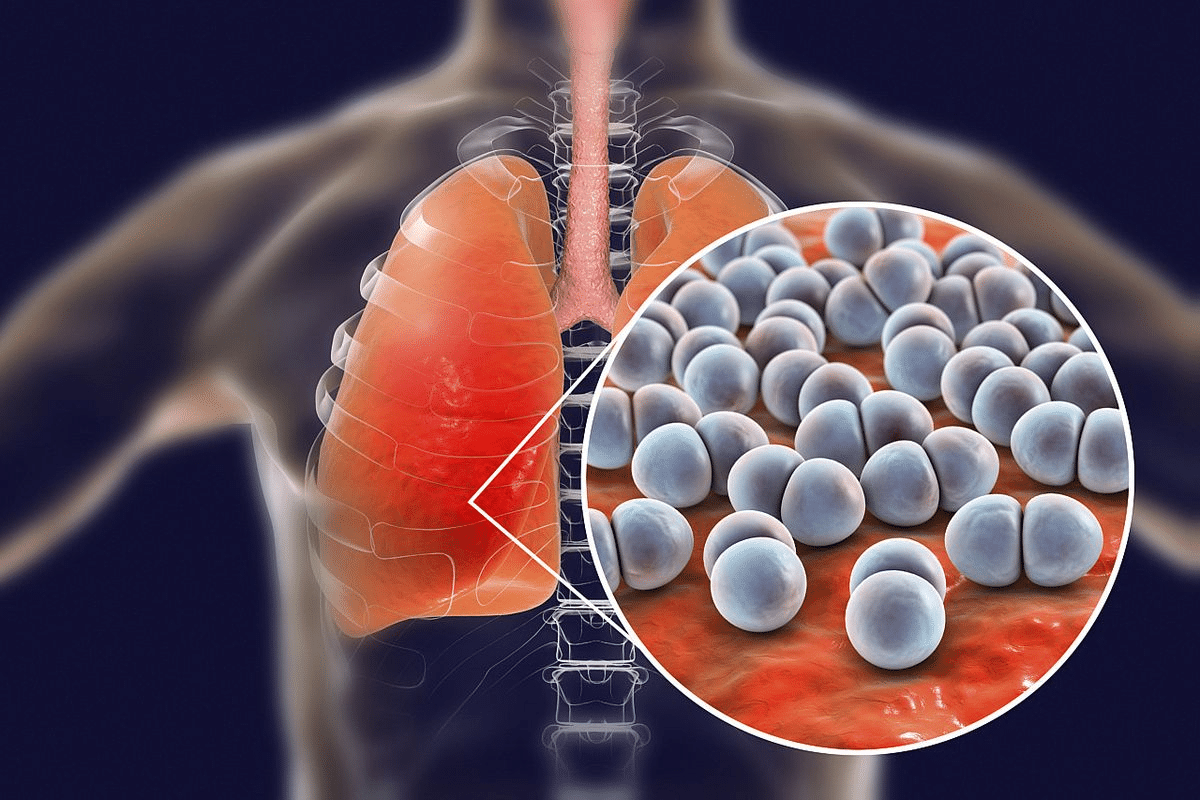
Detailed cap disease definition, covering its infectious etiology and the common pathogens involved in its development. Community-acquired pneumonia (CAP) is a serious lung infection that happens outside hospitals. It’s a big problem worldwide, causing a lot of sickness and death.
CAP happens when harmful germs settle in the lungs, causing inflammation and fluid buildup. This makes it hard for the lungs to work right. It’s a sudden lung infection, and how bad it is depends on the germ and the person’s health.
Knowing about CAP is key to spotting it early and treating it fast. This can really help patients get better. At Liv Hospital, we have teams of experts working together to care for CAP patients.
Key Takeaways
- Community-acquired pneumonia (CAP) is a serious lower respiratory tract infection.
- CAP is a leading cause of illness and death worldwide.
- The condition occurs when pathogenic microorganisms colonize the alveoli.
- Early recognition and timely treatment are key to better patient outcomes.
- Liv Hospital offers full care for CAP patients.
Understanding Community Acquired Pneumonia (CAP) Disease Definition
Grasping Community Acquired Pneumonia (CAP) means knowing its medical definition and key features. CAP is pneumonia caught outside a hospital or without recent hospital stay. This is key for diagnosis, treatment, and prevention.
