
Acute Myeloid Leukemia (AML) is a tough disease to treat. Leukemia stem cell therapy is a new hope to fight AML’s root cause.
There are big steps forward in bone marrow transplants. This gives new hope to AML patients. A recent study showed a patient’s success after an allogeneic stem cell transplant.
At Liv Hospital, we aim to give top-notch healthcare. We support patients from around the world. Our team works hard to find the best care for AML patients, including bone marrow transplant as a cure.
Key Takeaways
- Leukemia stem cell therapy targets the unique stem cell population in AML.
- Bone marrow transplant is a possible cure for AML.
- Allogeneic stem cell transplant is a treatment option for leukemia patients.
- Liv Hospital provides complete care for international patients.
- Personalized treatment plans are key for AML patients.
Understanding Acute Myeloid Leukemia (AML)
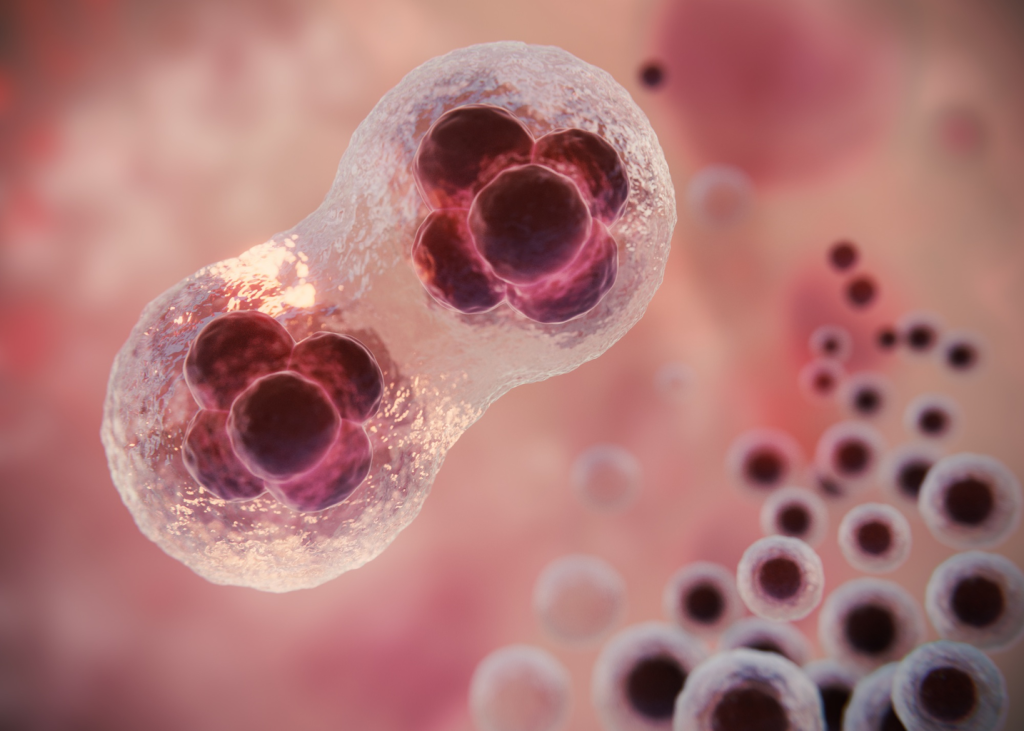
Acute Myeloid Leukemia (AML) is a condition where abnormal white blood cells grow fast in the bone marrow. This stops normal blood cells from being made, causing serious health problems.
What is AML and How Does it Develop?
AML starts when a genetic mutation happens in a stem cell. This leads to the growth of abnormal cells called leukemic blasts. These cells don’t mature right and take over the bone marrow.
The exact cause of AML is not known. But it’s thought to be due to genetics and the environment.
Risk Factors and Incidence Rates
There are several risk factors for AML. These include exposure to chemicals, radiation, and past treatments. Age is also a big risk factor, with AML becoming more common with age.
