Cancer involves abnormal cells growing uncontrollably, invading nearby tissues, and spreading to other parts of the body through metastasis.
Send us all your questions or requests, and our expert team will assist you.
The treatment of esophageal cancer represents a complex intersection of surgical precision, cytotoxic chemotherapy, ionizing radiation, and advanced immunotherapy. The therapeutic strategy is strictly stage-dependent. For very early mucosal disease, endoscopic therapies can preserve organ function. For locally advanced disease, the standard of care is multimodal, involving a “neoadjuvant” (pre-operative) approach to downstage the tumor before resection. For metastatic disease, the focus shifts to systemic control and palliation. The modern approach is highly personalized, integrating the patient’s physiological fitness with the tumor’s molecular profile.
Surgical resection, known as Esophagectomy, remains the cornerstone of curative treatment for fit patients with localized disease. However, it is a formidable procedure involving two or three body compartments (abdomen, chest, and neck). The goal is to remove the tumor-bearing esophagus and regional lymph nodes and reconstruct the gastrointestinal tract, typically by pulling the stomach up into the chest (gastric pull-up) to create a new conduit. Minimally Invasive Esophagectomy (MIE) and Robotic-Assisted Esophagectomy have revolutionized this field, utilizing small incisions and high-definition 3D visualization to reduce postoperative pain, pulmonary complications, and hospital stay duration compared to traditional open surgery.
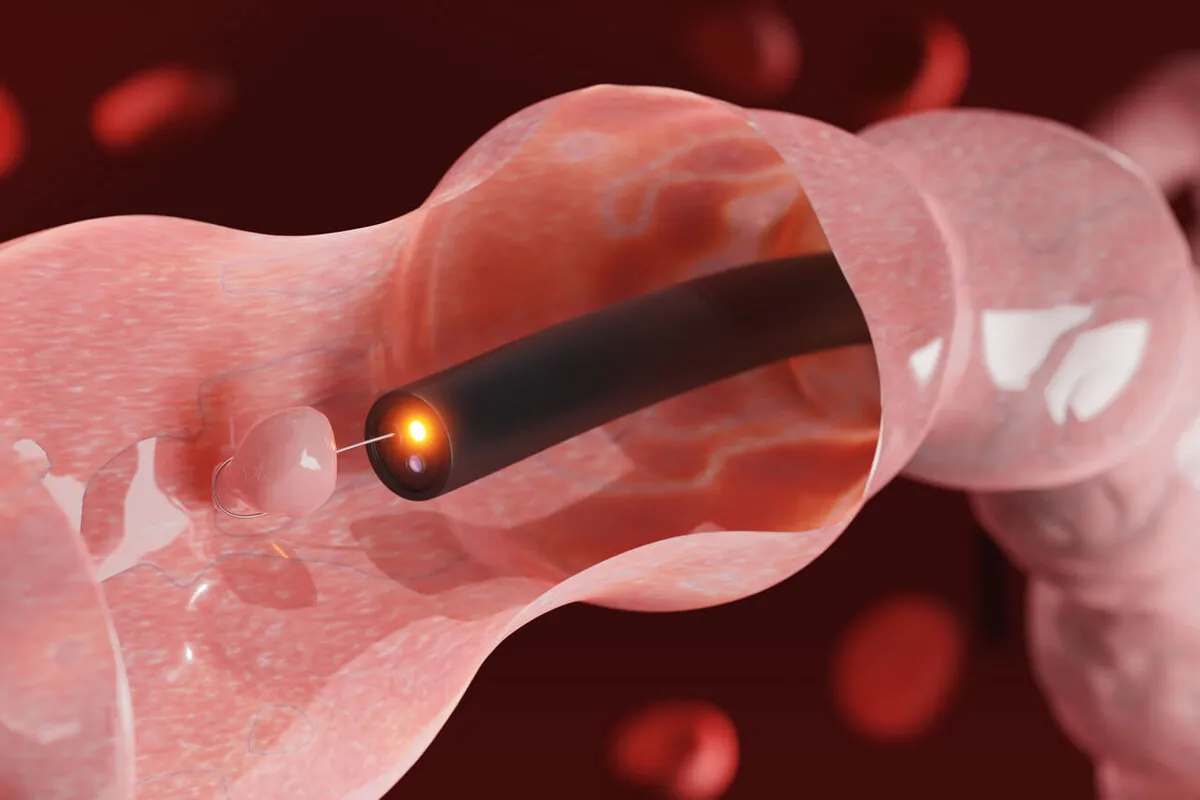
For tumors confined strictly to the mucosa (T1a), Endoscopic Mucosal Resection (EMR) or Endoscopic Submucosal Dissection (ESD) can be curative. These procedures are performed through an endoscope, lifting the tumor from the deeper muscle wall and shaving it off. This spares the patient the morbidity of an esophagectomy. Following resection, Radiofrequency Ablation (RFA) is often applied to the remaining Barrett’s esophagus segment to burn away any residual pre-cancerous cells, effectively “resetting” the esophageal lining. This regenerative approach relies on the body healing the ablated area with normal squamous epithelium in a non-acidic environment (controlled by acid-suppression medication).
or the majority of patients who present with locally advanced disease (tumor invading muscle or positive lymph nodes), surgery alone is insufficient. The standard of care is neoadjuvant chemoradiotherapy (often following protocols like the CROSS regimen). This involves concurrent administration of chemotherapy (e.g., carboplatin and paclitaxel) and radiation therapy for several weeks before surgery.
The rationale is threefold:
In some cases, particularly with Squamous Cell Carcinoma, patients may have a “complete clinical response” to chemoradiation, leading to debates about whether surgery is always necessary or if active surveillance (“watch and wait”) is a viable organ-preserving strategy.
Surgical Techniques and Approaches

