Last Updated on October 21, 2025 by mcelik

We are seeing a big change in treating some blood cancers with CAR T therapy. It’s a new kind of immunotherapy. It uses a patient’s own T cells to find and kill cancer cells.
CAR T cell therapy has changed how we fight cancer. More than 30,000 patients worldwide have been treated. It’s a personalized way to fight blood cancers like leukemia and lymphoma.
At Liv Hospital, we aim to give top-notch healthcare. We support patients from all over with our care. Our approach to CAR-T cell therapies focuses on the patient. We make sure patients get the best care possible.
Key Takeaways
- CAR T therapy is a revolutionary form of immunotherapy.
- Over 30,000 patients have been treated with CAR T cell therapy globally.
- CAR T cell therapy targets and destroys cancer cells.
- Liv Hospital offers a patient-centered approach to CAR-T cell therapies.
- CAR T therapy has shown significant promise in treating leukemia and lymphoma.
Understanding the Revolutionary Car T Therapy Approach
CAR-T therapy changes T-cells to fight cancer. It’s a new way to treat blood cancers that other treatments can’t touch.
How Chimeric Antigen Receptor Technology Works
CAR-T cell therapy uses chimeric antigen receptor (CAR) technology. It makes T-cells find and attack cancer cells. Here’s how:
- Extracting T-cells from the patient’s blood
- Genetically modifying these T-cells to produce CARs that can identify specific antigens on cancer cells
- Expanding the modified T-cells
- Reinfusing them back into the patient
After being put back in the body, CAR-T cells keep fighting cancer. They do this without harming healthy cells much. This makes treatments less harsh.
The Process of Engineering Patient T-Cells
Engineering T-cells is a detailed process. It involves several steps:
- T-cell extraction: T-cells are taken from the patient’s blood or bone marrow.
- Genetic modification: The T-cells are then changed to make CARs. This lets them find cancer cells. Viral vectors help add the CAR gene.
- Expansion: The modified T-cells grow in number. This makes sure there’s enough for treatment.
- Quality control: Before being given back to the patient, the CAR-T cells are tested. This checks if they’re safe and work well.
A study in Nature shows CAR-T cell therapy is a game-changer. It helps patients who’ve tried other treatments without success.
Being able to make T-cells target cancer opens new doors in treatment. As research grows, CAR-T cell therapy will likely help more people with cancer.
The History and Evolution of CAR-T Cell Technology
The journey of CAR-T cell therapy has been incredible. It started as an idea and now offers advanced treatments for blood cancers. This progress is a big step forward in fighting cancer.
From Laboratory Concept to Clinical Reality
For decades, CAR-T cell therapy was just an idea. But turning it into a real treatment took time. Early research focused on understanding T-cell biology and developing methods to genetically modify these cells. The first trials began a new chapter in cancer treatment, giving hope to many.
Key Scientific Breakthroughs in Development
Several breakthroughs have pushed CAR-T cell therapy forward. One big step was the creation of chimeric antigen receptor (CAR) technology. This lets T-cells target cancer cells better. Also, better gene editing tools and T-cell expansion techniques have made CAR-T cell therapies more effective and safe.
The growth of CAR-T cell therapy is marked by key milestones:
| Year | Milestone | Description |
|---|---|---|
| 1990s | Initial Concept | First ideas for using genetically modified T-cells to fight cancer. |
| Early 2000s | CAR Technology Development | Improvements in chimeric antigen receptor technology. |
| 2010s | First Clinical Trials | First trials showed CAR-T cell therapy’s success. |
| 2017 | FDA Approval | First FDA approval of a CAR-T cell therapy (Kymriah). |
The story of CAR-T cell technology is a big part of cancer treatment’s history. As research keeps going, CAR-T cell therapy’s impact on blood cancer patients will only grow.
FDA-Approved CAR-T Cell Therapies: The Complete List
The FDA has approved several CAR-T cell therapies. These treatments are changing how we fight blood cancers. They have shown to be safe and effective in clinical trials.
Kymriah (Tisagenlecleucel): First FDA-Approved Treatment
Kymriah was the first CAR-T cell therapy to get FDA approval. It’s a big deal in the medical world. It treats certain acute lymphoblastic leukemia (ALL) and diffuse large B-cell lymphoma (DLBCL). It works by targeting the CD19 antigen on cancer cells.