The American Cancer Society says AML rates go up a lot after 65.
| Risk Factor | Description | Impact on Incidence |
|---|---|---|
| Age | Increased risk with advancing age | Significantly higher incidence after age 65 |
| Chemical Exposure | Exposure to certain chemicals like benzene | Increased risk of developing AML |
| Previous Cancer Treatment | Previous chemotherapy or radiation therapy | Higher risk of secondary AML |
Common Symptoms and Diagnosis
AML symptoms can vary but often include tiredness, weight loss, frequent infections, and easy bruising or bleeding. Doctors use blood tests, bone marrow biopsies, and imaging to diagnose it.
Getting a diagnosis early is key for better treatment and outcomes.
The Challenge of Leukemia Stem Cells in AML
Understanding leukemia stem cells is key to tackling Acute Myeloid Leukemia (AML). These cells act like normal stem cells, growing and changing into more mature cancer cells. They are a big part of the problem in AML.
What Are Leukemia Stem Cells?
Leukemia stem cells start and grow AML. They are tough to kill with usual treatments. This makes them come back, causing relapse.
Key characteristics of leukemia stem cells include:
- Self-renewal capacity
- Ability to differentiate into more mature leukemia cells
- Resistance to conventional therapies
Why Leukemia Stem Cells Cause Disease Recurrence
Leukemia stem cells can make AML come back. They survive treatments and grow back. This leads to therapy resistance.
“The presence of leukemia stem cells is a major obstacle to achieving long-term remission in AML patients.”
A study found that these cells coming back after treatment means relapse is likely. So, we must target them to better treat AML.
Resistance to Conventional Treatments
Leukemia stem cells resist many AML treatments. They use drug pumps and stay quiet, making them hard to kill with chemotherapy.
| Mechanism of Resistance | Description |
|---|---|
| Drug Efflux Pumps | Proteins that pump chemotherapy drugs out of the cells, reducing their effectiveness. |
| Quiescence | A state of dormancy that makes leukemia stem cells less responsive to chemotherapy, which targets actively dividing cells. |
To beat these challenges, scientists are looking at new ways to fight leukemia stem cells. This includes immunotherapies and targeted therapies.
Standard Treatment Approaches for AML
AML treatment includes various therapies to help patients achieve remission and avoid relapse. The treatment plan depends on the patient’s age, health, and the leukemia’s genetic makeup.
Induction Chemotherapy
Induction chemotherapy is the first step to fight AML. It aims to kill leukemia cells in the bone marrow and blood. This lets normal cells grow back. Common agents are cytarabine and anthracyclines.
Consolidation Therapy
After remission, consolidation therapy targets any hidden leukemia cells. It’s key to lower relapse risk. This phase may include more chemotherapy or stem cell transplantation.
Targeted Therapy Options
Targeted therapies aim at specific molecules in leukemia cells. FLT3 and IDH1/2 inhibitors are examples. They help patients with certain genetic mutations.
Limitations of Standard Treatments
Though treatments have improved, there are challenges. Some patients don’t respond well, and others relapse. Chemotherapy and targeted therapy resistance are big hurdles.
| Treatment Approach | Description | Benefits |
|---|---|---|
| Induction Chemotherapy | Initial treatment to achieve remission | High response rate in newly diagnosed patients |
| Consolidation Therapy | Treatment after remission to prevent relapse | Reduces risk of relapse |
| Targeted Therapy | Treatment targeting specific genetic mutations | Effective for patients with specific mutations |
Bone Marrow Transplantation: Fundamentals
Understanding bone marrow transplantation is key for those facing AML. This treatment replaces diseased bone marrow with healthy cells. It’s a complex process.
Types of Bone Marrow Transplants
There are different bone marrow transplants, each with its own use. The main types are:
- Autologous Transplant: Uses the patient’s own stem cells, collected, stored, and then reinfused after chemotherapy.
- Allogeneic Transplant: Uses stem cells from a donor, often a sibling or unrelated donor with a matching HLA type.
- Syngeneic Transplant: Rare, uses stem cells from an identical twin, providing a perfect genetic match.
| Type of Transplant | Donor Source | Key Characteristics |
|---|---|---|
| Autologous | Patient’s own cells | Lower risk of GVHD, but may have malignant cells |
| Allogeneic | Related or unrelated donor | Higher risk of GVHD, but can fight leukemia |
| Syngeneic | Identical twin | Lowest risk of GVHD, but rare due to twin need |
The Transplantation Process
The bone marrow transplant process starts with conditioning. This includes chemotherapy and sometimes radiation. It kills the diseased bone marrow and weakens the immune system.
