak, and having neurological issues.
Treatment for Vitamin B12 deficiency anemia usually means taking Vitamin B12 supplements. These can be taken by mouth or given as injections, based on how bad the deficiency is and how well the body absorbs the vitamin.
Pernicious Anemia: A Special Case
Pernicious anemia is a type of Vitamin B12 deficiency anemia. It happens when the body can’t absorb Vitamin B12. This is because the stomach lining is damaged, stopping the body from making intrinsic factor, a protein needed for Vitamin B12 absorption.
Pernicious anemia needs special treatment. This often means getting Vitamin B12 injections for life. This way, the body doesn’t need intrinsic factor to absorb Vitamin B12. Knowing about pernicious anemia is important for giving the right care to those affected.
By understanding Vitamin B12’s role in making red blood cells and how to treat deficiencies, we can help manage Vitamin B12 deficiency anemia. This improves health outcomes for patients.
Folate Deficiency Anemia
Folate deficiency anemia happens when the body doesn’t have enough folate. Folate, or vitamin B9, is key for making red blood cells. Without enough, the body can’t make or keep healthy red blood cells, causing anemia.
Causes of Folate Deficiency
There are many reasons for folate deficiency. These include not eating enough folate-rich foods and certain health issues. Poor dietary habits and malabsorption issues play big roles.
Some groups are more at risk. This includes pregnant women, people with alcohol problems, and those with gut disorders.
Symptoms and Diagnosis
Symptoms of folate deficiency anemia include feeling very tired, weak, and short of breath. Doctors use blood tests to check folate levels and look at red blood cells.
They also check for reasons why folate levels are low. This could be because of not eating enough or not absorbing nutrients well.
Treatment and Prevention
Treatment usually means taking folate supplements and eating more folate-rich foods. Foods like leafy greens, legumes, and fortified cereals are good sources.
To prevent folate deficiency anemia, eat a balanced diet and manage health issues. Pregnant women are often told to take folate supplements to help their baby grow.
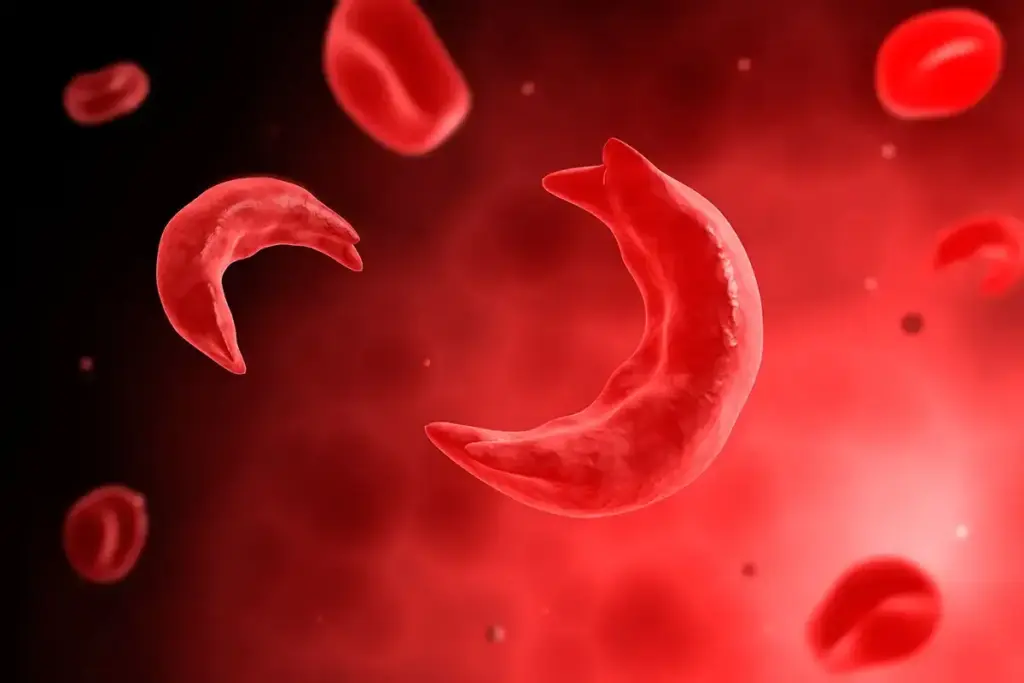
Hemolytic Anemia: When Red Blood Cells Are Destroyed
Hemolytic anemia is when red blood cells are destroyed too quickly. This leads to a lack of healthy red blood cells in the body. It’s a major type of anemia.
Inherited Forms
Inherited hemolytic anemia comes from genetic mutations. These mutations can make red blood cells more likely to break down.
Some common inherited forms include:
- Sickle cell anemia
- Thalassemia
- Hereditary spherocytosis
These conditions can vary in severity. They may need different treatments.
