Cancer involves abnormal cells growing uncontrollably, invading nearby tissues, and spreading to other parts of the body through metastasis.
Send us all your questions or requests, and our expert team will assist you.
After completing curative treatment for cervical cancer, patients enter a phase of structured surveillance. The primary goal is the early detection of recurrence, as most recurrences occur within the first two years. The standard follow-up schedule involves physical examinations every 3 to 6 months for the first 2 years, then every 6 to 12 months through year 5.
These visits include a thorough symptom review—asking about leg swelling, pain, or bleeding—and a pelvic examination. For patients treated with radiation, pap smears are often less valuable due to radiation-induced cell changes, but HPV testing may still have a role. Imaging (CT or PET-CT) is not performed routinely for asymptomatic patients but is triggered by any suspicious findings on exam or new symptoms.
For patients treated with fertility-sparing surgery (trachelectomy), surveillance also includes monitoring the isthmus (the connection between the uterus and vagina) for stenosis or recurrence. Surveillance is a partnership; patient education on “red flag” symptoms ensures that any recurrence of disease is promptly evaluated between scheduled visits.
Treatment for cervical cancer often impacts ovarian function. Radical hysterectomy may preserve ovaries, but radiation therapy invariably destroys them if they are in the treatment field. This induces “surgical” or “medical” menopause, which occurs abruptly rather than gradually. Young women may experience sudden, severe hot flashes, night sweats, mood lability, and vaginal dryness.
Hormonal Replacement Therapy (HRT) is a critical component of survivorship care for these women. Unlike breast cancer, cervical cancer (specifically squamous cell carcinoma) is generally not hormone-sensitive. Therefore, HRT is safe and strongly recommended for young survivors to protect bone density (preventing osteoporosis) and cardiovascular health, in addition to managing menopausal symptoms.
For patients with adenocarcinoma, which can theoretically be estrogen-sensitive, the decision is more nuanced, but HRT is still often considered safe after a thorough risk-benefit discussion. Managing bone health also involves calcium and Vitamin D supplementation and weight-bearing exercise, as estrogen loss accelerates bone resorption.
Cervical cancer treatment significantly affects sexual function. Radical surgery can shorten the vagina, while radiation therapy causes fibrosis (scarring), stenosis (narrowing), and mucosal atrophy (dryness). These physical changes can lead to dyspareunia (painful intercourse) or the inability to engage in penetrative sexual activity.
Vaginal rehabilitation is a proactive part of care. Patients treated with radiation are prescribed the use of vaginal dilatants. These are graduated cylinders used to gently stretch the vaginal tissues, preventing them from sticking together and maintaining length and width. Regular use of dilators, starting shortly after treatment ends, is crucial for allowing future gynecologic exams and sexual intimacy.
Lubricants and vaginal moisturizers (non-hormonal or low-dose estrogen creams) address dryness. Beyond the physical, the psychological impact on body image and libido is profound. Counseling and referral to sex therapists help couples navigate intimacy after cancer, reframing sexuality in a way that accommodates the physical changes while maintaining connection.
The removal of pelvic lymph nodes (lymphadenectomy) or their irradiation disrupts the lymphatic drainage system of the legs. This can lead to lymphedema—the chronic accumulation of protein-rich fluid in the legs or genital region. Symptoms include swelling, heaviness, or tightness in one or both legs.
Prevention is key. Patients are educated on skin care to prevent infections (cellulitis), which can trigger or worsen lymphedema. This includes avoiding needle sticks or insect bites on the legs. If swelling occurs, early referral to a certified lymphedema therapist is vital.
Treatment involves Complete Decongestive Therapy (CDT), which includes manual lymphatic drainage massage, compression bandaging, and the use of custom-fitted compression garments (stockings). While lymphedema is a chronic condition, diligent management can keep the swelling under control and prevent severe disability.

A cervical cancer diagnosis carries a unique stigma due to its association with a sexually transmitted infection (HPV). Patients often grapple with feelings of shame, guilt, or anger towards partners. This emotional burden can lead to isolation and depression.
Psycho-oncology support is integrated into the care plan to normalize these feelings. Educating patients that HPV is ubiquitous and not a marker of promiscuity helps deconstruct the stigma. Support groups connect women with peers who share similar experiences, providing validation and practical advice on navigating survivorship.
Furthermore, because the disease affects women of reproductive age, fertility grief is a significant theme. Even if fertility-sparing surgery was attempted, the anxiety surrounding pregnancy or the loss of fertility requires specialized counseling. Addressing the “whole woman”—emotional, social, and physical—is the philosophy of modern survivorship care.
Send us all your questions or requests, and our expert team will assist you.
Radiation causes the tissues of the vagina to create scar tissue, which can make the vagina shorter, narrower, and less elastic. This can make pelvic exams and sexual intercourse painful or impossible. Using a dilator regularly (usually a few times a week) acts as physical therapy to keep the tissues flexible and open.
For the majority of cervical cancer survivors (those with squamous cell carcinoma), HRT is considered safe and is highly recommended if you have gone into early menopause. It does not increase the risk of cancer recurrence and protects your bones and heart. Discuss your specific pathology with your doctor.
Protect your legs from injury. Avoid tight clothing or jewelry that constricts the legs or groin. Keep your skin moisturized to prevent cracks. If you get a cut or insect bite on your leg, clean it immediately and watch for infection. Maintaining a healthy weight also lowers the risk of developing lymphedema.
“Normal” may look different, but a satisfying sex life is possible. It may require more preparation, such as using ample lubrication or moisturizers, and using positions that allow you to control the depth of penetration. Open communication with your partner and patience are key. Sexual rehabilitation therapy can be invaluable.
If you were treated with radiation, traditional Pap smears are often difficult to read. However, your doctor will perform a pelvic exam and may do an HPV test or a modified smear from the vaginal cuff every 3 to 6 months initially. The schedule depends on your specific treatment and risk factors, eventually spacing out to annual visits.

