Last Updated on October 20, 2025 by
![Bone Marrow Diseases: 10 Common Types, Disorders & Abnormalities [2025] 1 Bone Marrow Diseases: 10 Common Types, Disorders & Abnormalities [2025]](https://cdnint.mlphosts.com/wp-content/uploads/2025/10/image-56.jpeg)
At Liv Hospital, we know that bone marrow disorders are complex and can change lives. These conditions affect the cells that keep us healthy and strong. It’s important to understand their types and symptoms.
We focus on innovative, patient-centered care for various bone marrow conditions. Our goal is to give the best care for each patient. We deal with different bone marrow diseases, like leukemia and aplastic anemia.
Key Takeaways
- Understanding bone marrow disorders is key for effective treatment.
- Bone marrow diseases can greatly affect patients’ quality of life.
- Liv Hospital provides innovative, patient-centered care for patients with bone marrow conditions.
- There are many types of bone marrow diseases, including leukemia and aplastic anemia.
- Comprehensive care is vital for managing bone marrow abnormalities.
Understanding Bone Marrow: Function and Importance
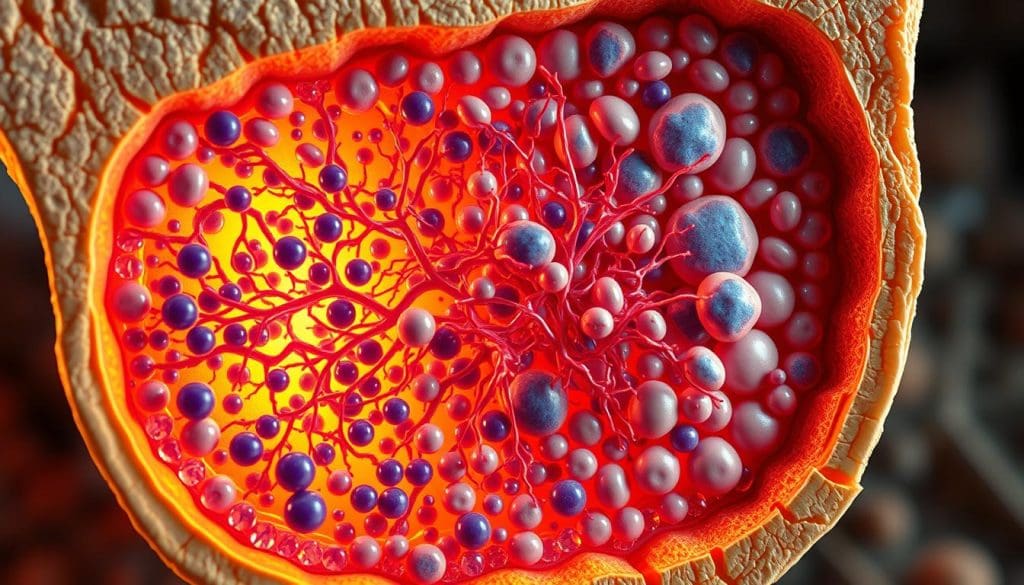
Bone marrow is a spongy tissue inside our bones. It’s key to our health, making blood cells. Bone marrow’s role in our overall health is vital.
The Role of Bone Marrow in Blood Cell Production
Bone marrow makes all blood cells. This includes red cells for oxygen, white cells for fighting infections, and platelets for clotting. The production of these cells is a highly regulated process.
“The bone marrow is a remarkable organ, capable of producing over 500 billion blood cells daily,” highlighting its critical role in sustaining life and health.
Types of Bone Marrow: Red vs. Yellow
There are two types of bone marrow: red and yellow. Red bone marrow makes blood cells, with a network of blood vessels. Yellow bone marrow has fat cells and doesn’t make blood cells in adults, but can change to red marrow.
- Red bone marrow: actively produces blood cells
- Yellow bone marrow: has fat cells, can convert to red marrow
Normal Bone Marrow Function
Normal bone marrow makes blood cells well and meets the body’s needs. It balances different cell types and regulates their release. A healthy bone marrow is essential for overall well-being.
Understanding bone marrow function is key to knowing about blood diseases. By knowing how it works normally, we can understand what happens in diseases.
Bone Marrow Disease: Classification and Overview
Bone marrow diseases cover a wide range of conditions that affect blood cell production. These issues can seriously harm a person’s health. They can lead to many problems if not treated right.
There are different types of bone marrow diseases. Knowing these types is key to finding the right treatment.