Medical Definition of CAP
Community Acquired Pneumonia is pneumonia caught outside a hospital. It’s not from recent hospital stay or healthcare exposure. Symptoms include cough, fever, and trouble breathing, with lung infection signs on X-rays.
We diagnose CAP by symptoms and chest X-rays. It can be caused by bacteria, viruses, or fungi. Knowing this helps pick the right tests and treatments.
Distinguishing CAP from Other Types of Pneumonia
It’s important to tell CAP apart from other pneumonias. Hospital-acquired pneumonia (HAP) happens in those hospitalized over 48 hours. It’s caused by tougher germs due to hospital settings. Healthcare-associated pneumonia (HCAP) is for those recently in healthcare.
|
Type of Pneumonia |
Setting |
Common Pathogens |
|---|---|---|
|
CAP |
Community |
Streptococcus pneumoniae, Haemophilus influenzae |
|
HAP |
Hospital |
Pseudomonas aeruginosa, MRSA |
|
HCAP |
Healthcare settings |
Varied, including resistant strains |
Common Terminology and Abbreviations
In CAP, you’ll see CAP, HAP, and HCAP often. CAP means Community Acquired Pneumonia. HAP is Hospital-Acquired Pneumonia. HCAP is Healthcare-Associated Pneumonia. Knowing these helps doctors talk clearly.
The term C/A/P means Community Acquired Pneumonia. It’s key to understand this to read medical texts and patient records well. CAP is a big cause of sickness and death worldwide, as Wikipedia notes.
The Global Burden of Community Acquired Pneumonia
Community-acquired pneumonia (CAP) is a big problem worldwide. It affects people of all ages and in many places. This makes it a big worry for public health.
Worldwide Incidence and Prevalence
The number of CAP cases varies a lot around the world. It can range from 1.5 to 14 cases per 1000 people each year. The Global Burden of Disease reports say it caused 2.49 million deaths globally.
Epidemiological studies show CAP hits harder on the elderly and those with health issues. Knowing this helps us focus our efforts better.
CAP in the United States: Statistics and Demographics
In the U.S., CAP is a big reason for hospital stays and deaths, mainly among the elderly. It affects about 5.5 million adults each year, with many needing hospital care.
|
Age Group |
Incidence Rate (per 1000 person-years) |
Hospitalization Rate (%) |
|---|---|---|
|
18-64 years |
2.46 |
15.6 |
|
65-79 years |
6.78 |
34.5 |
|
80+ years |