In the metastatic setting, or for patients unable to undergo surgery, systemic therapy is the primary modality. Conventional chemotherapy (fluoropyrimidines, platinums, taxanes) targets rapidly dividing cells. However, the landscape is shifting towards immunotherapy. Immune Checkpoint Inhibitors (PD-1 inhibitors like nivolumab or pembrolizumab) are now approved for first-line treatment in combination with chemotherapy for advanced esophageal cancer. These drugs release the brakes on the immune system, allowing T-cells to recognize and attack the tumor.
Targeted therapies are used for specific molecular subtypes. HER2-positive adenocarcinomas are treated with trastuzumab, a monoclonal antibody that blocks the HER2 signaling pathway. Newer agents, including antibody-drug conjugates (ADCs) such as trastuzumab deruxtecan, offer potent options for patients who progress on initial therapies.
Palliative Interventions
The toxicity of esophageal cancer treatment is significant. Radiation can cause esophagitis (inflammation of the lining), making swallowing painful and requiring intense nutritional support. Chemotherapy can cause neuropathy, fatigue, and immune suppression. Post-esophagectomy complications can include anastomotic leaks (where the connection fails to heal), pneumonia, and atrial fibrillation. Managing these toxicities requires a proactive, supportive care team including dietitians, pain specialists, and physiotherapists to maintain the patient’s performance status and ability to complete the treatment course.


Send us all your questions or requests, and our expert team will assist you.
Neoadjuvant therapy refers to treatment given before the primary surgery. In esophageal cancer, this typically involves a combination of chemotherapy and radiation. The goal is to shrink the tumor, kill any cancer cells in the lymph nodes, and improve the chances of a successful, curative surgery.
Immunotherapy drugs, such as checkpoint inhibitors, do not kill cancer cells directly. Instead, they block proteins that cancer cells use to hide from the immune system. This allows the patient’s own white blood cells (T-cells) to recognize and attack the cancer more effectively. It is often used in advanced stages or after surgery.
An esophageal stent is a flexible, mesh-like tube (usually metal) that is placed inside the esophagus using an endoscopy. It expands against the walls of the esophagus to push the tumor aside and keep the pathway open, allowing patients with advanced cancer to swallow food and liquids more easily.
Robotic surgery is a form of minimally invasive surgery that allows for greater precision and 3D visualization. Compared to traditional open surgery (large incisions), it typically results in less blood loss, less pain, fewer lung complications, and a faster recovery. However, the long-term cancer cure rates are generally similar between the two approaches.


Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)