Acquired Hemolytic Anemia
Acquired hemolytic anemia is not passed down but develops over time. It can be caused by:
- Autoimmune disorders
- Infections
- Certain medications
- Cancer
Finding the cause is key to treating it effectively.
Management Strategies
Managing hemolytic anemia involves treatments to reduce red blood cell destruction. It also helps the body make new red blood cells.
Some strategies include:
- Medications: To slow down the immune system if it’s attacking red blood cells.
- Blood transfusions: To increase healthy red blood cells.
- Lifestyle changes: Avoiding substances that can cause red blood cell breakdown.
Understanding the cause and using the right treatments can help people with hemolytic anemia. It can make their lives more comfortable and reduce anemic symptoms.
Aplastic Anemia: Bone Marrow Failure
Aplastic anemia is a rare and serious condition where the bone marrow fails. It doesn’t make enough blood cells, like red and white blood cells, and platelets.
Causes and Risk Factors
It’s hard to find out what causes aplastic anemia. But, some things can raise your risk. These include chemicals like pesticides and certain drugs.
Viral infections, like hepatitis and HIV, can also harm the bone marrow. Sometimes, it’s linked to other diseases, like autoimmune disorders and cancers.
Diagnosis and Testing
To diagnose aplastic anemia, doctors use blood tests and bone marrow biopsies. Blood tests show low counts of blood cells. A bone marrow biopsy checks if the marrow is working right.
They might also do genetic tests and imaging studies. These help find other possible causes.
Treatment Options
Treatment for aplastic anemia depends on how severe it is and why it happened. For mild cases, the focus is on managing symptoms. For more serious cases, doctors might use immunosuppressive therapy.
For younger patients, a bone marrow transplant might be an option. Supportive care, like blood transfusions and antibiotics, is also important. It helps manage the condition and prevent infections.
Living with aplastic anemia is tough, but with the right treatment, many people manage well. It’s key to work closely with healthcare professionals to find the best treatment plan.
Thalassemia: Genetic Blood Disorders
Thalassemia is a hereditary condition that affects how the body makes hemoglobin. Hemoglobin is a protein in red blood cells that carries oxygen. Knowing about thalassemia is key for diagnosing and treating it.
Alpha and Beta Thalassemia
Thalassemia comes in two main types: Alpha and Beta. The type depends on which part of the hemoglobin is affected.
- Alpha Thalassemia: This happens when there’s a problem with the genes for alpha-globin. The severity depends on how many genes are affected.
- Beta Thalassemia: It’s caused by issues with the HBB gene on chromosome 11. It affects the beta-globin chains. The severity can range from mild to severe.
Severity Levels and Symptoms
The symptoms of thalassemia vary based on how severe it is.
|
Severity Level |
Symptoms |
Characteristics |
|---|---|---|
|
Mild |
May have no symptoms or mild anemia |
Often requires minimal or no treatment |
|
Moderate |
Anemia, fatigue, pale skin |
May require regular blood transfusions |
|
Severe |
Severe anemia, failure to thrive in children, bone deformities |
Requires regular blood transfusions and other intensive treatments |
Living with Thalassemia
Managing thalassemia involves a detailed plan. This includes regular check-ups, blood transfusions, and sometimes bone marrow transplants. It’s also important to be aware of complications and how to handle them.
For those with thalassemia, understanding the condition and following the treatment plan is essential. Knowing the signs of complications and when to seek medical help is vital. Good management can greatly improve life quality.
Diagnosing thalassemia involves blood tests and genetic analysis. This helps determine the type and severity. Treatment plans are customized to meet individual needs, focusing on symptom management and preventing complications.
Sickle Cell Anemia: A Hereditary Condition
Sickle cell anemia is a condition where red blood cells don’t shape right. This makes it hard for them to carry oxygen well.
Genetic Basis
This condition comes from a gene mutation in the HBB gene. This gene is for the beta-globin part of hemoglobin. The mutation makes abnormal hemoglobin, called sickle hemoglobin or HbS.
The disease is passed down in an autosomal recessive pattern. This means a person needs two bad HBB genes (one from each parent) to have it.
Symptoms and Complications
People with sickle cell anemia face many symptoms. These include pain episodes, anemia, and a higher chance of getting infections. The sickling of red blood cells can block small blood vessels, causing pain and tissue damage.
Other issues can be splenic sequestration, stroke, and acute chest syndrome. It’s important to watch and manage these problems closely.
Current Treatments and Research
Treatments aim to manage symptoms, prevent problems, and improve life quality. This includes pain relief, blood transfusions, and drugs like hydroxyurea.
