Identify key lung disease symptoms and understand your risk factors. Learn early warning signs, pediatric risks, and prevention strategies at LIV Hospital.
Send us all your questions or requests, and our expert team will assist you.
A cough is the body’s natural reflex to clear the airways of mucus and irritants. However, a cough that lasts longer than eight weeks is considered chronic and requires evaluation. It can be dry or productive, meaning it produces phlegm.
Common causes include postnasal drip, asthma, and acid reflux. It can also be a sign of more serious conditions like chronic obstructive pulmonary disease (COPD) or lung fibrosis.
Persistent coughing can disrupt sleep and cause physical exhaustion. Identifying the underlying trigger is the first step toward relief.
Dyspnea is the uncomfortable sensation of not getting enough air. It is often described as air hunger or chest tightness. It can occur during physical exertion or while at rest.
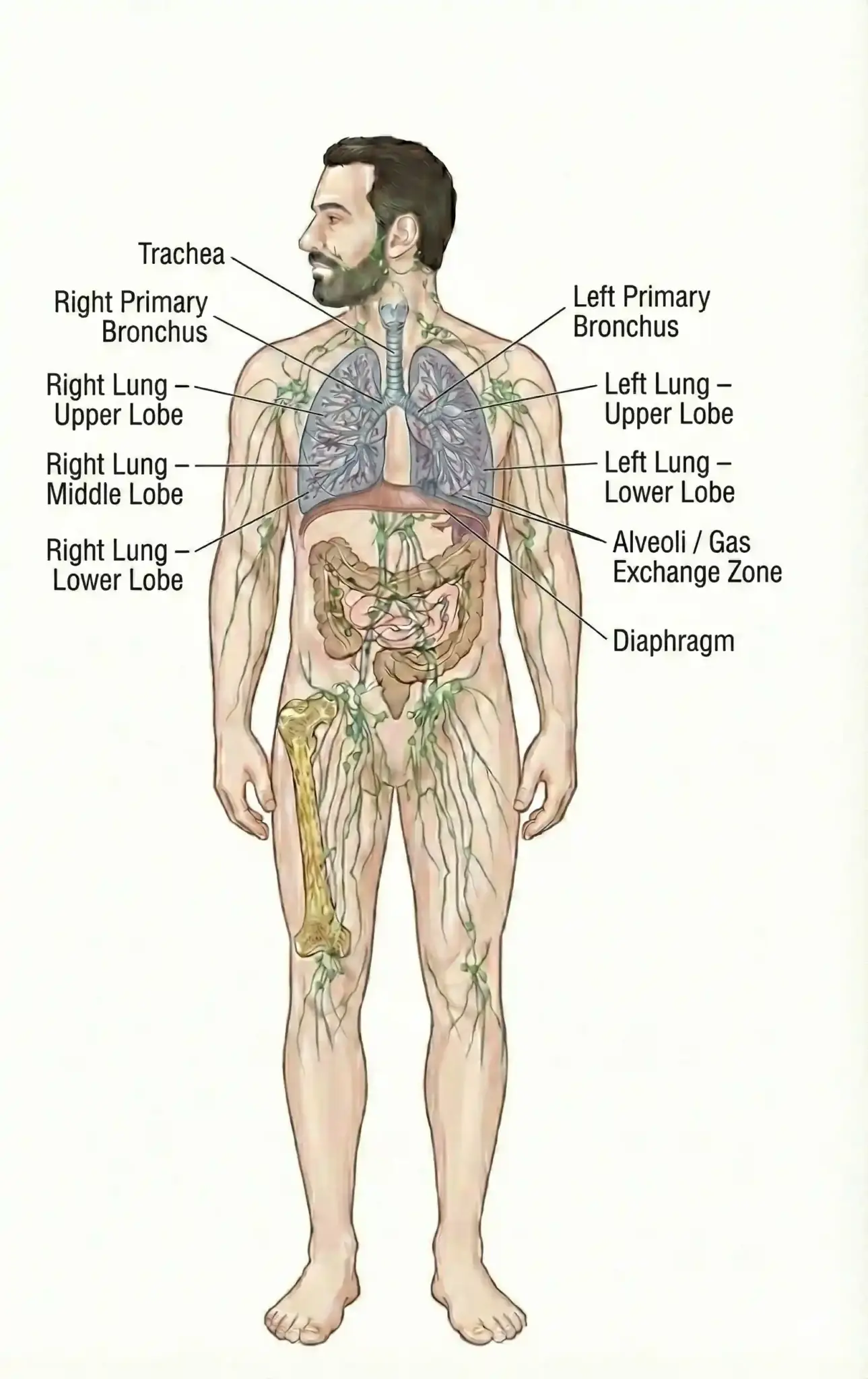
This symptom is a hallmark of many respiratory and cardiac conditions. In the context of lung health, it often indicates an obstruction in the airways or a problem with gas exchange.
Sudden-onset dyspnea is a medical emergency. Chronic dyspnea develops slowly and may be dismissed by patients as a sign of aging or lack of fitness.
Chest pain related to lung issues often feels sharp and worsens with deep breathing or coughing. This is known as pleuritic chest pain. It suggests inflammation of the lung lining.
Tightness or pressure in the chest can be a symptom of asthma or bronchospasm. It feels like a band is tightening around the ribcage, restricting the ability to take a full breath.
Differentiating lung pain from heart pain is critical. Lung pain is usually influenced by breathing, whereas heart pain is often constant or worsens with exertion.

