Listing and explaining conditions similar to asthma and copd that often lead to misdiagnosis (e.g., heart failure, bronchiectasis). Asthma is often misdiagnosed, with studies showing about 30% of those thought to have it actually don’t. This is because other conditions can cause similar breathing problems.
Many health issues can make it hard to breathe, like heart failure. Doctors use special tests to figure out why someone is having trouble breathing.
At Liv Hospital, we focus on accurate diagnoses to give the right treatment. It’s key to know the conditions that mimic asthma to care for patients properly.
Key Takeaways
- Asthma is often misdiagnosed, with approximately 30% of patients having another condition.
- Breathing difficulties can be caused by various health issues, including heart failure.
- Accurate diagnosis is key for the right treatment.
- Thorough testing is needed to find the real cause of breathing problems.
- Understanding asthma-like conditions is vital for good care.
The Challenge of Asthma Diagnosis
Asthma is often misdiagnosed because its symptoms can look like other health issues. This makes it hard for doctors to accurately diagnose asthma.
Misdiagnosis Statistics
About 30% of people thought to have asthma might actually have something else. This mistake can lead to wrong treatments and delayed care for the real problem.
The effects of wrong diagnosis are big. Patients might get the wrong meds or miss the right treatment. This shows how important it is to get the diagnosis right.
Why Asthma Is Frequently Misdiagnosed
Asthma symptoms can look like other health problems, like GERD, vocal cord issues, and heart disease. This makes it hard to tell what’s really going on.
- GERD can cause coughing and wheezing, like asthma.
- Vocal cord problems can make breathing hard, like asthma.
- Heart issues can also cause shortness of breath, like asthma.
Common Symptoms That Lead to Confusion
Symptoms like wheezing, coughing, and shortness of breath are common in asthma. But they can also be signs of other health issues. It’s important to understand these symptoms and their possible causes.
- Wheezing can mean asthma, but it can also show up in other lung problems.
- Coughing is a symptom that can point to asthma or other lung issues.
- Shortness of breath needs careful checking to figure out why it’s happening.
Gastroesophageal Reflux Disease (GERD)

GERD is a chronic digestive disorder that can cause symptoms similar to asthma. This can lead to misdiagnosis. We will look at how GERD can be mistaken for asthma and the differences between the two.
How GERD Mimics Asthma Symptoms
GERD causes stomach acid to flow back into the esophagus. Sometimes, this acid reaches the lungs, causing respiratory symptoms. These symptoms include coughing, wheezing, and shortness of breath, common in asthma.
The irritation of the airways by stomach acid leads to inflammation and constriction. This can cause a range of respiratory issues that mimic asthma. If the cause is not properly investigated, it can lead to a misdiagnosis.
Distinguishing Features of GERD
While GERD and asthma share similar symptoms, there are key differences. These include:
- Heartburn and regurgitation, classic GERD symptoms.
- Difficulty swallowing or feeling like food is stuck in the throat.
- Chest pain that may spread to the back, arms, or jaw.
These symptoms are less common in asthma. They can indicate the presence of GERD.
When to Suspect GERD Instead of Asthma
Healthcare providers should suspect GERD when patients show typical GERD symptoms. They should also consider it when asthma symptoms don’t respond to standard treatments. Tests like endoscopy or esophageal pH monitoring can confirm GERD.
|
Symptom |
GERD |
Asthma |
|---|---|---|
|
Coughing |
Often triggered by lying down or eating |
Typically worse at night or with exposure to allergens |
|
Wheezing |
May occur due to acid reflux into the airways |
Common due to airway constriction |
|
Chest Pain |
Can be a burning sensation or sharp pain |
Usually associated with tightness or discomfort |
Understanding the differences between GERD and asthma is key for accurate diagnosis and treatment. Recognizing the unique characteristics of each condition helps healthcare providers offer targeted care to patients.
Vocal Cord Dysfunction (VCD)
Vocal Cord Dysfunction (VCD) can be mistaken for asthma because of similar symptoms. It involves the abnormal closure of the vocal cords during breathing. This can cause respiratory distress.