Then, the transplant happens. The donor’s or patient’s stem cells are infused into the bloodstream. These cells then make healthy blood cells in the bone marrow.
Donor Selection and HLA Matching
Choosing the right donor is key for allogeneic transplants. HLA matching ensures the donor and recipient are compatible. HLA typing tests for genetic markers that help the immune system.
A close HLA match lowers the risk of GVHD and improves transplant success. The HLA match is a major factor in transplant outcomes.
Allogeneic Hematopoietic Stem Cell Transplantation for AML
Allogeneic hematopoietic stem cell transplantation is a promising cure for Acute Myeloid Leukemia (AML). It replaces the patient’s sick bone marrow with healthy stem cells from a donor. This can lead to long-term remission and better survival chances.
Patient Eligibility Criteria
Choosing the right patients for this treatment is key. We look at their health, AML stage, and donor availability. High-risk AML patients or those who’ve relapsed are often the best candidates.
We also check if the patient can handle the transplant and the needed immunosuppressive therapy. This helps us pick the most likely to benefit from the treatment.
Pre-Transplant Conditioning Regimens
Pre-transplant conditioning is vital. It uses chemotherapy and radiation to clear the patient’s bone marrow and weaken their immune system. The aim is to make room for the donor stem cells to grow and produce healthy blood cells.
The regimen’s strength depends on the patient’s health and the transplant plan. Myeloablative conditioning is strong and wipes out the bone marrow. Reduced-intensity conditioning is gentler and used for older or sicker patients.
The Graft-versus-Leukemia Effect
The graft-versus-leukemia (GVL) effect is a big plus. It happens when the donor’s immune cells fight and kill the patient’s leukemia cells. This effect is a major reason why this treatment can cure AML.
“The graft-versus-leukemia effect is a key part of the treatment’s success, helping to control leukemia cells.”
Understanding and using the GVL effect can improve AML treatment outcomes for those getting this transplant.
Leukemia Stem Cell Therapy: Advanced Treatment Strategies
Leukemia stem cell therapy is a new hope in fighting AML. It focuses on targeting leukemia stem cells, a key strategy in this fight.
Targeting Specific Leukemia Stem Cell Markers
Identifying and targeting specific markers on leukemia stem cells is a big step forward. This helps us get rid of the main cause of AML coming back.
- CD123: A marker found on leukemia stem cells, making it a key target for treatment.
- CD47: Helps leukemia stem cells avoid the immune system, another important target.
- CLL-1: Being studied for its role in targeting leukemia stem cells.
By focusing on these markers, we can create treatments that are more precise and effective.
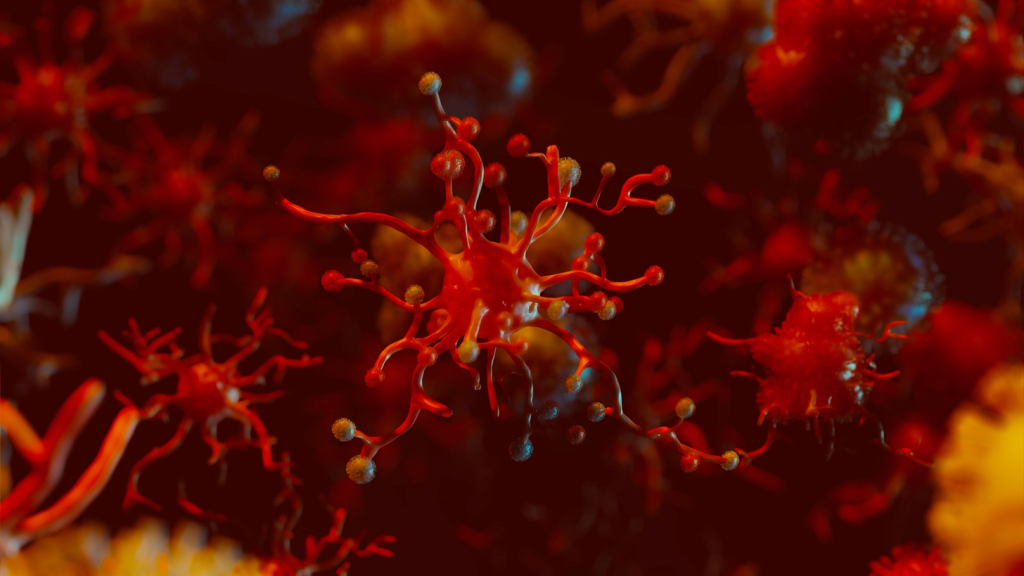
Immunotherapeutic Approaches
Immunotherapy has changed how we treat many cancers, including AML. It aims to boost the body’s immune system to fight leukemia stem cells.
