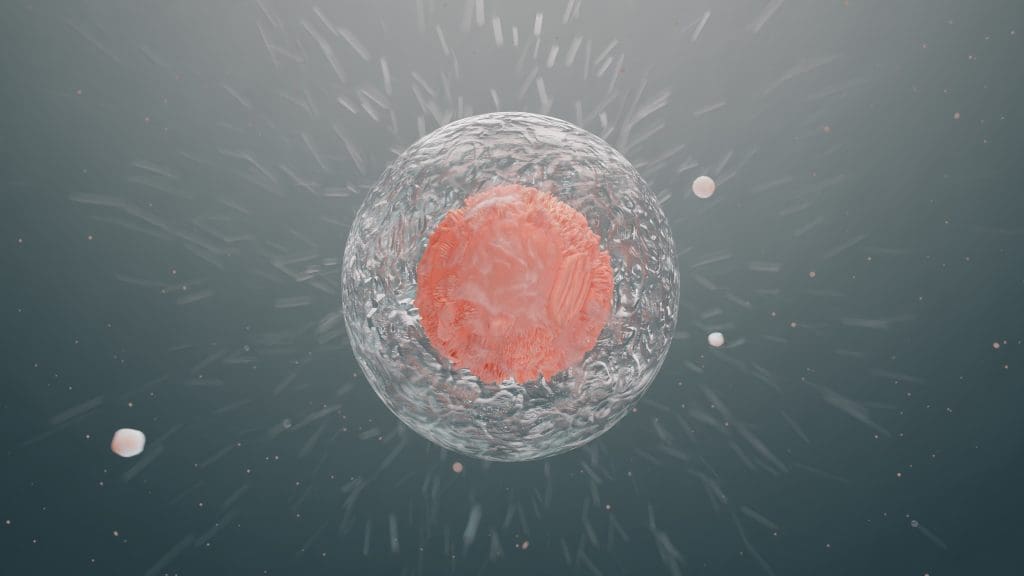
Did you know that pluripotent stem cells can turn into almost any cell in the human body? This makes them very important for medical research and new treatments.
These cells are also called embryonic stem cells. They have a lot of promise for learning about human growth and treating diseases. Their ability to become different cell types is a big step forward for regenerative medicine.
Key Takeaways
- Pluripotent stem cells can develop into almost any cell type.
- They are very important for medical research and new treatments.
- These cells are also known as embryonic stem cells.
- Their ability to change into different cells is very useful for regenerative medicine.
- Learning about pluripotent stem cells can lead to new treatments.
The Fundamental Nature of Embryonic Stem Cells
Embryonic stem cells come from early-stage embryos. They can turn into almost any cell in the body. This makes them very useful for studying human development, diseases, and for regenerative medicine.
Defining Embryonic Stem Cells and Their Origin
Embryonic stem cells are pluripotent stem cells from the inner cell mass of a blastocyst, an early embryo. They can become almost any cell type. This is key for their role in development and in medical treatments.
To get embryonic stem cells, embryos from in vitro fertilization are used. The inner cell mass is taken out. Then, these cells are grown in the lab to keep their ability to become many cell types.
Key Characteristics That Make Them Unique
One main trait of embryonic stem cells is their pluripotency. This means they can become every type of body cell. This is different from multipotent stem cells, which can only become a few types of cells.
| Characteristic | Description |
| Pluripotency | Ability to differentiate into almost any cell type |
| Self-renewal | Capacity to proliferate without differentiating |
| Origin | Derived from the inner cell mass of a blastocyst |
These traits make embryonic stem cells a strong tool in biomedical research. They also hold promise for cell therapies in regenerative medicine.
Pluripotent Stem Cells: The Scientific Terminology
Pluripotency is key to understanding embryonic stem cells. These cells can turn into any type of body cell.
What “Pluripotent” Means in Cell Biology
In cell biology, “pluripotent” means a stem cell can become almost any cell type. This means they can turn into nerve, muscle, or blood cells.
Pluripotency is a critical characteristic that makes embryonic stem cells special.A stem cell expert says, “Pluripotency is what makes embryonic stem cells so valuable for research and possible treatments.”
Why Embryonic Stem Cells Are Classified as Pluripotent
Embryonic stem cells are called pluripotent because they come from early embryos. They can turn into many cell types. This is because of their origin and ability to form different cells in a lab.
Their pluripotency comes from their special gene expression. This lets them stay undifferentiated but also turn into various cell types.
Understanding pluripotency is vital for stem cell research and new treatments. The study of pluripotent stem cells is ongoing. It has big implications for regenerative medicine and understanding human development.
Different Classes of Stem Cells Explained
It’s important to know about the different types of stem cells. They play a big role in how our bodies grow and heal. Stem cells are sorted by how many kinds of cells they can turn into.
Totipotent Stem Cells: The Most Versatile
Totipotent stem cells are the most flexible. They can become any cell in the body, including those in the placenta. This makes them key in the start of a baby’s development.
Pluripotent Stem Cells: Extensive but Limited
Pluripotent stem cells can turn into almost any cell, except those in the placenta. They live in the early embryo and are vital for research and healing.
Multipotent and Unipotent Stem Cells: More Restricted
Multipotent stem cells can turn into a few types of cells. For example, blood cells. Unipotent stem cells can only turn into one type of cell.
Knowing about totipotent, pluripotent, multipotent, and unipotent stem cells is key. It helps scientists improve treatments and healing.
- Totipotent: Can develop into any cell type, including placental cells.
- Pluripotent: Can differentiate into almost any cell type, excluding placental cells.
- Multipotent: Can develop into multiple cell types within a specific lineage.
- Unipotent: Can differentiate into only one cell type.