Symptoms That Overlap With Asthma
VCD and asthma share symptoms, making it important to tell them apart. Symptoms of VCD include wheezing, shortness of breath, and throat tightness. These symptoms are similar to asthma, leading to misdiagnosis.
Wheezing is a key symptom in both conditions. But in VCD, wheezing happens during both inhalation and exhalation. In asthma, it mainly occurs when breathing out.
Key Differences Between VCD and Asthma
While both can cause wheezing and shortness of breath, there are differences. VCD often causes hoarseness and a feeling of strangulation or tightness in the throat. This is less common in asthma.
Asthma is often triggered by allergens, cold air, or exercise. VCD, on the other hand, can be triggered by stress, anxiety, or irritants.
|
Characteristics |
VCD |
Asthma |
|---|---|---|
|
Wheezing |
Inspiratory or biphasic |
Expiratory |
|
Triggers |
Stress, anxiety, irritants |
Allergens, cold air, exercise |
|
Symptoms |
Hoarseness, throat tightness |
Cough, chest tightness |
Diagnostic Approaches for VCD
Diagnosing VCD requires a clinical evaluation and diagnostic tests. Laryngoscopy is a key tool that lets doctors see the vocal cords during breathing.
Other tests include spirometry, which shows airflow changes during VCD episodes. Provocation testing also helps find triggers.
“The diagnosis of VCD requires a high index of suspicion and careful evaluation to distinguish it from asthma and other respiratory conditions.” – Expert in Pulmonology
Understanding VCD and its differences from asthma is key for proper treatment. Accurate diagnosis of VCD allows for targeted therapies. This helps alleviate symptoms and improves quality of life.
Anxiety-Related Breathing Disorders
Anxiety can make breathing hard, making it hard to tell if it’s asthma. Anxiety can cause breathing problems that look like asthma. We’ll look at how anxiety can make symptoms seem like asthma and why it’s important to tell them apart.
Panic Attacks vs. Asthma Attacks
Panic attacks can make breathing feel very hard, like asthma. But, there are big differences. Panic attacks come with a lot of fear or worry, while asthma attacks have a history and specific things that set them off.
Key differences between panic attacks and asthma attacks:
|
Characteristics |
Panic Attacks |
Asthma Attacks |
|---|---|---|
|
Primary Symptoms |
Intense fear, palpitations, hyperventilation |
Wheezing, coughing, shortness of breath |
|
Triggers |
Stress, anxiety-provoking situations |
Allergens, respiratory infections, exercise |
|
Response to Treatment |
Responds to anxiety management techniques |
Responds to asthma medications |
Hyperventilation Syndrome
Hyperventilation syndrome is when you breathe too fast and deep, often because of stress or anxiety. This can make you feel dizzy, lightheaded, and your fingers might tingle, making it seem like asthma. It’s important to know why you’re hyperventilating to treat it right.
Hyperventilation syndrome can be managed through breathing exercises and relaxation techniques.
The Anxiety-Asthma Connection
Anxiety and asthma are closely linked. Anxiety can make asthma worse, and having asthma can make you more anxious. It’s key to treat both at the same time for the best results.
When we diagnose and treat patients, we must think about how anxiety and asthma work together. Understanding both conditions helps us give better care and treatment plans.
Cardiac Conditions That Mimic Asthma
Heart problems, like heart failure, can show symptoms that look like asthma. This makes it hard to figure out what’s wrong. It’s important to know about these heart issues to give the right diagnosis and treatment.
Heart Failure and Cardiac Asthma
Heart failure means the heart can’t pump enough blood. This can cause symptoms like shortness of breath and wheezing. Cardiac asthma is when heart failure makes symptoms look like asthma.
It’s key to tell cardiac asthma apart from real asthma. Asthma is a long-term inflammation of the airways. But cardiac asthma is a sign of heart failure. The treatments for these are very different.
Coronary Artery Disease
Coronary artery disease (CAD) can also look like asthma. CAD happens when the heart’s main blood vessels get damaged. Symptoms like chest tightness and hard breathing might be mistaken for asthma.