Some exciting immunotherapeutic strategies include:
- CAR-T cell therapy: Genetically modifies T cells to attack leukemia stem cells.
- Checkpoint inhibitors: Allows the immune system to better target leukemia stem cells.
- Monoclonal antibodies: Binds to leukemia stem cell markers, marking them for destruction.
Combination Treatment Protocols
Using different treatments together is a promising approach. It combines targeted therapies, immunotherapies, and traditional treatments to improve outcomes.
Some possible combinations are:
- Targeted therapy + chemotherapy
- Immunotherapy + targeted therapy
- Combining different immunotherapies
Emerging Experimental Therapies
The field of leukemia stem cell therapy is growing fast. New therapies are showing promise, including:
- HIF-2α inhibitors: Like casdatifan, which may treat certain cancers.
- Stem cell-targeting bispecific antibodies: Enhances the immune response by binding to leukemia stem cells and immune cells.
As research keeps advancing, we’ll see more innovative treatments for AML, giving patients new hope.
Success Rates of Bone Marrow Transplant for AML
Knowing the success rates of bone marrow transplants is key for AML patients. This procedure, also known as hematopoietic stem cell transplantation, is a mainstay in AML treatment. It offers a chance for many patients to be cured.
Overall Survival Statistics
Research shows different survival rates for AML patients after bone marrow transplants. Success depends on the patient’s age, AML stage, and donor match. Recent data shows the survival rate can vary a lot.
A study in a top medical journal found a 5-year survival rate of 40-50% for AML patients after transplant. But, these numbers can change based on the patient group and transplant center.
Factors Affecting Transplant Outcomes
Many things can affect the success of a bone marrow transplant for AML patients. These include:
- The patient’s overall health and fitness for the transplant
- The stage of AML at the time of transplant
- The degree of HLA matching between the donor and recipient
- The conditioning regimen used before the transplant
For more detailed information on the types of cancer that require stem cell transplant, including AML, you can visit Liv Hospital’s resource page.
Long-term Survival Rates
Long-term survival rates for AML patients after bone marrow transplant are key. They show how well the treatment works over time.
| Time Post-Transplant | Survival Rate |
|---|---|
| 1 Year | 60-70% |
| 3 Years | 45-55% |
| 5 Years | 40-50% |
These numbers highlight the need for careful patient selection and post-transplant care. As medical tech and treatments improve, we expect better survival rates for AML patients.
Complications and Side Effects of Stem Cell Transplantation
Stem cell transplantation offers hope for those with acute myeloid leukemia. But, it also has risks. It’s important to know the complications that can happen.
Graft-Versus-Host Disease (GVHD)
Graft-versus-host disease is a big risk with allogeneic stem cell transplantation. It happens when the donor’s immune cells attack the recipient’s body. Managing GVHD well is key to avoiding long-term harm and improving outcomes.
Acute GVHD usually shows up within the first 100 days after the transplant. It can cause skin rashes, liver problems, or stomach issues. Chronic GVHD can happen months or years later and can affect many parts of the body, like the skin, eyes, and lungs.
Infection Risks and Prevention
Patients getting stem cell transplants face a higher risk of infections. This is because of the treatments that weaken the immune system. Preventing infections is very important.
Common infections include bacteria, viruses, and fungi. Using antibiotics and closely watching for infections can help. Teaching patients how to prevent infections is also key.