14.03 |
54.2 |
Economic and Healthcare Impact
CAP costs a lot, with over $10 billion spent each year in the U.S. This includes hospital bills, doctor visits, and lost work time. It also leads to a lot of hospital visits and deaths among the elderly.
It’s key to understand CAP’s global impact to fight it better. By looking at how common it is, how it affects people, and its costs, we can do better for patients.
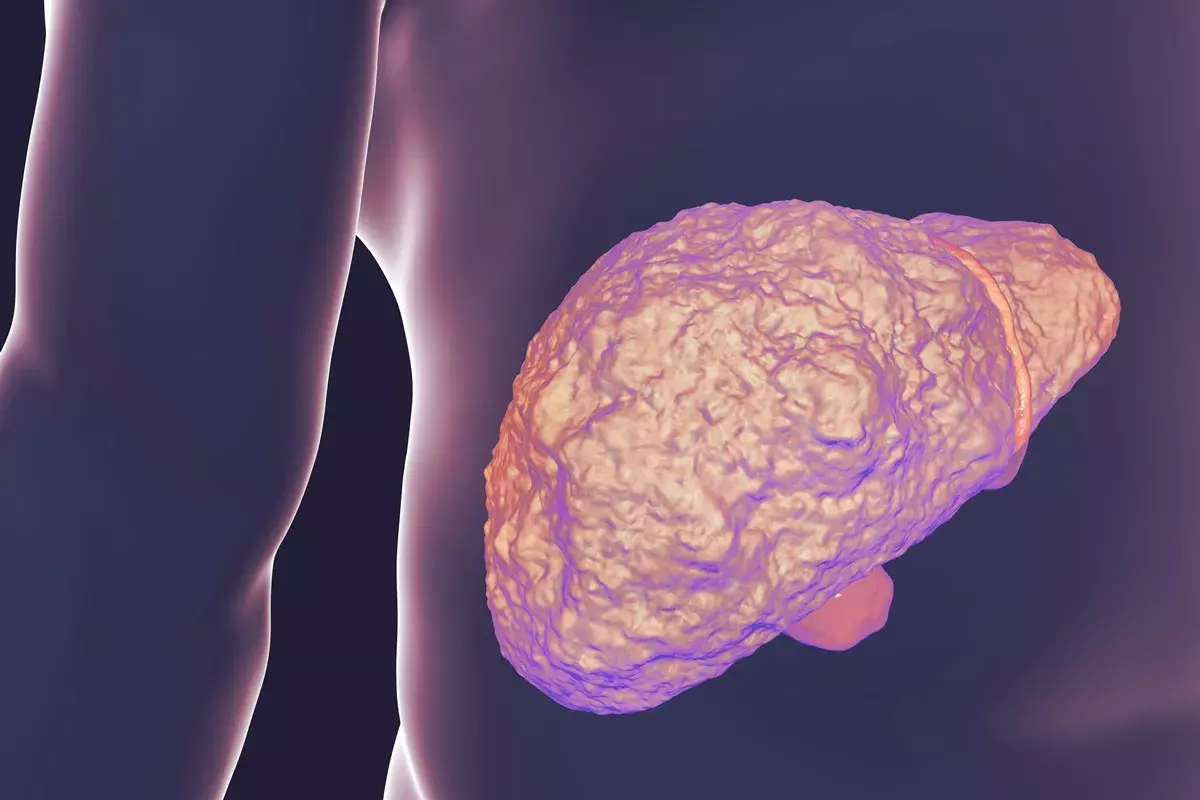
Pathophysiology of Community Acquired Pneumonia
Community Acquired Pneumonia (CAP) happens when the lungs can’t fight off infections. This is due to many factors, like how harmful the pathogen is and how well the body’s immune system responds.
Infection Development in the Lungs
Bacteria can get into the lungs in a few ways. The most common is micro-aspiration, where tiny bits of saliva are breathed in. Macro-aspiration is when more is aspirated, often in people who can’t swallow well or are very sleepy.
Another way is through the blood, called hematogenous spread. This is less common but very serious. Knowing how CAP starts is key to understanding it.
Inflammatory Response and Alveolar Damage
When bacteria get into the lungs, they start an inflammatory response. This brings in neutrophils and releases cytokines and chemokines to fight the infection. But, this fight can also damage the alveoli, making it hard to breathe.
The fight between the body’s defenses and the pathogen’s strength decides the infection’s outcome. If the body’s response is too strong, it can lead to serious problems.
Host Defense Mechanisms
Our body’s defenses are key in preventing and fighting CAP. These include physical barriers and immune responses. People with weak immune systems are more likely to get CAP.
It’s important to understand how the pathogen and the body’s defenses interact. This helps in finding better ways to prevent and treat CAP.
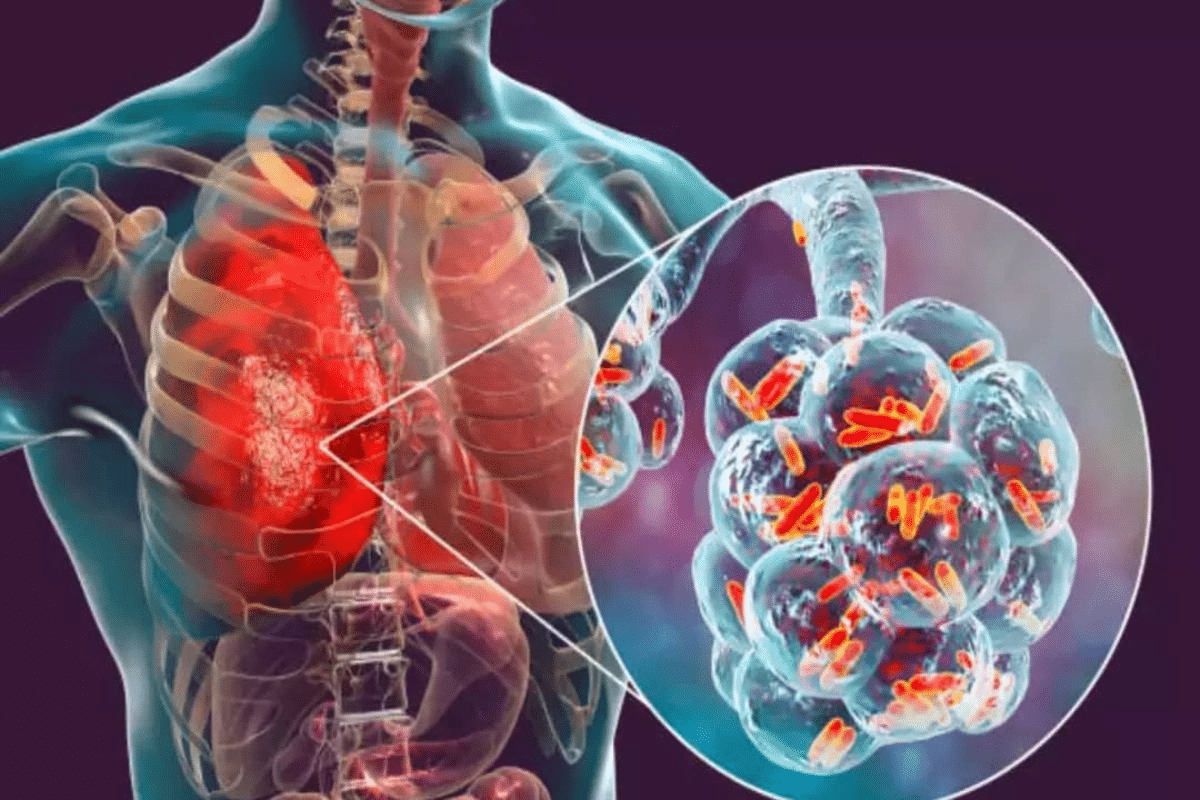
Etiology of Community Acquired Pneumonia
Community Acquired Pneumonia (CAP) has many causes. These include bacteria, viruses, and fungi. Knowing what causes it helps doctors diagnose and treat it better.
Bacterial Causes
Bacteria are the main culprits behind CAP. Streptococcus pneumoniae is the top offender. Other big players are Haemophilus influenzae and Moraxella catarrhalis.
|
Bacterial Pathogen |
Prevalence |
Clinical Significance |