Scientists are working on new treatments. They’re looking into gene therapy and other ways to fix the genetic defect.
|
Treatment Approach |
Description |
Benefits |
|---|---|---|
|
Pain Management |
Use of medications to alleviate pain during crises |
Reduces suffering and improves quality of life |
|
Blood Transfusions |
Transfusion of normal red blood cells to reduce HbS percentage |
Decreases risk of complications like stroke |
|
Hydroxyurea |
Medication that reduces frequency of pain crises |
Improves quality of life and reduces hospitalizations |
Diagnosing Anemia: Tests and Procedures
Understanding anemia starts with the right diagnosis. Blood tests and other methods help us find the cause. This is key to treating it right.
We use many tools to find out if you have anemia. First, we look at your medical history and do a physical check. Then, we do specific tests to confirm it.
Blood Tests and What They Reveal
Blood tests are the main way to diagnose anemia. They show how severe and what type it is. Important tests include:
- Complete Blood Count (CBC): Checks red and white blood cells, and platelets.
- Reticulocyte Count: Sees how many new red blood cells the bone marrow makes.
- Iron Studies: Looks at iron levels, like serum iron and ferritin.
- Vitamin B12 and Folate Levels: Finds out if you’re lacking these important nutrients.
|
Blood Test |
Normal Range |
What It Indicates |
|---|---|---|
|
Hemoglobin (Hb) |
13.8-17.2 g/dL (men), 12.1-15.1 g/dL (women) |
Low levels mean you have anemia. |
|
Mean Corpuscular Volume (MCV) |
80-100 fL |
Tells us if your anemia is small, normal, or big cell. |
Additional Diagnostic Procedures
Other tests might be needed to find why you have anemia. These include:
- Bone Marrow Biopsy: Looks at the bone marrow to see how it’s working.
- Endoscopy: Checks for bleeding in the stomach or intestines.
- Genetic Testing: Finds genetic problems like thalassemia or sickle cell anemia.
The World Health Organization says diagnosing anemia is a big deal. It needs a detailed approach.
“Anemia is not a disease, but a sign of an underlying condition that needs to be diagnosed and treated.”
By using all these methods, we can find out if you have anemia. We can then treat it in a way that fits you best.
Treatment Approaches for Different Anemia Types
Treating anemia involves many strategies, from diet changes to medical treatments. The right treatment depends on the cause, how severe it is, and the patient’s health.
Nutritional Interventions
For many anemia types, like iron deficiency, diet changes are key. Increasing iron intake through food or supplements helps a lot. Eating foods high in iron, like red meat and spinach, is good. Also, vitamin C helps iron absorption, so eating foods with vitamin C, like citrus fruits, is helpful too.
Medications and Supplements
If diet changes don’t work, medicines and supplements are needed. Iron supplements are often given for iron deficiency anemia. For vitamin B12 deficiency, vitamin B12 injections or pills help. Folate supplements treat folate deficiency anemia. Sometimes, medicines that help make more red blood cells are used, like for chronic diseases.
Advanced Treatments for Severe Cases
For very severe anemia, more serious treatments are needed. Blood transfusions quickly raise red blood cell counts, easing symptoms. For genetic anemias like thalassemia or sickle cell, bone marrow transplantation might be an option. Also, medicines that manage complications or the underlying cause, like hydroxyurea for sickle cell anemia, are important.
Managing anemia is a journey that needs patience and the right treatment. Tailoring treatment to the specific anemia type and cause helps improve outcomes.
Preventing Anemia: Dietary and Lifestyle Factors
To prevent anemia, we need to make dietary changes and lifestyle adjustments. Understanding anemia causes and how to treat it through nutrition and lifestyle helps a lot. This way, we can lower its occurrence.
Iron-Rich Foods and Absorption
Iron is key for making red blood cells. Eating foods rich in iron is a big step in stopping iron deficiency anemia. Foods high in iron include red meat, poultry, fish, beans, lentils, and fortified cereals. But, it’s not just about eating these foods; enhancing iron absorption is also key.
Vitamin C helps a lot with iron absorption. So, eating foods rich in vitamin C (like citrus fruits, bell peppers, and tomatoes) with iron-rich foods boosts absorption. But, tea and coffee can block iron absorption if eaten with iron-rich foods.
- Include a variety of iron-rich foods in your diet.
- Consume vitamin C-rich foods alongside iron-rich foods.
- Avoid tea and coffee when eating iron-rich foods.
Other Nutrients Essential for Blood Health
Besides iron, other nutrients are important for healthy red blood cells. Vitamin B12 and folate are key for making red blood cells. Not having enough of these can cause different anemia types.
Foods high in vitamin B12 are meat, fish, poultry, eggs, and dairy. For folate, eat dark leafy greens, legumes, and fortified cereals. Getting enough of these nutrients through food or supplements is important for avoiding anemia.