Yescarta (Axicabtagene Ciloleucel): Expanding Options
Yescarta is another FDA-approved CAR-T cell therapy. It’s mainly for DLBCL and some non-Hodgkin lymphomas. Like Kymriah, it targets the CD19 antigen, giving patients a personalized treatment.
Breyanzi, Abecma, and Other Approved Therapies
Other CAR-T cell therapies have also been approved, like Breyanzi and Abecma. Breyanzi treats certain DLBCL and follicular lymphoma. Abecma is for multiple myeloma. Each targets different antigens, giving patients more options.
Here’s a table showing the FDA-approved CAR-T cell therapies:
| Therapy Name | Target Antigen | Indications |
|---|---|---|
| Kymriah (Tisagenlecleucel) | CD19 | ALL, DLBCL |
| Yescarta (Axicabtagene Ciloleucel) | CD19 | DLBCL, certain non-Hodgkin lymphomas |
| Breyanzi (Lisocabtagene Maraleucel) | CD19 | DLBCL, follicular lymphoma |
| Abecma (Idecabtagene Vicleucel) | BCMA | Multiple Myeloma |
These CAR-T cell therapies are a big step forward in treating blood cancers. They offer new hope and better outcomes for patients. As research goes on, we’ll see even more advancements in CAR-T cell therapy.
Blood Cancers Successfully Treated with CAR-T Cells
CAR-T cell therapy is making a big difference in treating blood cancers. It’s changing how we treat leukemia, lymphoma, and multiple myeloma.
Leukemia: Types and Treatment Protocols
CAR-T cell therapy works well for some types of leukemia. Acute Lymphoblastic Leukemia (ALL) has seen great results, with some patients getting complete remission.
Lymphoma: Diffuse Large B-Cell and Beyond
For lymphoma, CAR-T cell therapy is approved for Diffuse Large B-Cell Lymphoma (DLBCL). It offers new hope for those who didn’t respond to other treatments.
Multiple Myeloma: Newest Applications
Multiple myeloma treatment is also seeing benefits from CAR-T cell therapy. Research is ongoing to improve its safety and effectiveness. New trials are showing promising results.
| Cancer Type | Specific Condition | Treatment Status |
|---|---|---|
| Leukemia | Acute Lymphoblastic Leukemia (ALL) | Approved |
| Lymphoma | Diffuse Large B-Cell Lymphoma (DLBCL) | Approved |
| Multiple Myeloma | Relapsed or Refractory Multiple Myeloma | Clinical Trials |
Remarkable Remission Rates in Clinical Trials
CAR-T cell therapy has changed how we treat some blood cancers. It has shown high remission rates in clinical trials. This gives hope to patients who have tried other treatments without success.
One key thing about CAR-T cell therapy is its high success rate. It works well for patients with hard-to-treat blood cancers. We’ll look into what these success rates mean for patients.
Understanding the 80%+ Response Rates
Research shows CAR-T cell therapy can work for over 80% of patients in some cases. For example, a key study found an 82% response rate in patients with a specific type of lymphoma. These patients had tried many treatments without success.
The treatment’s success comes from its personalized approach. It uses a patient’s own T-cells to attack cancer cells. This targeted method can lead to lasting and effective results.
“The advent of CAR-T cell therapy has marked a new era in the treatment of certain hematologic malignancies, giving patients a chance at long-term survival and potentially even cure.” – Hematologist-Oncologist
Long-term Survival Data in Refractory Cases
Long-term studies have shown CAR-T cell therapy’s lasting effects. Many patients have stayed in remission for a long time. This is a big deal for patients with poor prognoses.
For instance, a study on patients with relapsed or refractory ALL found many in complete remission at 24 months or more. This is a big win for a group with a tough prognosis.
The long-term survival data show CAR-T cell therapy’s promise. It could change how we treat certain blood cancers. It offers hope for patients who were once thought to have no cure.
The Patient Journey Through Car T Therapy
The journey through CAR-T cell therapy is complex. It involves several key steps. We will explore the patient’s journey, from the first evaluation to after treatment. We will focus on the main parts of this new cancer treatment.