|---|---|---|
|
Streptococcus pneumoniae |
High |
Most common cause of CAP, associated with severe disease |
|
Haemophilus influenzae |
Moderate |
Often seen in patients with underlying conditions |
|
Moraxella catarrhalis |
Moderate |
Common in patients with COPD |
Viral Causes
Viruses are also big players in CAP, mainly in certain groups. Influenza virus is a big one, during outbreaks. Other viruses like Respiratory Syncytial Virus (RSV) and Adenovirus also play a part.
Fungal and Atypical Pathogens
Fungi like Histoplasma capsulatum and Coccidioides spp. are less common but important in certain areas. Atypical bacteria, like Mycoplasma pneumoniae and Chlamydophila pneumoniae, also cause CAP.
It’s key to look at all these causes when treating CAP. This ensures the best care for patients.
Classification Systems for CAP
Classification systems for Community Acquired Pneumonia (CAP) are key. They help doctors figure out how serious the disease is and how to treat it. These systems also help spot patients who need extra care.
Severity-Based Classification
Severity-based systems are used a lot to check how bad CAP is. The CURB-65 score is a big help. It looks at five things: Confusion, Uremia, Respiratory rate, Blood pressure, and age 65 or older.
The CURB-65 score gives points for each of these. It helps doctors decide if a patient needs to be in the hospital or not.
Pathogen-Based Classification
Pathogen-based classification finds out what caused the pneumonia. This is important for choosing the right antibiotics. Common culprits include Streptococcus pneumoniae, Haemophilus influenzae, and viruses.
Tests like PCR and serology help find the cause. This is key when the usual suspects don’t work or when atypical pathogens are suspected.
Clinical Setting Classification
Clinical setting classification looks at where the pneumonia was caught. This matters because the likely cause and treatment can differ.
Healthcare-associated pneumonia might need stronger antibiotics because of resistant bugs. Community-acquired pneumonia might get more targeted treatment based on local bugs and resistance.
Key Classification Systems:
- Severity-based classification (e.g., CURB-65 score)
- Pathogen-based classification
- Clinical setting classification
Using these systems helps doctors make better choices for treating CAP. This leads to better results for patients.