Primary vs. Secondary Bone Marrow Disorders
Bone marrow diseases can be primary or secondary. Primary ones start in the bone marrow. Secondary ones come from other conditions or outside factors.
Primary disorders include leukemia and myeloproliferative neoplasms. They directly harm the bone marrow’s blood cell production. Secondary disorders can be caused by infections, medicines, or other diseases that affect the bone marrow.
Common Symptoms and Warning Signs
The symptoms of bone marrow diseases vary. Common ones are fatigue, weakness, and shortness of breath. These often happen because of anemia or low red blood cell count.
Other signs include frequent infections, easy bruising or bleeding, and bone pain. Spotting these symptoms early is key for quick diagnosis and treatment. We stress the need to see a doctor if these signs don’t go away or get worse.
Risk Factors and Epidemiology
Many factors can lead to bone marrow diseases. These include genetics, exposure to harmful chemicals or radiation, and past treatments like chemotherapy. Knowing these risk factors helps find who might be more likely to get these diseases.
Studies show that some bone marrow diseases are more common in certain groups and ages. We keep studying these trends. This helps us understand the causes better and find ways to prevent them.
Leukemia: Cancer of the Blood-Forming Tissues
Leukemia is a cancer that makes abnormal blood cells grow too much in the bone marrow. This messes up the normal blood cell production. It leads to health problems. We’ll look at the different types of leukemia, their signs, and how to treat them.
Acute Myeloid Leukemia (AML)
Acute Myeloid Leukemia (AML) is a fast-growing cancer that starts in the bone marrow. It quickly spreads to the blood and other parts of the body. AML makes abnormal cells grow fast in the bone marrow, blocking normal blood cell production. Treatment for AML includes chemotherapy, targeted therapy, or a bone marrow transplant.
Acute Lymphoblastic Leukemia (ALL)
Acute Lymphoblastic Leukemia (ALL) affects the lymphoid cells in the bone marrow. It grows quickly if not treated. ALL is the most common cancer in kids, but it can also happen in adults. Symptoms of ALL include tiredness, fever, and easy bruising. Treatment for ALL is usually chemotherapy and sometimes a bone marrow transplant. For more on treatments, check out Healthline’s CLL treatment resource.
Chronic Myeloid Leukemia (CML)
Chronic Myeloid Leukemia (CML) is a cancer that affects white blood cells and grows slowly. It’s marked by too many myeloid cells in the bone marrow. CML is linked to a genetic abnormality called the Philadelphia chromosome. Treatment for CML often involves targeted therapy, which has greatly improved patient outcomes.
Chronic Lymphocytic Leukemia (CLL)
Chronic Lymphocytic Leukemia (CLL) is a slow-growing cancer of lymphoid cells. It’s more common in older adults. CLL can cause swollen lymph nodes, tiredness, and frequent infections. Treatment for CLL varies based on the stage and symptoms. It can include watchful waiting, chemotherapy, targeted therapy, or immunotherapy. Healthline’s article on CLL treatment offers the latest on treatment options.
Myeloproliferative Neoplasms
Myeloproliferative neoplasms are a complex group of blood disorders. They are marked by the excessive production of mature blood cells. We will explore the different subtypes of MPNs and their clinical features.
Myeloproliferative neoplasms are diseases that cause the overproduction of blood cells. This can lead to various complications. The main subtypes include Polycythemia Vera, Essential Thrombocythemia, Primary Myelofibrosis, and Chronic Neutrophilic Leukemia.
Polycythemia Vera
Polycythemia Vera (PV) is a type of MPN. It is characterized by the overproduction of red blood cells, white blood cells, and platelets. This can increase the risk of blood clots.
Symptoms may include headaches, dizziness, and itching after bathing. Treatment often involves reducing blood cell production through medication or phlebotomy.
Essential Thrombocythemia
Essential Thrombocythemia (ET) is marked by excessive platelet production. This can cause blood clotting and other complications. Patients with ET are at risk of thrombosis and may experience symptoms such as headaches and fatigue.
Management strategies include medications to reduce platelet count and prevent clotting.
Primary Myelofibrosis
Primary Myelofibrosis (PMF) is a condition where the bone marrow is replaced by fibrotic tissue. This leads to anemia and other blood-related issues. Symptoms can include severe anemia, fatigue, and enlargement of the spleen.
Treatment options vary depending on the severity of the disease. They may include medication, blood transfusions, or bone marrow transplantation.