Distinguishing Cardiac from Pulmonary Symptoms
Telling apart heart and lung problems is important for good care. Here’s a table that shows the main differences:
|
Symptom |
Cardiac Cause |
Pulmonary Cause (Asthma) |
|---|---|---|
|
Shortness of Breath |
Often linked to effort or lying down |
Can happen anytime, often from allergens or irritants |
|
Wheezing |
May be present, mainly in cardiac asthma |
Common, often with cough and chest tightness |
|
Chest Pain/Tightness |
Common in coronary artery disease, may spread to arm or jaw |
Typically due to airway narrowing |
It’s vital for doctors to know the difference between heart problems and asthma. By looking closely at symptoms and using tests, we can make sure patients get the right treatment.
Conditions Similar to Asthma and COPD: Pulmonary Disorders
Many pulmonary conditions can look like asthma and COPD, making diagnosis hard. We’ll look at some of these conditions, their symptoms, and why getting the right diagnosis is key.
Pulmonary Hypertension
Pulmonary hypertension means high blood pressure in the lungs’ arteries. It can cause shortness of breath, fatigue, and chest pain, similar to asthma or COPD. Accurate diagnosis is vital because treatments are different.
Bronchiectasis
Bronchiectasis makes airways wider and can cause chronic cough, sputum, and infections. It shares some symptoms with COPD but needs its own treatment plan.
Alpha-1 Antitrypsin Deficiency
Alpha-1 antitrypsin deficiency is a genetic disorder that can lead to lung disease, like emphysema. It’s often linked to COPD but has its own treatment and can affect the liver too.
Interstitial Lung Disease
Interstitial lung disease (ILD) includes lung disorders with inflammation and scarring. It can cause shortness of breath and cough, like asthma and COPD. But, ILD needs specific tests and treatments.
It’s important for doctors to know about these conditions to make the right diagnosis and treatment plans. By understanding each condition’s unique features, we can help patients live better lives.
Upper Airway and Structural Issues
It’s not always asthma; sometimes, upper airway structural issues are the culprit behind respiratory distress. When diagnosing respiratory conditions, it’s key to look at the upper airway and structural abnormalities. These can mimic asthma symptoms.
Tracheobronchomalacia
Tracheobronchomalacia is a condition where the cartilage in the trachea and bronchi weakens or softens. This can cause the airway to partially or fully collapse during breathing. Symptoms include wheezing, coughing, and shortness of breath, similar to asthma.
Key features of tracheobronchomalacia include:
- Dynamic airway collapse during expiration
- Worsening symptoms during respiratory infections or with increased intrathoracic pressure
- Possible presence of a “dying breath” or “fish mouth” appearance on bronchoscopy
Central Airway Obstruction
Central airway obstruction is when the trachea or main bronchi are partially or fully blocked. This can be due to tumors, foreign bodies, or inflammation. Symptoms include stridor, wheezing, and dyspnea, which can be mistaken for asthma.