Organ Toxicities
Organ toxicities are another risk with stem cell transplantation. This is often because of the treatment. The liver, kidneys, and lungs are most at risk.
Choosing the right treatment and watching how organs work can help. We also use strategies to protect organs from damage.
Quality of Life After Transplant
After stem cell transplantation, the quality of life is very important. The treatment can cure the disease but comes with big physical and emotional challenges.
Creating care plans that cover physical, emotional, and social needs is vital. We help patients manage late effects and promote healthy living. This improves their overall well-being.
AML and Bone Marrow Transplant: Relapse Challenges
Relapse is a big problem for people with Acute Myeloid Leukemia (AML) after bone marrow transplant. This treatment can be very effective, but the risk of the leukemia coming back is always there.
Incidence and Timing of Relapse
The chance of AML coming back after transplant varies. It depends on the patient’s health before transplant, the type of transplant, and if they have graft-versus-host disease (GVHD). Most relapses happen in the first two years after transplant.
| Time Post-Transplant | Relapse Incidence |
|---|---|
| 0-6 months | High risk |
| 6-12 months | Moderate risk |
| 1-2 years | Decreasing risk |
| >2 years | Low risk |
Monitoring for Minimal Residual Disease
It’s very important to watch for minimal residual disease (MRD) after transplant. MRD are leukemia cells that are hard to find but can be spotted with special tests. Checking for MRD helps catch relapse early.
“The detection of MRD post-transplant is a strong predictor of relapse, and its presence often prompts preemptive therapeutic interventions.”
Treatment Options for Post-Transplant Relapse
When AML comes back after transplant, treatment options are few and hard to use. They might include:
- Stopping immunosuppression to help the graft fight leukemia
- Chemotherapy or targeted therapy to get the leukemia into remission
- Donor lymphocyte infusion (DLI) to boost the immune system against leukemia
- Second allogeneic transplant in some cases
Second Transplantation Considerations
Getting a second bone marrow transplant can be a cure for some with AML relapse. But, this choice depends on many things like how long the first remission lasted, the patient’s health, and if there’s a good donor.
Dealing with AML relapse after transplant needs a detailed and personal plan. By watching patients closely and using different treatments, we can help them and give them hope.
Recent Advances in Stem Cell Transplant for Leukemia
Stem cell transplantation for leukemia has seen big changes. New conditioning regimens, better donor selection, and ways to avoid complications are leading the way. These changes are making treatments more effective and safer.
Novel Conditioning Regimens
Old conditioning regimens were too harsh. Novel conditioning regimens aim to be gentler but just as effective. For example, reduced-intensity conditioning (RIC) lets older or sicker patients get transplants.
Haploidentical Transplantation
Haploidentical transplants use half-matched donors. This has opened up more donor options. Thanks to better ways to prevent GVHD and care after transplant, these transplants work as well as full matches.
GVHD Prevention Strategies
Graft-versus-host disease (GVHD) is a big problem after stem cell transplants. New ways to prevent GVHD include post-transplant cyclophosphamide and other treatments. These methods are showing great promise in reducing GVHD.
Post-Transplant Maintenance Therapies
Researchers are looking into ways to keep patients in remission after transplant. Targeted therapies and immunotherapies are being tested. For instance, FLT3 inhibitors are helping patients with FLT3-mutated AML stay in remission.
These breakthroughs are changing how we treat leukemia with stem cell transplants. As research keeps moving forward, we can look forward to even better treatments and care for patients.
Personalized Medicine in AML Treatment
Genetic and molecular profiling have led to new ways to treat AML. Personalized medicine means treating each patient based on their unique genetic and lifestyle factors. This approach aims to make treatments more effective and safer.
Genetic and Molecular Profiling
Genetic and molecular profiling help us understand AML better. By studying a patient’s leukemia cells, doctors can find specific targets for treatment. This leads to treatments that work better and have fewer side effects.
Risk-Adapted Treatment Approaches
Risk-adapted treatment plans adjust based on how likely a disease is to come back. Patients with high-risk AML might need stronger treatments, like stem cell transplants. Those with lower-risk disease might get milder treatments, which could lower the risk of complications.