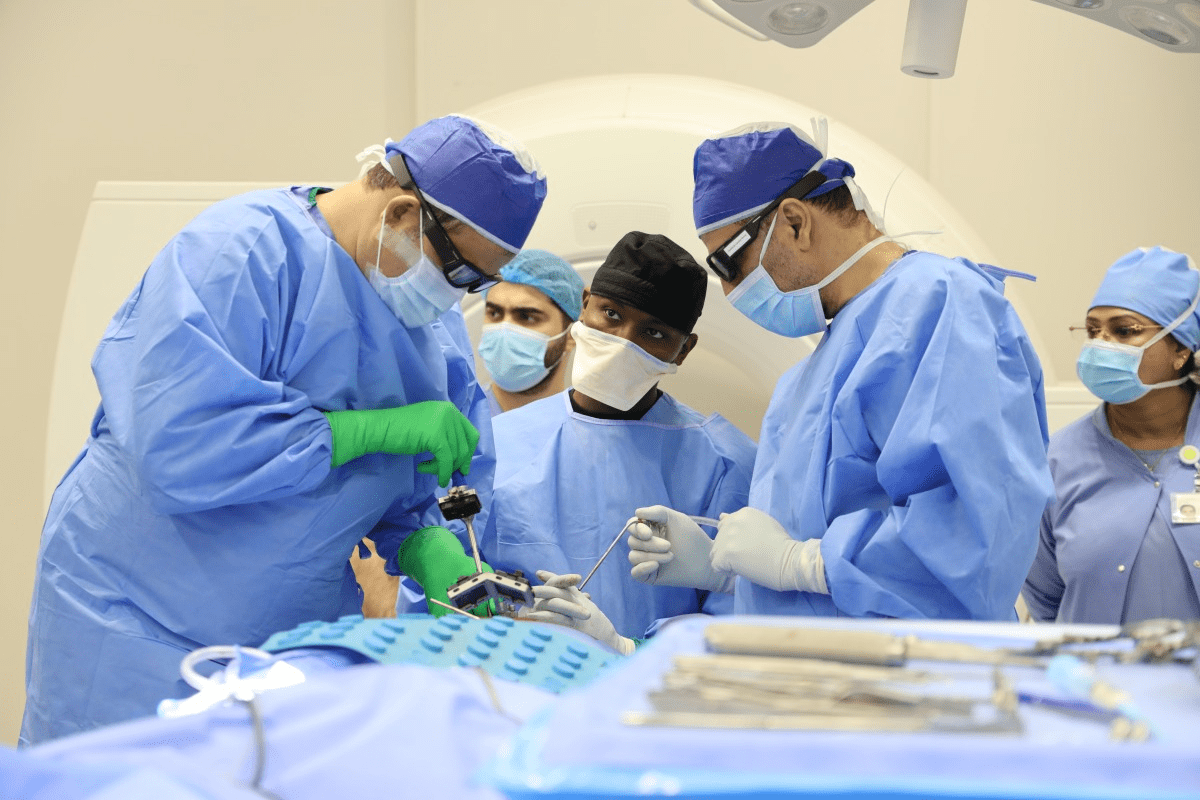
Pre-Treatment Evaluation and Eligibility
Before starting CAR-T cell therapy, a patient must be evaluated. This check looks at the patient’s health, past treatments, and cancer details. The evaluation includes:
- Comprehensive medical history
- Physical examination
- Laboratory tests (including blood counts and chemistry)
- Imaging studies (such as CT scans or PET scans)
The Cell Collection and Manufacturing Process
The cell collection process, or leukapheresis, takes T-cells from the patient’s blood. These cells are then sent to a lab to be made to fight cancer. The lab work includes:
| Step | Description | Timeline |
|---|---|---|
| T-cell extraction | Leukapheresis to collect T-cells | 1-2 days |
| Cell engineering | Genetic modification to target cancer cells | 7-14 days |
| Cell expansion | Growing the engineered cells | 7-14 days |
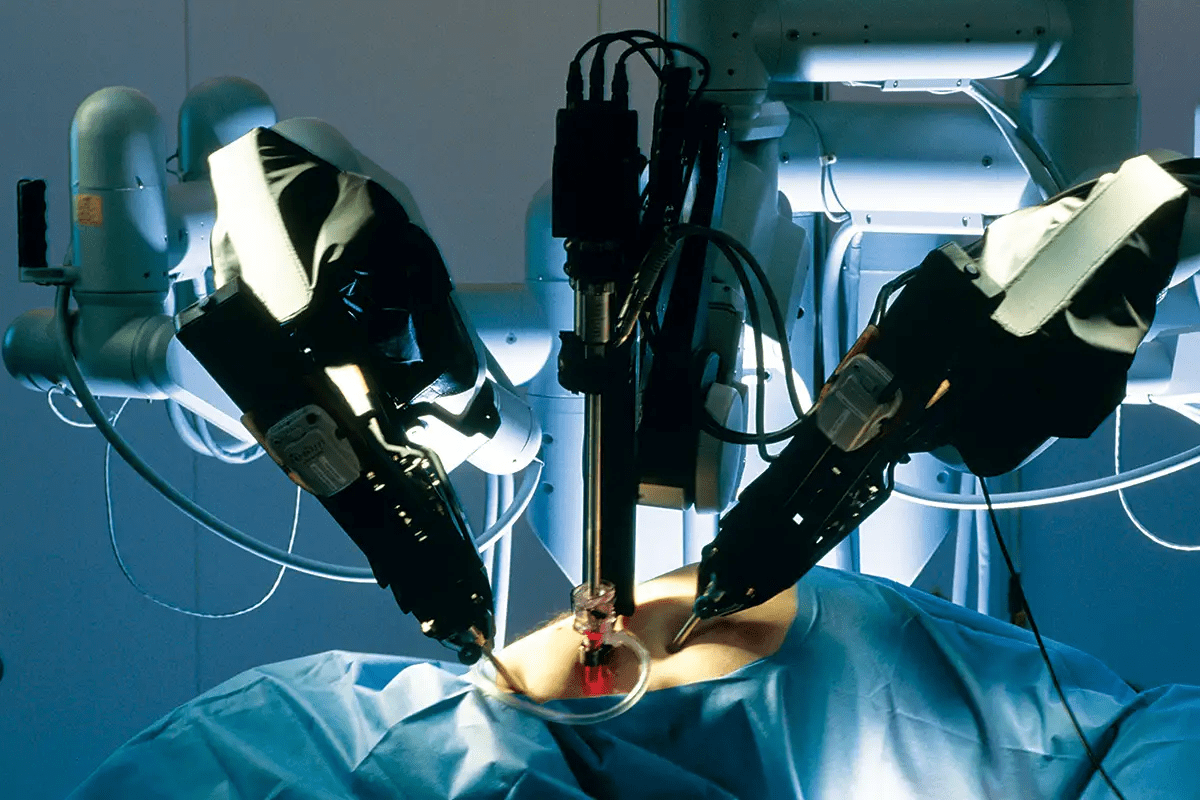
Infusion Procedure and Post-Treatment Monitoring
After the lab work, the CAR-T cells are given back to the patient. This is done through an IV, like a blood transfusion. It’s important to watch the patient closely after treatment for side effects and to see how well it worked.
Monitoring includes regular visits, lab tests, and imaging studies. These help check how the patient is doing and manage any side effects.
Managing Side Effects of CAR-T Cell Treatments
While CAR-T cell therapy offers new hope for cancer patients, it’s important to understand and manage its side effects. As we continue to use this innovative treatment, we must also address the challenges it presents.
Cytokine Release Syndrome: Recognition and Management
Cytokine release syndrome (CRS) is a major side effect of CAR-T cell therapy. It happens when the infused T cells release a lot of cytokines into the bloodstream. This can lead to serious complications. Early recognition and management of CRS are critical to prevent severe outcomes.
Symptoms of CRS can range from mild to severe. They include fever, fatigue, nausea, and in severe cases, hypotension and organ dysfunction. We use a grading system to assess CRS severity. For mild cases, we use hydration and antipyretics. But for severe cases, we use tocilizumab, an anti-IL-6 receptor antibody, to manage CRS.
Neurological Toxicities: ICANS and Other Complications
Neurological toxicity, or ICANS, is another significant side effect of CAR-T cell therapy. ICANS can cause confusion, disorientation, aphasia, and in severe cases, seizures or cerebral edema. The pathophysiology of ICANS is complex and not fully understood, making its management challenging.