Chronic Neutrophilic Leukemia
Chronic Neutrophilic Leukemia (CNL) is a rare type of MPN. It is characterized by the sustained proliferation of neutrophils, a type of white blood cell. This condition can lead to an increased risk of infections and other complications.
Treatment typically involves managing symptoms. It may include medication to reduce neutrophil count.
In conclusion, myeloproliferative neoplasms are a diverse group of blood disorders. They require careful diagnosis and management. Understanding the different subtypes and their clinical features is key to providing effective treatment.
Aplastic Anemia: When Bone Marrow Stops Working
Aplastic anemia is a rare and serious condition. It happens when the bone marrow can’t make blood cells. This leads to fewer red blood cells, white blood cells, and platelets.
Causes of Aplastic Anemia
Many things can cause aplastic anemia. Toxins, certain medicines, and viruses are some examples. Sometimes, the cause is unknown.
- Toxins: Chemicals like pesticides and benzene can harm the bone marrow.
- Medications: Some drugs, like antibiotics and anti-inflammatory medicines, can cause it.
- Viral Infections: Viruses like hepatitis and HIV can also affect the bone marrow.
Clinical Presentation and Diagnosis
The symptoms of aplastic anemia vary. They can include feeling very tired, getting sick easily, and bleeding or bruising.
To diagnose aplastic anemia, doctors use blood tests, bone marrow aspiration, and biopsy. These tests show how much the bone marrow is failing and rule out other conditions.
Treatment Approaches
Treatment for aplastic anemia depends on how severe it is and the patient’s health. Options include immunosuppressive therapy, bone marrow transplantation, and supportive care.
| Treatment | Description | Indications |
|---|---|---|
| Immunosuppressive Therapy | Drugs that suppress the immune system to reduce damage to the bone marrow. | Patients with severe aplastic anemia who are not candidates for bone marrow transplantation. |
| Bone Marrow Transplantation | Replacing the damaged bone marrow with healthy marrow from a donor. | Patients with severe aplastic anemia who have a suitable donor. |
| Supportive Care | Blood transfusions and antibiotics to manage symptoms and prevent infections. | All patients with aplastic anemia to manage symptoms and improve quality of life. |
Getting a diagnosis of aplastic anemia can be tough. But with the right treatment and care, many people can live well with it.
Myelodysplastic Syndromes (MDS)
Myelodysplastic syndromes (MDS) are a group of disorders where the bone marrow fails to make healthy blood cells. This failure causes anemia, infections, and bleeding problems.
Classification of MDS Subtypes
MDS is divided into subtypes based on the World Health Organization (WHO) system. This system looks at the number of blasts in the bone marrow and genetic changes.
- MDS with single lineage dysplasia
- MDS with multilineage dysplasia
- MDS with ring sideroblasts
- MDS with excess blasts
Knowing these subtypes helps doctors predict how the disease will progress and choose the right treatment.
Risk Stratification Systems
Risk stratification in MDS is key to predicting outcomes and making treatment plans. The International Prognostic Scoring System (IPSS) is a common tool. It groups patients by their risk of turning into AML.
| IPSS Category | Score | Prognosis |
|---|---|---|
| Low | 0 | Favorable |
| Intermediate-1 | 0.5-1.0 | Intermediate |
| Intermediate-2 | 1.5-2.0 | Poor |
| High | >2.5 | Very Poor |
Clinical Features and Diagnosis
MDS symptoms vary but often include anemia, neutropenia, and thrombocytopenia. Doctors use blood tests, bone marrow aspiration, and cytogenetic analysis for diagnosis.
“The diagnosis of MDS requires a detailed evaluation, including morphological assessment, cytogenetics, and molecular studies, to accurately diagnose and subtype the disease.”
Progression to Acute Myeloid Leukemia
One major concern in MDS is the risk of turning into Acute Myeloid Leukemia (AML). Patients with higher-risk MDS are more likely to develop AML. This requires close monitoring and aggressive treatment.
Managing MDS is complex, and a personalized approach is essential. Understanding MDS subtypes, risk stratification, and symptoms helps doctors provide better care.
Multiple Myeloma: Cancer of Plasma Cells
Multiple myeloma is a serious cancer of plasma cells. It’s a challenge to diagnose and treat. We’ll look into its causes, symptoms, stages, and treatments to grasp this complex bone marrow disease.