At Liv Hospital, we know how hard radicular pain can be. It’s caused by inflammation or compression of the spinal nerves in the cervical region.
Managing chronic neck pain or nerve irritation? A cervical epidural steroid injection might help. At Liv Hospital, we focus on you, using the newest methods
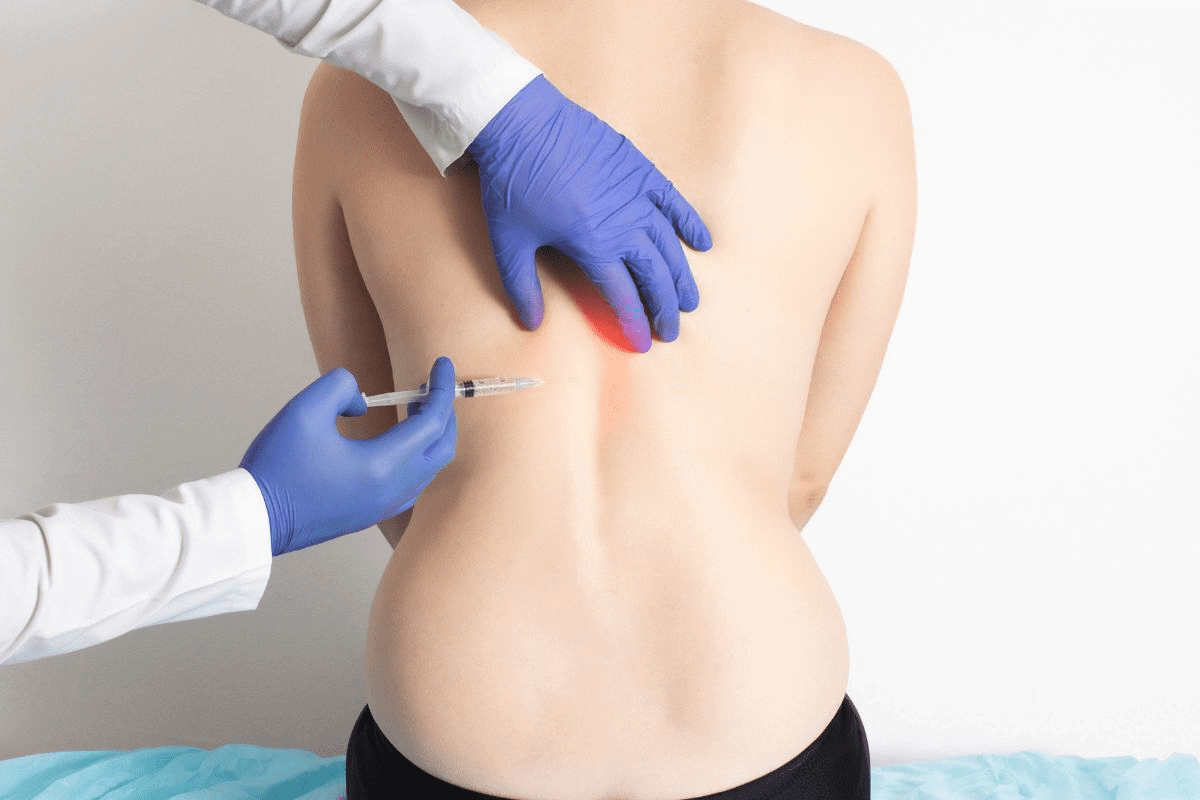
If you’re dealing with neck pain and symptoms that spread, a cervical epidural steroid injection might help. This treatment is good for issues like cervical
Managing chronic neck pain and cervical radiculopathy can be tough. Cervical epidural steroid injections (ESIs) offer a helpful solution. They reduce inflammation around the spinal
At Liv Hospital, we know how tough neck pain and radiculopathy can be. Cervical epidural steroid injections are a key treatment for these issues. These

Knowing what to expect after a cervical epidural steroid injection is key. It helps manage your hopes and ensures a smooth healing. We’ll look at

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)