“A well-balanced diet that includes a variety of foods can help prevent nutritional deficiencies, including those that lead to anemia.”
By eating a diet full of essential nutrients and living a healthy lifestyle, we can stop anemia and stay healthy.
Special Considerations: Anemia in Pregnancy and Children
It’s important to know about anemia in pregnancy and children. Anemia can affect both the mother and the child. It’s a condition that needs quick diagnosis and treatment.
Maternal Anemia and Its Effects
Anemia in pregnancy is a big worry. It can harm both the mother and the baby. Maternal anemia often comes from iron deficiency, but other issues can also cause it.
Pregnancy changes the body’s needs for iron and other nutrients. If these needs aren’t met, anemia can happen. Regular prenatal care helps catch and manage anemia early.
|
Risks Associated with Maternal Anemia |
Potential Complications |
|---|---|
|
Preterm Labor |
Increased risk of premature birth |
|
Low Birth Weight |
Potential for developmental issues |
|
Maternal Fatigue |
Reduced quality of life and ability to care for newborn |
Childhood Anemia: Causes and Prevention
Anemia in kids is a big concern. It can be caused by many things, like not getting enough nutrients. Iron deficiency is a main reason for anemia in kids, often because of a bad diet.
To prevent anemia, kids need a diet full of iron and other important nutrients. They also need regular health checks. Early diagnosis through anemia diagnosis tests is key to helping them.
Knowing about anemic meaning in pregnancy and childhood is very important. It shows why we need to be aware and take steps to stop and treat anemia in these groups.
When to Seek Medical Help for Anemia
Anemia is a serious condition that needs timely medical attention. Some cases are mild and can be managed with diet changes. But, others are severe and require immediate care.
Emergency Warning Signs
Some symptoms mean you need to see a doctor right away. These include:
- Severe shortness of breath: Feeling winded even when sitting or doing light activities.
- Chest pain: Pain in the chest that spreads to arms, back, neck, jaw, or stomach.
- Dizziness or fainting: Feeling dizzy or fainting, which can mean a big drop in blood pressure or severe anemia.
- Rapid heartbeat: A fast or irregular heartbeat that shows anemia’s effect on the heart.
Finding the Right Specialist
If you have anemia symptoms or have been diagnosed, finding the right doctor is key. Start with your primary care doctor. They can send you to a specialist if needed. Hematologists, who focus on blood disorders, are good for anemia.
Look for a doctor with experience in anemia. They should have a good treatment plan and be ready to answer your questions.
Conclusion: Living Well with Anemia
Living with anemia means knowing what it is and the types that exist. It’s important to manage it well to live a good life.
At Liv Hospital, we focus on the latest care and ethics. We meet international healthcare standards. Our goal is to give top-notch care for all anemia types.
It’s key to know the causes, signs, and treatments for anemia. For more details, check out the .
By actively managing anemia, people can live full and happy lives. We aim to offer the care and support needed for the best health outcomes.
FAQ
What is anemia?
Anemia is a condition where the body doesn’t have enough red blood cells. These cells are key for carrying oxygen.
What are the main types of anemia?
There are over 400 types of anemia. The main ones include iron deficiency, vitamin B12 deficiency, and sickle cell anemia.
What are the common symptoms of anemia?
Symptoms include fatigue, weakness, and pale skin. You might also feel short of breath or dizzy.
How is anemia diagnosed?
Doctors use blood tests to find anemia. They might also do a bone marrow biopsy for more info.
What is iron deficiency anemia?
It’s the most common anemia. It happens when the body doesn’t have enough iron for hemoglobin.
How is iron deficiency anemia treated?
Treatment includes iron supplements and eating more iron-rich foods. Doctors also look for the cause.
What is vitamin B12 deficiency anemia?
It’s caused by not enough vitamin B12. This vitamin is needed for red blood cells. It can come from diet, absorption, or medical issues.
How is vitamin B12 deficiency anemia treated?
Treatment is vitamin B12 supplements and diet changes. Doctors also look for underlying causes.
Can anemia be prevented?
Yes, by eating right and making lifestyle changes. This includes iron and vitamin intake and less alcohol.
How does anemia affect pregnancy?
Anemia in pregnancy can harm both mom and baby. It can lead to preterm labor and low birth weight. Good prenatal care is key.
When should I seek medical help for anemia?
See a doctor if you have anemia symptoms. This is important for early treatment and better health.
What are the emergency warning signs of anemia?
Look out for severe shortness of breath, chest pain, and dizziness. These need immediate medical help.
How can I live well with anemia?
Manage anemia by following treatment plans and making healthy lifestyle choices. Regular check-ups with your doctor are also important.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4985396/