We use a multidisciplinary approach to manage ICANS. This involves neurologists, intensivists, and other specialists as needed. Treatment strategies include supportive care, corticosteroids, and in some cases, anti-IL-6 therapy. Close monitoring and early intervention are key to mitigating ICANS risks.
Long-term Safety Considerations and Follow-up
Beyond immediate side effects, CAR-T cell therapy raises long-term safety concerns. Patients may face prolonged cytopenias, hypogammaglobulinemia, and long-term neurological effects. Ongoing monitoring and follow-up care are essential to manage these risks and ensure the best outcomes for patients.
We recommend regular follow-up visits to monitor blood counts, immunoglobulin levels, and overall health. Patients are also counseled on long-term risks and the importance of reporting new or concerning symptoms. By taking a proactive and holistic approach to long-term care, we can maximize CAR-T cell therapy benefits while minimizing risks.
Cost and Accessibility of CAR-T Cell Therapies
CAR-T cell therapies are changing cancer treatment, but cost and access are big concerns. These treatments are very expensive, costing between $373,000 and over $500,000 per session. The price depends on the product and what the patient needs.
Pricing Models and Insurance Coverage
The prices for CAR-T cell therapies vary a lot. For example, Kymriah costs about $373,000, and Yescarta is also around $373,000. Insurance coverage is key to making these treatments available to patients.
Key aspects of insurance coverage include:
- Most major insurance providers cover CAR-T cell therapies
- Coverage often depends on specific patient criteria and diagnosis
- Prior authorization is typically required
- Out-of-pocket costs can vary significantly for patients
Manufacturers are trying to make these treatments more accessible. They offer financial help and special pricing models.
Geographic Availability and Certified Treatment Centers
Not all places have access to CAR-T cell therapies. This is because they need special treatment centers. There are over 100 certified centers in the U.S. and more worldwide.
Key factors influencing geographic availability include:
- The need for specialized infrastructure and trained staff
- Complexity of the CAR-T cell manufacturing process
- Requirement for intensive patient monitoring and support
Healthcare systems are working to add more treatment centers. This will help more patients get these life-saving treatments.
As CAR-T cell therapies improve, we’ll see changes in pricing and insurance. More places will also offer these treatments. These changes will help more people get the help they need.
The Future Frontiers of Car T Research
CAR-T cell research is set to grow, reaching beyond current uses. Studies aim to solve current problems and find new ways to use this therapy.
Off-the-Shelf (Allogeneic) CAR-T Approaches
One exciting area is off-the-shelf, or allogeneic, CAR-T cells. These use donor cells, unlike today’s therapy that uses a patient’s cells. This could make treatment cheaper and more accessible.
But, there are challenges like graft-versus-host disease (GVHD). Gene editing, like CRISPR/Cas9, might help solve these issues.
| Feature | Autologous CAR-T | Allogeneic CAR-T |
|---|---|---|
| Cell Source | Patient’s own T cells | Donor-derived T cells |
| Production Time | Several weeks | Potentially faster, as cells are pre-made |
| Cost | High, due to personalized manufacturing | Potentially lower, with economies of scale |
| GVHD Risk | Low | Higher, but mitigated by gene editing |
Solid Tumor Applications: Challenges and Progress
CAR-T therapy works well for some blood cancers but faces hurdles in solid tumors. Researchers are tackling issues like tumor diversity and the immune-suppressing tumor environment.
Studies are looking for the right targets for solid tumors and ways to keep CAR-T cells active. Some ideas include using CAR-T with other treatments.
Autoimmune Disease Treatment
Researchers also see CAR-T therapy’s promise in treating autoimmune diseases. It could help reset the immune system, leading to long-term relief for conditions like lupus and rheumatoid arthritis.
Early trials show hope, with some patients seeing big improvements. But, more research is needed to fully grasp the benefits and risks.
As CAR-T cell research advances, we’ll see new uses for this technology. The future looks bright for treating various diseases with CAR-T therapy.
CAR-T Therapy Compared to Traditional Cancer Treatments
CAR-T cell therapy is a new way to fight cancer. It’s different from traditional chemotherapy. This method has shown great promise in treating blood cancers.
Advantages Over Conventional Chemotherapy
CAR-T cell therapy has big advantages over chemotherapy. It targets cancer cells directly, without harming healthy cells. Chemotherapy, on the other hand, can harm both cancer and healthy cells, causing more side effects.