Risk stratification is key in these plans. Doctors look at genetic and molecular details to sort patients into risk groups. This helps guide treatment choices.
Predictive Biomarkers for Transplant Success
Predictive biomarkers are important for deciding if a stem cell transplant will work for AML patients. Biomarkers like measurable residual disease (MRD) status and certain genetic mutations give clues about relapse risk and survival chances.
Using these biomarkers in treatment planning helps doctors make better decisions. They can figure out if a transplant is right for a patient and plan ways to reduce risks.
Conclusion: The Future of Curative Approaches for AML
Acute Myeloid Leukemia (AML) is a tough disease to treat. But, new ways to treat it are giving patients hope. The future of AML treatment looks bright, with new ways to cure it being found.
Recent studies show promise. For example, allogeneic stem cell transplant and CAR-T cell therapy are showing good results. We’re also seeing new ways to treat AML, like better conditioning regimens and ways to prevent GVHD.
As research goes on, we’ll see even better treatments for AML. It’s key to keep working on new treatments. This way, we can help more patients get better and live longer.
What is Acute Myeloid Leukemia (AML)?
Acute Myeloid Leukemia (AML) is a cancer that starts in the bone marrow. It quickly spreads to the blood. It can also go to other parts like the lymph nodes, liver, spleen, and even the brain.
Can bone marrow transplant cure AML?
Yes, a bone marrow transplant can cure AML. It replaces the bad marrow with healthy one. This can be from the patient or a donor.
What is the role of leukemia stem cells in AML?
Leukemia stem cells start and grow AML. They are hard to kill, leading to the disease coming back. Scientists are working on new ways to target these cells.
What are the different types of bone marrow transplants?
There are two main types: autologous and allogeneic. Autologous uses the patient’s own stem cells. Allogeneic uses a donor’s stem cells. Donor transplants can be related or unrelated.
What is the graft-versus-leukemia effect?
The graft-versus-leukemia effect is when donor immune cells fight leukemia cells. This can lower the chance of leukemia coming back after a transplant.
What are the possible complications of stem cell transplantation?
Complications include graft-versus-host disease, infections, and organ damage. The risk depends on the transplant type, HLA matching, and the patient’s health.
How is minimal residual disease monitored after bone marrow transplant?
MRD is checked with special tests. These tests find small leukemia cells in the blood or bone marrow. Regular checks help catch relapse early.
What is personalized medicine in AML treatment?
Personalized medicine in AML tailors treatment to the patient’s leukemia. It uses genetic and molecular profiles. This helps choose the best treatment, including bone marrow transplantation.
What are the latest advancements in leukemia stem cell therapy?
New advancements target leukemia stem cells directly. They include immunotherapy and experimental treatments. These aim to improve treatment outcomes by tackling the root cause of AML.
Can leukemia be cured with bone marrow transplant?
Bone marrow transplantation can cure leukemia, including AML. The chance of a cure depends on the disease stage, HLA matching, and the patient’s health.
What is allogeneic hematopoietic stem cell transplantation?
Allogeneic hematopoietic stem cell transplantation uses donor stem cells. It treats AML by replacing the patient’s bad marrow with healthy donor marrow.
What is the significance of HLA matching in bone marrow transplantation?
HLA matching is key in bone marrow transplantation. It lowers the risk of graft-versus-host disease and rejection. A close match between donor and recipient leads to better outcomes.
References
- U.S. National Cancer Institute. Adult AML treatment (PDQ ®). Retrieved from https://www.cancer.gov/types/leukemia/patient/adult-aml-treatment-pdq
- Nature Reviews. Therapeutic targeting of acute myeloid leukemia. Retrieved from https://www.nature.com/articles/s41568-020-00303-6
- PubMed Central (PMC). Molecular pathogenesis and targeted treatment of acute myeloid leukemia. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4116825/
- Medical News Today. Bone marrow transplant for leukemia “ what to know. Retrieved from https://www.medicalnewstoday.com/articles/bone-marrow-transplant-for-leukemia
- Cancer Research UK. Bone marrow / stem cell transplants for leukemia. Retrieved from https://www.cancerresearchuk.org/about-cancer/bone-marrow-stem-cell-transplants-leukaemia