Diagnostic approaches for central airway obstruction include:
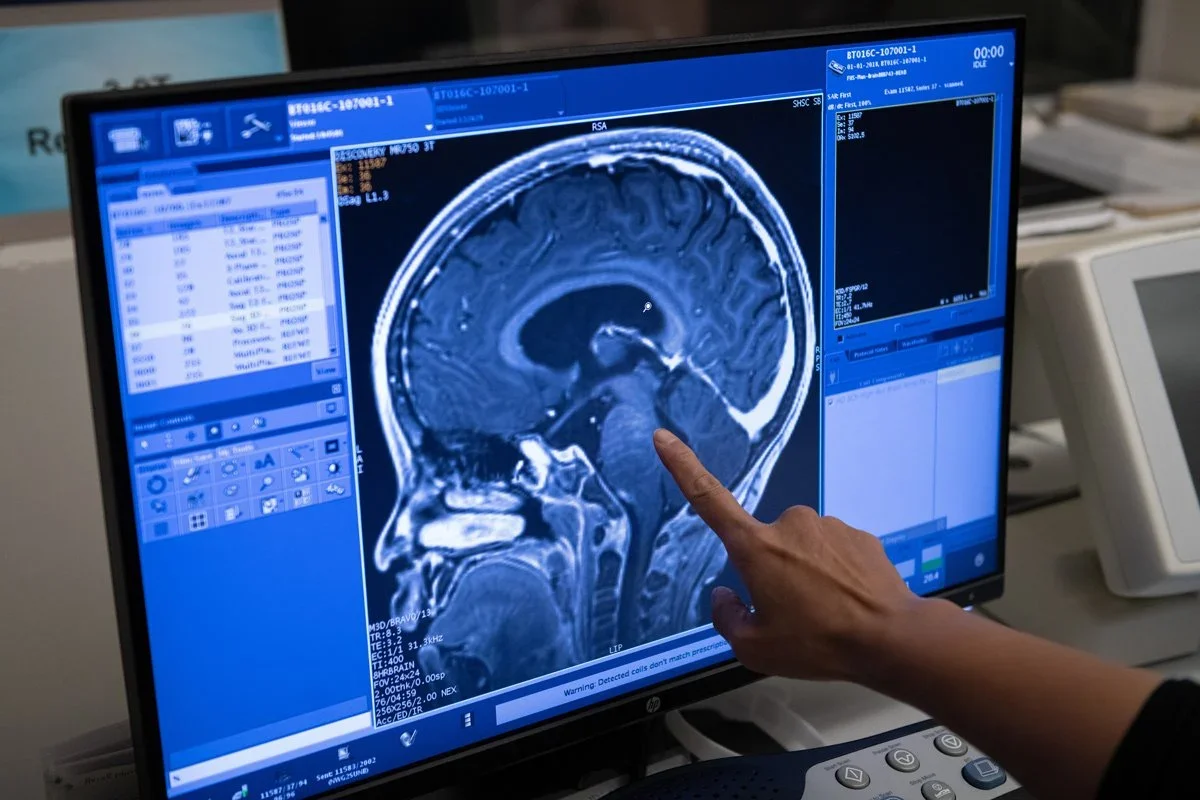
- Imaging studies such as CT scans or MRI
- Bronchoscopy to visualize the airway and assess the extent of obstruction
- Flow-volume loops to evaluate the functional impact of the obstruction
Laryngeal and Tracheal Abnormalities
Laryngeal and tracheal abnormalities can also present with symptoms similar to asthma. Conditions like laryngomalacia, tracheal stenosis, or laryngeal cysts can cause wheezing, coughing, or difficulty breathing.
Diagnostic considerations for laryngeal and tracheal abnormalities include:
- Laryngoscopy or bronchoscopy to visualize the larynx and trachea
- Imaging studies to assess the structure of the upper airway
- Evaluation of symptoms during different phases of breathing
Accurate diagnosis of these upper airway and structural issues is key for proper management and treatment. We must consider these conditions when evaluating patients with respiratory symptoms that may be attributed to asthma.
Allergic and Inflammatory Conditions
Allergic and inflammatory conditions can be hard to tell apart from asthma. They cause breathing problems and need different treatments than asthma.
Allergic Bronchopulmonary Aspergillosis
Allergic bronchopulmonary aspergillosis (ABPA) is a reaction to Aspergillus. It often hits people with asthma or cystic fibrosis. Symptoms include wheezing, coughing, and trouble breathing, making it seem like asthma is getting worse.
Diagnostic Features of ABPA:
- Presence of Aspergillus-specific IgE antibodies
- Eosinophilia
- Central bronchiectasis
- High total IgE levels
Eosinophilic Bronchitis
Eosinophilic bronchitis has chronic cough and sputum eosinophilia but no asthma. It’s a unique condition that can be mistaken for asthma because of similar symptoms.
|
Characteristics |
Asthma |
Eosinophilic Bronchitis |
|---|---|---|
|
Primary Symptom |
Wheezing and shortness of breath |
Chronic cough |
|
Eosinophilia |
Present |
Present |
|
Airway Obstruction |
Reversible |
Not reversible |
Hypersensitivity Pneumonitis
Hypersensitivity pneumonitis (HP) is a lung disease caused by inhaling certain antigens. It can be linked to work or environmental exposures. Symptoms include cough, shortness of breath, and tiredness, which might be mistaken for asthma or other lung issues.