Risk Factors for Developing CAP
It’s important to know the risk factors for Community Acquired Pneumonia (CAP). This helps us spot who’s at higher risk and take steps to prevent it. CAP can hit anyone, but some factors make it more likely.
Age-Related Risk Factors
Age is a big risk factor for CAP. Older adults and young children are more at risk because their immune systems are weaker. Older adults might have other health issues that make fighting infections harder. Young children’s immune systems are not fully grown yet.
Underlying Medical Conditions
People with certain health conditions are more likely to get CAP. For example, chronic obstructive pulmonary disease (COPD), heart disease, and diabetes can weaken the body’s defense against infections.
|
Underlying Condition |
Risk Level |
Reason |
|---|---|---|
|
COPD |
High |
Damaged lungs are more susceptible to infection. |
|
Heart Disease |
Moderate to High |
Reduced cardiac output can impair lung function. |
|
Diabetes |
Moderate |
Impaired immune response due to high blood sugar levels. |
Lifestyle and Environmental Factors
Lifestyle and environment also affect CAP risk. Smoking and air pollution can harm lung health, making it easier to get sick.
Community and Social Determinants
Community and social factors, like socioeconomic status and access to healthcare, also matter. People with lower income might find it hard to get medical care on time.
Knowing these risk factors helps doctors find and help those at risk. They can then take steps to prevent CAP.
Clinical Manifestations and Symptoms
CAP symptoms can vary from mild to severe. This requires a careful approach to diagnosis and treatment. The symptoms of CAP depend on the pathogen, the patient’s age, and their health.
Common Symptoms of CAP
The usual signs of CAP include cough, fever, and shortness of breath. Other symptoms like fatigue, headache, and muscle pain can also occur. Some people may feel chest pain that gets worse when they breathe deeply or cough.
- Cough, which may be productive or non-productive
- Fever, often accompanied by chills
- Shortness of breath or difficulty breathing
- Chest pain or discomfort
- Fatigue or feeling weak
Atypical Presentations in Special Populations
Some groups, like the elderly or those with weak immune systems, may show different symptoms of CAP. Older adults might have confusion or altered mental status instead of typical respiratory symptoms. People with health issues may see their symptoms get worse.
Severity Indicators and Warning Signs
It’s important to know the signs of severe CAP. These signs need quick medical help. Some warning signs include:
- Severe difficulty breathing
- Chest pain or pressure
- Cyanosis (a bluish discoloration of the skin)
- Confusion or altered mental status
- High fever that is not responding to treatment
Patients and caregivers should watch for these signs. This way, they can get medical help fast.
Diagnosis and Assessment of CAP
To diagnose Community Acquired Pneumonia (CAP), we use a mix of clinical checks, lab tests, and imaging. We’ll look at how CAP is diagnosed, aiming for a full understanding of this condition.
Physical Examination Findings
A detailed physical check is key in spotting CAP. We search for fever, fast breathing, and sounds like crackles in the lungs. These signs suggest pneumonia and guide further tests. The check also helps figure out how serious the CAP is and if the patient needs to be in the hospital.
A medical expert says, “A careful physical check is vital for patients with suspected CAP. It gives important info on the illness’s severity and helps decide the first steps in treatment.”
“The physical check should cover vital signs, lung sounds, and signs of breathing trouble.”
Laboratory Tests and Biomarkers
Lab tests are essential in diagnosing and managing CAP. We often do tests like a complete blood count (CBC), blood cultures, and sputum analysis. Biomarkers like C-reactive protein (CRP) and procalcitonin help diagnose CAP and guide antibiotic use.
- CBC to check white blood cell count
- Blood cultures to spot bacteremia
- Sputum analysis to find the pathogen
Imaging Studies
Imaging, like chest X-rays, is vital in diagnosing CAP. Chest X-rays confirm pneumonia, show how much of the lung is affected, and spot complications like pleural effusion. Chest X-rays are a key tool in managing the condition.
Microbiological Diagnosis
Identifying the pathogen in CAP is critical. We use Gram stain, culture, and molecular tests to find bacteria, viruses, or other pathogens. This info is key for targeted antibiotic treatment and better patient care.
|
Diagnostic Method |
Purpose |
|---|---|
|
Gram stain |
Rapid identification of bacteria |
|
Culture |
Identification of causative pathogen |
|
Molecular tests |
Detection of specific pathogens |
Treatment Approaches for Community Acquired Pneumonia
Community-acquired pneumonia (CAP) needs a full treatment plan. This includes antibiotics and supportive care. We will look at different treatment methods, like antibiotic choices and when to stay in the hospital or go home.