Pathophysiology and Disease Mechanism
Multiple myeloma is when bad plasma cells grow too much in the bone marrow. This messes up the marrow’s job, causing anemia, bone damage, and weak immunity.
The disease works by bad cells and the bone marrow working together. Cytokines and growth factors help the cancer cells grow. For example, myeloma cells and bone marrow cells make growth factors that help the tumor grow.
“The bone marrow microenvironment plays a critical role in the pathogenesis of multiple myeloma, providing a sanctuary for myeloma cells to survive and proliferate.”
Clinical Manifestations
People with multiple myeloma have many symptoms. These include bone pain, tiredness, frequent infections, and high calcium levels.
The symptoms can be remembered with the CRAB mnemonic:
- C: High calcium
- R: Kidney problems
- A: Anemia
- B: Bone damage
Staging and Risk Assessment
Staging multiple myeloma is key for knowing the outlook and treatment plan. The International Staging System (ISS) is used. It looks at serum albumin and beta-2 microglobulin levels.
| Stage | Criteria | Median Survival |
|---|---|---|
| I | Serum beta-2 microglobulin | 62 months |
| II | Neither stage I nor stage III | 44 months |
| III | Serum beta-2 microglobulin ≥ 5.5 mg/L | 29 months |
Current Treatment Approaches
Treatment for multiple myeloma has improved a lot. New drugs and combinations are available. We have proteasome inhibitors, immunomodulatory drugs, and monoclonal antibodies.
Treatment plans are made for each patient. They consider age, health, and risk level. For some, getting stem cells back is a key part of treatment.
As we learn more about multiple myeloma, we’re getting better treatments. The future looks bright for better patient care.
Inherited Bone Marrow Failure Syndromes
We will look at genetic conditions called inherited bone marrow failure syndromes. These affect how the bone marrow makes blood cells. They cause health problems because the bone marrow can’t make enough blood cells.
Fanconi Anemia
Fanconi anemia is a rare genetic disorder. It makes it hard for the body to make blood cells, leading to bone marrow failure. People with Fanconi anemia often have anemia, infections, and bleeding because they don’t have enough blood cells.
Diamond-Blackfan Anemia
Diamond-Blackfan anemia affects the production of red blood cells. It causes a severe lack of red blood cells, leading to anemia soon after birth. It can also cause other problems like congenital anomalies and slow growth.
Shwachman-Diamond Syndrome
Shwachman-Diamond syndrome is a rare genetic disorder. It affects the bone marrow’s ability to make blood cells and the pancreas’s function. It causes exocrine pancreatic insufficiency, bone marrow problems, and a higher risk of infections and leukemia.
Dyskeratosis Congenita
Dyskeratosis congenita is an inherited disorder. It causes the skin and mucous membranes to age too quickly and leads to bone marrow failure. It is known for a classic triad of skin hyperpigmentation, nail dystrophy, and oral leukoplakia. Bone marrow failure is a big risk, leading to aplastic anemia and other problems.
| Syndrome | Primary Characteristics | Bone Marrow Impact |
|---|---|---|
| Fanconi Anemia | Congenital abnormalities, cancer risk | Bone marrow failure |
| Diamond-Blackfan Anemia | Red blood cell deficiency, congenital anomalies | Red blood cell production affected |
| Shwachman-Diamond Syndrome | Pancreatic insufficiency, infections, leukemia risk | Bone marrow dysfunction |
| Dyskeratosis Congenita | Skin hyperpigmentation, nail dystrophy, oral leukoplakia | Bone marrow failure |
Diagnosis and Testing for Bone Marrow Abnormalities
We use different tests to find bone marrow diseases and disorders. These tests help us know what kind of problem there is, what treatment to use, and how the disease is changing.
Blood Tests and Complete Blood Count
Blood tests are often the first step in finding bone marrow problems. A Complete Blood Count (CBC) checks the levels of different blood cells. It looks at red blood cells, white blood cells, and platelets.
A CBC can show if there’s a problem like anemia, leukopenia, or thrombocytopenia. For example, low red blood cells might mean aplastic anemia or myelodysplastic syndrome.
| Blood Test Component | Normal Range | Possible Indication of Abnormality |
|---|---|---|
| Red Blood Cells (RBC) | 4.32-5.72 million cells/μL | Anemia or Erythrocytosis |
| White Blood Cells (WBC) | 3.5-10.5 thousand cells/μL | Leukemia or Infection |
| Platelets | 150-450 thousand cells/μL | Thrombocytopenia or Thrombocytosis |
Bone Marrow Aspiration and Biopsy
Bone marrow aspiration and biopsy are key tests for finding bone marrow problems. They remove a sample of bone marrow for checking.