Wheezing is a high-pitched whistling sound made while breathing. Narrowed airways cause it and are most often heard during exhalation. It is a classic sign of asthma and COPD.
Stridor is a harsh, vibrating noise heard during inhalation. It indicates an obstruction in the upper airway, such as the trachea or larynx. This is often a medical emergency.
Crackles or rales are bubbling sounds heard with a stethoscope. They indicate fluid in the tiny air sacs, common in pneumonia or heart failure.
Sputum, or phlegm, is mucus produced by the lungs. While some mucus is normal for protection, excessive production indicates inflammation or infection. The color and consistency can provide diagnostic clues.
Clear or white mucus is often seen in asthma or viral infections. Yellow or green mucus typically signals a bacterial infection. Thick, sticky mucus is characteristic of conditions like cystic fibrosis.
Chronic bronchitis is defined by a daily productive cough for months at a time. Managing mucus clearance is vital to prevent secondary infections.
Coughing up blood is a frightening symptom that always warrants immediate medical attention. It can range from blood-streaked sputum to coughing up large amounts of pure blood.
Common causes include severe infection, bronchitis, or lung cancer. It can also be caused by a blood clot in the lung, known as a pulmonary embolism.
The source of the bleeding must be identified quickly. It usually indicates damage to the blood vessels within the bronchial tubes or lung tissue.
Chronic lung disease forces the body to work harder to breathe. This increased work of breathing consumes a significant amount of energy, leading to persistent fatigue.
Low oxygen levels, or hypoxemia, deprive the muscles and brain of the fuel they need. This results in lethargy, difficulty concentrating, and weakness.
Patients may find they need to rest after simple tasks like showering or dressing. Addressing oxygen levels often improves energy and mental clarity.
Many respiratory problems manifest during sleep. Loud snoring and gasping for air are signs of obstructive sleep apnea. This interrupts the sleep cycle and lowers oxygen levels.
Morning headaches are a common symptom of high carbon dioxide levels during sleep. This suggests hypoventilation, where the patient is not breathing deeply enough at night.
Restless sleep and excessive daytime sleepiness are consequences of poor respiratory control at night. These symptoms affect overall health and safety.
Air pollution is a significant risk factor for developing and worsening lung disease. Particulate matter from vehicle exhaust and industrial emissions can penetrate deep into the lungs.
Indoor allergens such as dust mites, mold, and pet dander are common asthma triggers. Poor ventilation in homes can trap these irritants.
Seasonal allergens, such as pollen, cause inflammation in the airways. Understanding environmental triggers helps manage symptoms and prevent flare-ups.
Air pollution is a significant risk factor for developing and worsening lung disease. Particulate matter from vehicle exhaust and industrial emissions can penetrate deep into the lungs.
Indoor allergens such as dust mites, mold, and pet dander are common asthma triggers. Poor ventilation in homes can trap these irritants.
Seasonal allergens, such as pollen, cause inflammation in the airways. Understanding environmental triggers helps manage symptoms and prevent flare-ups.
Genetics plays a role in susceptibility to lung diseases. Alpha-1 antitrypsin deficiency is a genetic condition that predisposes individuals toearly-onsett COPD, even if they have never smoked.
Cystic fibrosis is an inherited disorder that causes thick, sticky mucus to build up in the lungs. It requires lifelong management.
A family history of asthma or lung cancer also increases an individual’s risk. Genetic screening can help identify those who need closer monitoring.