Antibiotic Therapy Guidelines
Antibiotics are key in treating CAP. Empiric antibiotic treatment starts based on the likely cause and how sick the patient is. The right antibiotics depend on several things, like health conditions and the risk of drug-resistant bacteria.
For healthy patients with mild CAP, amoxicillin or doxycycline are often recommended. But for those who are sicker or at risk for resistant bacteria, stronger antibiotics like fluoroquinolones or beta-lactam plus macrolide combinations are suggested.
Outpatient vs. Inpatient Management
Deciding if a patient should stay home or go to the hospital depends on how sick they are. Tools like the Pneumonia Severity Index (PSI) or CURB-65 score help doctors make this choice.
Patients with mild CAP and few health issues can usually stay home. But those with severe disease or serious health problems might need to be in the hospital for better care.
Supportive Care Measures
Supportive care is also vital in treating CAP. This includes oxygen for those with low oxygen levels, staying hydrated, and eating well. Managing pain is also important, as CAP can be very uncomfortable.
Treatment in Special Populations
Some groups, like the elderly, pregnant women, and those with weakened immune systems, need special care for CAP. For example, older adults might need stronger treatment because they’re at higher risk for problems. Pregnant women need antibiotics that are safe for both them and their baby.
Knowing these special needs is key to giving the best care for CAP patients. Tailoring treatment to each patient can lead to better outcomes and fewer complications.
Prevention Strategies and Conclusion
Preventing community acquired pneumonia (CAP) is key to lowering its global impact. We can do this by using vaccines and making lifestyle changes. Vaccines against pneumococcal disease and flu are very effective in stopping CAP, mainly in those at high risk.
Living a healthy lifestyle also helps. Not smoking and eating well can lower your chance of getting CAP. These steps are vital in our fight against CAP.
We’ve talked about CAP a lot. We’ve covered what it is, its global impact, how it works, who gets it, and how to treat it. Knowing these details helps us prevent and manage CAP better.
In short, stopping CAP is a big job that needs vaccines, healthy living, and good care. If we all work together, we can make CAP less common. This will help patients feel better and live better lives.
FAQ
What is community-acquired pneumonia (CAP)?
Community-acquired pneumonia (CAP) is a serious lung infection. It happens outside hospitals and is caused by bacteria, viruses, and fungi.
What are the common causes of CAP?
Common causes of CAP include bacteria like Streptococcus pneumoniae and viruses like influenza. Haemophilus influenzae and Moraxella catarrhalis are also common bacteria.
How is CAP distinguished from other types of pneumonia?
CAP is different from other pneumonias because it occurs outside hospitals. This makes it a community-acquired infection.
What are the risk factors for developing CAP?
Several factors increase the risk of CAP. These include age, health conditions, lifestyle, and environmental factors. Smoking and exposure to pollutants are also risks.
What are the common symptoms of CAP?
Symptoms of CAP include cough, fever, and chest pain. Difficulty breathing is also common. Some people, like older adults, may have different symptoms.
How is CAP diagnosed?
Doctors diagnose CAP through physical exams, lab tests, and imaging. They look for signs of infection and its cause.
What is the treatment for CAP?
Treatment for CAP includes antibiotics and supportive care. Antibiotics are chosen based on the cause. Supportive care helps manage symptoms and prevent complications.
Can CAP be prevented?
Yes, CAP can be prevented. Vaccines and lifestyle changes help. Vaccines protect against certain causes. Healthy habits reduce risk.
What is the global burden of CAP?
CAP is a major cause of illness and death worldwide. It has a big impact on healthcare and the economy. It affects vulnerable groups like older adults and young children.
How is CAP classified?
CAP is classified in different ways. These include severity, pathogen, and setting. Classification helps guide treatment and management.
What is the role of antibiotic therapy in CAP treatment?
Antibiotics are key in treating CAP. Guidelines suggest specific antibiotics based on the cause. Starting treatment quickly is important for better outcomes.
When is hospitalization necessary for CAP?
Hospitalization is needed for severe CAP cases. This includes those needing close monitoring, intravenous antibiotics, or oxygen therapy. It’s also for those with severe symptoms or complications.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7119140/