Key benefits of CAR-T cell therapy include:
- Targeted action on cancer cells
- Potential for durable responses in patients with refractory or relapsed cancers
- A new treatment paradigm for patients who have failed multiple previous therapies
Complementary Roles with Stem Cell Transplantation
CAR-T cell therapy can also work with stem cell transplantation. These treatments fight cancer in different ways. Stem cell transplantation uses high-dose chemotherapy, replacing damaged stem cells. CAR-T cell therapy modifies T cells to attack cancer cells.
Using both therapies together might offer a better way to treat some cancers. For example, CAR-T cell therapy can kill remaining cancer cells after stem cell transplantation. This could lead to better results for patients.
It’s worth noting that the specific application of CAR-T cell therapy in relation to stem cell transplantation is an area of ongoing research, with clinical trials exploring the safety and efficacy of various combinations.
Global Impact: Over 30,000 Patients Treated Worldwide
The global use of CAR-T cell therapy has been groundbreaking. Over 30,000 patients worldwide have been treated. This treatment has changed cancer care and given hope to many.
As we learn more about CAR-T cell therapy, its global effect is key. Its use in many countries shows its power to change cancer treatment worldwide.
International Adoption and Availability
CAR-T cell therapy has quickly been adopted globally. Countries worldwide have started using it, with many centers of excellence opening. This has made the treatment more available to more people.
Even countries with less resources are starting to use CAR-T cell therapy. They see its value in improving cancer care for their people. This shows the medical community’s teamwork in fighting cancer.
Patient Demographics and Selection Criteria
Patients getting CAR-T cell therapy come from all walks of life. They are young and old, with different blood cancers. The treatment is mainly for those with certain types of blood cancers.
As we get more experience with CAR-T cell therapy, patient selection is getting better. New data helps decide who will benefit most. Age, health, and disease details are all considered.
Conclusion: The Transformative Promise of CAR-T Cell Therapy
We’ve looked into CAR-T cell therapy, its history, and how it’s used to fight blood cancers. This therapy has changed how we treat cancer, giving hope to those with leukemia, lymphoma, and multiple myeloma.
What makes CAR-T cell therapy special is its personalized and targeted approach. It turns a patient’s T-cells into cancer-fighting machines. This has led to high success rates in trials. It’s a major step forward in cancer treatment.
So far, over 30,000 patients worldwide have been treated with CAR-T cell therapy. It shows great promise in improving patient outcomes. As research grows, we’ll see even more improvements, like treatments for solid tumors. We’re excited to share these advancements in the fight against cancer.
What is CAR T therapy?
CAR T therapy uses your own T cells to fight cancer. It takes T cells, changes them to find cancer, and puts them back in you.
How does CAR T cell therapy work?
It adds a special receptor to T cells. This lets them find and kill cancer cells better.
What blood cancers can be treated with CAR-T cell therapy?
It’s approved for leukemia, lymphoma, and multiple myeloma. It can lead to complete remission for some patients.
What are the FDA-approved CAR-T cell therapies?
The FDA has approved Kymriah, Yescarta, Breyanzi, and Abecma. Each targets different cancer types.
What is the process of CAR T cell therapy?
It starts with taking T cells, then changing them, and putting them back in you. Before and after, you’re closely watched.
What are the side effects of CAR-T cell therapy?
It can cause serious side effects like cytokine release syndrome and brain problems. Managing these is key.
How much does CAR-T cell therapy cost?
It’s very expensive, costing hundreds of thousands to over a million dollars. Insurance and where you live can affect if you can get it.
What is the future of CAR-T cell therapy?
Researchers are working to make it better and use it for more things. They’re looking at solid tumors and autoimmune diseases.
How does CAR-T cell therapy compare to traditional cancer treatments?
It’s more targeted and personal than chemotherapy. It can work with other treatments, like stem cell transplants.
Is CAR-T cell therapy available globally?
Yes, it’s used worldwide, helping thousands of patients. But, where and who can get it varies.
What is the response rate of CAR-T cell therapy in clinical trials?
Trials show it’s very effective, with over 80% of patients responding. Long-term, it looks promising for hard-to-treat cancers.
Can CAR-T cell therapy be used for solid tumors?
It’s mainly for blood cancers, but research is exploring solid tumors. It’s a tough challenge, but progress is being made.