Specific jobs expose workers to substances that damage the lungs. Construction workers exposed to asbestos are at risk for mesothelioma and asbestosis.
Miners exposed to coal dust can develop black lung disease. Farmers are at risk of developing hypersensitivity pneumonitis from moldy hay and grain dust.
Healthcare workers may be exposed to infectious respiratory diseases. Proper protective equipment and safety regulations are essential for preventing occupational lung disease.
Respiratory infections are common triggers for exacerbations of chronic lung disease. A simple cold can lead to a severe asthma attack or a COPD flare-up.
Viral infections like influenza and RSV cause inflammation in the airways. Bacterial pneumonia can cause fluid buildup and lung consolidation.
Fungal infections can occur in individuals with weakened immune systems. Vaccination and hygiene are key preventative measures against these triggers.
Lung health is often connected to other body systems. Rheumatoid arthritis and lupus can cause inflammation in the lung tissue or lining. This is known as interstitial lung disease.
Heart failure can cause fluid to back up into the lungs, causing pulmonary edema. Neuromuscular diseases like ALS can weaken the muscles used for breathing.
Kidney failure can also lead to fluid overload in the lungs. A holistic approach is needed to manage these interconnected conditions.
Knowing when to seek help is vital. Patients often search for pulmonology near me when symptoms become persistent or interfere with daily life. A cough lasting more than a few weeks or unexplained shortness of breath warrants a visit.
Finding a pulmonology doctor near me is crucial for managing chronic conditions. Regular checkups can prevent rapid decline and manage acute flare-ups.
Immediate care should be sought for chest pain, coughing up significant blood, or severe difficulty breathing. Early intervention preserves lung function.
Send us all your questions or requests, and our expert team will assist you.
A cough is considered chronic if it lasts eight weeks or longer in adults or four weeks in children, and a medical professional should evaluate it.
Chronic low oxygen levels can strain the right side of the heart, which pumps blood to the lungs; when it becomes overworked, fluid can back up and pool in the legs and ankles.
Yes, anxiety can trigger hyperventilation or a feeling of air hunger, but it is essential to rule out physical lung causes before attributing the symptom solely to anxiety.
While vaping eliminates the combustion of tobacco, it introduces other harmful chemicals and ultrafine particles into the lungs that can cause severe inflammation and permanent damage.
Clubbing is a physical sign in which the fingertips become enlarged, and the nails curve around the tips; it is often associated with chronic low oxygen levels and lung diseases.


Conjunctivochalasis is a common eye condition. It causes extra folds in the conjunctiva, which can mess up tear flow and drainage. Over 98% of people

Nearly 20% of Americans have skin sensitivity or allergic reactions to skincare or cosmetics. It’s key to know why a skin sensitivity test is important.Explaining

Getting a correct diagnosis for groin hernias is key for good treatment. Femoral hernias are rare, making up about 3 to 5 percent of all
At Liv Hospital, we’re always looking for new ways to fight cancer. Frequent cancer therapy is one of these methods. It uses special electromagnetic waves

Down syndrome, also known as Trisomy 21, is a congenital anomaly. It is a genetic condition that people are born with. It happens when there

Many people get confused about the difference between arthrosis and osteoarthritis. It’s important to know the difference to take care of your joints. Arthrosis is

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)