In a bone marrow aspiration, a needle takes out a sample of marrow. This sample is checked for abnormal cells. A bone marrow biopsy takes a small piece of bone tissue for checking too.
“Bone marrow aspiration and biopsy are essential for diagnosing and monitoring various bone marrow disorders, including leukemia and myelodysplastic syndromes.”
Cytogenetic Analysis
Cytogenetic analysis looks at the chromosomes of bone marrow cells for genetic problems. This test helps find conditions like leukemia and guides treatment.
This test can find chromosomal issues, like translocations or deletions, in bone marrow diseases. For example, the Philadelphia chromosome is a sign of chronic myeloid leukemia (CML).
Molecular and Genetic Testing
Molecular and genetic testing find specific genetic changes in bone marrow cells. These tests give detailed info on the disease’s genetics, helping decide treatment.
Tests like PCR and next-generation sequencing (NGS) can spot mutations. For example, they can find FLT3-ITD in acute myeloid leukemia (AML) or the BCR-ABL fusion gene in CML.
By using these tests together, doctors can accurately diagnose and manage bone marrow problems. This improves patient care and outcomes.
Conclusion: Advances in Bone Marrow Disease Treatment
We’ve seen big steps forward in treating bone marrow diseases. This brings new hope to those with abnormal bone marrow and different bone marrow conditions. These advances have changed how we manage these complex conditions, making life better for patients.
Now, treating bone marrow diseases includes new methods like targeted therapies and stem cell transplants. These new ways have helped patients with leukemia, myeloproliferative neoplasms, and myelodysplastic syndromes. They have a better chance of recovery.
We’re working hard to keep improving treatments and support for patients. Our aim is to offer top-notch healthcare and support to patients worldwide. We want to make sure patients get the latest and best care for their condition.
FAQ
What are bone marrow disorders?
Bone marrow disorders are conditions that affect the bone marrow. They include leukemia, myeloproliferative neoplasms, aplastic anemia, myelodysplastic syndromes, and multiple myeloma.
What is the function of bone marrow?
Bone marrow makes blood cells. It produces red blood cells, white blood cells, and platelets. These cells are key for healthy blood counts.
What are the common symptoms of bone marrow diseases?
Symptoms include fatigue, weight loss, fever, and night sweats. Bone pain, bleeding, and bruising easily are also common.
What is the difference between red and yellow bone marrow?
Red bone marrow makes blood cells. Yellow bone marrow has fat cells and doesn’t produce blood cells.
What are the risk factors for developing bone marrow diseases?
Risk factors include radiation, chemicals, and viruses. Genetic predisposition and age also play a role.
How are bone marrow diseases diagnosed?
Doctors use blood tests, bone marrow biopsies, and genetic tests. These help diagnose bone marrow diseases.
What is leukemia?
Leukemia is cancer in the bone marrow. It causes abnormal white blood cell production.
What are myeloproliferative neoplasms?
Myeloproliferative neoplasms are conditions where blood cells are overproduced. They include polycythemia vera, essential thrombocythemia, and primary myelofibrosis.
What is aplastic anemia?
Aplastic anemia is when the bone marrow can’t make blood cells. This leads to anemia, infections, and bleeding.
What are myelodysplastic syndromes?
Myelodysplastic syndromes are conditions with abnormal blood cell production. They often lead to acute myeloid leukemia.
What is multiple myeloma?
Multiple myeloma is cancer in plasma cells of the bone marrow. It causes bone damage, anemia, and kidney problems.
What are inherited bone marrow failure syndromes?
Inherited bone marrow failure syndromes are genetic disorders. They include Fanconi anemia, Diamond-Blackfan anemia, and dyskeratosis congenita.
References
- News-Medical.net: Bone Marrow Diseases
- Merck Manuals: Overview of Myeloproliferative Neoplasms
- PMC (National Library of Medicine): Chronic Myeloproliferative Neoplasms: a Collaborative Approach
- Blood (American Society of Hematology): Introduction to a review series on myeloproliferative neoplasms
- NCBI Bookshelf (StatPearls): Bone Marrow Failure
- PMC (National Library of Medicine): Bone Marrow Failure Syndromes, Overlapping Diseases with a Common Cytokine Signature