Diagnostic Approaches for HP:
- Detailed exposure history
- High-resolution CT scans
- Serum precipitins against suspected antigens
- Lung biopsy in some cases
Getting the right diagnosis for these conditions is key to proper treatment. Knowing the unique signs of each helps doctors treat them differently from asthma.
Conclusion: The Importance of Accurate Diagnosis
Getting a correct diagnosis is key to managing breathing problems well. We’ve talked about how some conditions can be mistaken for asthma. This shows how tricky it can be to figure out what’s really going on.
Asthma misdiagnosis can lead to the wrong treatment and too much medication. This is why a detailed medical history, physical check-up, and tests are so important.
When we see patients with symptoms that seem like asthma, we need to think about many other conditions. This is called differential diagnosis. It helps us find the real cause of symptoms. This way, we can give better treatment plans.
By understanding all the conditions that can look like asthma, we can make better diagnoses. We should always be ready to think of other possibilities if treatment doesn’t work. This way, we can give patients the best care for their specific needs.
FAQ
What are some conditions that can be mistaken for asthma?
Conditions like Gastroesophageal Reflux Disease (GERD) and Vocal Cord Dysfunction (VCD) can be mistaken for asthma. Anxiety-related breathing disorders, heart issues, and lung problems can also be confused with asthma.
How can GERD be distinguished from asthma?
GERD can be told apart from asthma by its symptoms, like heartburn and regurgitation. Tests like endoscopy and pH monitoring help diagnose GERD. GERD can irritate the airways, causing asthma-like symptoms.
What is Vocal Cord Dysfunction (VCD) and how is it different from asthma?
VCD is when the vocal cords don’t work right, causing symptoms like wheezing and shortness of breath. It’s different from asthma and can be diagnosed with tests like laryngoscopy and specific breathing tests.
Can anxiety cause symptoms similar to asthma?
Yes, anxiety can make you breathe too fast and cause panic attacks. These symptoms can be like asthma. It’s important to think about anxiety when diagnosing asthma.
How can cardiac conditions be distinguished from asthma?
Heart problems like heart failure and coronary artery disease can feel like asthma. A doctor will look at your medical history and do tests like echocardiography to tell the difference.
What are some pulmonary disorders that can be confused with asthma or COPD?
Pulmonary issues like pulmonary hypertension and bronchiectasis can seem like asthma or COPD. To diagnose correctly, a doctor will do imaging studies and pulmonary function tests.
Can structural issues in the upper airway be mistaken for asthma?
Yes, problems like tracheobronchomalacia can seem like asthma. Tests like bronchoscopy can help find these issues.
What are some allergic and inflammatory conditions that can be mistaken for asthma?
Allergic conditions like allergic bronchopulmonary aspergillosis can seem like asthma. A doctor will need to do allergy tests and possibly a lung biopsy to diagnose correctly.
Is it possible to have asthma-like symptoms without having asthma?
Yes, many conditions can cause symptoms that seem like asthma. This shows why getting the right diagnosis is so important.
Why is accurate diagnosis important in managing respiratory conditions?
Getting the right diagnosis is key to treating respiratory conditions. It ensures patients get the right treatment, improving their health and life quality.
Can you have an asthma attack without having asthma?
Yes, you can have symptoms that seem like an asthma attack without having asthma. This can happen if you have another condition that mimics asthma.
How do you know if you have asthma or another condition?
To figure out if you have asthma or something else, you need a full evaluation. This includes looking at your medical history, doing a physical exam, and running tests like pulmonary function tests and imaging studies.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://pubmed.ncbi.nlm.nih.gov/28027384/