The Historical Development of Stem Cell Research
Stem cell research has a rich history that shows how far we’ve come. It’s filled with key discoveries and big steps forward. These have changed how we see stem cells and their uses.
Early Discoveries and Pioneering Work
In the early 20th century, scientists started working with stem cells. But it wasn’t until the 1960s that big breakthroughs happened.
The 1980s brought a major milestone with the discovery of embryonic stem cells. Martin Evans and Matthew Kaufman found these cells in mouse embryos. They could turn into many different cell types. This opened up new paths for studying development and regenerative medicine.
Evolution of Terminology and Understanding
As research went on, so did our understanding of stem cells. The term “pluripotent” became common for cells that can become many types. Then, in 2006, Shinya Yamanaka found a way to make adult cells pluripotent. This was a game-changer, making personalized medicine seem closer.
Stem cell research has also seen tech and culture techniques get better. These improvements help keep and change stem cells in labs. They’re key for the growth of regenerative medicine and cell therapy.
Sources of Embryonic Stem Cells
Embryonic stem cells come from the inner cell mass of blastocysts. These are embryos that have grown for about 5-6 days. They are pluripotent, which means they can turn into almost any cell in the body.
Blastocysts and the Inner Cell Mass
The journey to get embryonic stem cells starts with the blastocyst. This is an early stage in development with a fluid-filled cavity and an inner cell mass. The inner cell mass is key because it forms the fetus. The outer layer, or trophoblast, helps make placental tissues.
Cells from the inner cell mass are taken out and grown in labs. This involves breaking down the inner cell mass into single cells. Then, these cells are grown on a special layer to help them grow and stay pluripotent.
Donation and Collection Processes
Getting embryonic stem cells often uses embryos left over from in vitro fertilization (IVF). Couples or individuals who have done IVF might donate these embryos for research. This is a great way to get these cells.
The donation process makes sure donors know how their embryos will be used. This is very important in stem cell research. It shows respect for the donors’ choices and privacy.
After donation, the embryos are grown in labs until they are blastocysts. Then, the inner cell mass is taken out to get the stem cells.
Induced Pluripotent Stem Cells (iPSCs): A Revolutionary Alternative
A major breakthrough in stem cell technology came with the development of induced pluripotent stem cells. This innovation has opened new avenues in regenerative medicine and cellular therapy.
The Breakthrough of Cellular Reprogramming
Cellular reprogramming is a process that allows scientists to convert adult cells into a pluripotent state, similar to that of embryonic stem cells. This is achieved by introducing specific genes that reprogram the cell’s genetic material.
Key to this technology is the ability to reprogram adult cells, such as skin or blood cells, into iPSCs. These cells can then be directed to differentiate into various cell types, opening up new treatments for many diseases.
“The discovery of induced pluripotent stem cells has revolutionized the field of stem cell research, providing a powerful tool for understanding development and disease.”
How iPSCs Differ from Embryonic Stem Cells
While both iPSCs and embryonic stem cells are pluripotent, they differ in their origin. Embryonic stem cells are derived from embryos, whereas iPSCs are generated from adult cells through reprogramming.
iPSCs offer several advantages, including avoiding the ethical concerns associated with embryonic stem cells. They can also be made from a patient’s own cells, potentially reducing the risk of immune rejection.
Advantages and Limitations of iPSC Technology
iPSC technology has several advantages, including the promise of personalized medicine and the ability to model diseases in vitro. Yet, there are also limitations, such as the risk of insertional mutagenesis and the possibility of teratoma formation.
- Advantages:
- Potential for personalized cell therapy
- Ability to model diseases
- Avoidance of ethical concerns related to embryonic stem cells
- Limitations:
- Risk of insertional mutagenesis
- Potential for teratoma formation
- Efficiency and stability of reprogramming
In conclusion, induced pluripotent stem cells represent a significant advancement in stem cell biology, opening new possibilities for research and therapy. While challenges remain, the promise of iPSCs to transform our understanding and treatment of diseases is substantial.
Cultivation and Maintenance of Pluripotent Stem Cells
To grow pluripotent stem cells, we need a special environment. This keeps their ability to become many different cell types. We use certain lab techniques to support these cells.
Laboratory Techniques for Stem Cell Culture
There are several important lab techniques for growing pluripotent stem cells. These include:
- Maintaining cells in a feeder-free or feeder-dependent culture system.
- Using growth factors such as basic fibroblast growth factor (bFGF) to support pluripotency.
- Passaging cells regularly to prevent overgrowth and maintain their undifferentiated state.
- Monitoring cell health and detecting any signs of differentiation or contamination.
Feeder-free cultures help avoid contamination and ensure consistent conditions. But, they need careful control over growth factors and nutrients.
Challenges in Maintaining Pluripotency
Keeping pluripotent stem cells in their undifferentiated state is a big challenge. This requires:
- Optimizing the culture conditions to support pluripotency.
- Avoiding the introduction of differentiation-inducing factors.
- Regularly monitoring the cells for signs of differentiation.
Genetic instability is another issue, as long culture can cause chromosomal problems. Regular genetic tests are key to keeping the cells healthy.
By tackling these challenges, researchers can better grow and keep pluripotent stem cells. This boosts their use in medicine.
Differentiation Process: What Makes Pluripotent Stem Cells Special
Understanding pluripotent stem cells is key for regenerative medicine. These cells can turn into any cell type in the body. This makes them very useful for research and treatments.
The Process of Cellular Differentiation
Cellular differentiation is when a cell becomes specialized. It’s guided by genes and the environment. Transcription factors are important in deciding a cell’s path.
The steps to become a specific cell include gene changes and shape changes. Signaling pathways help control these steps, responding to inside and outside signals.
Controlling Differentiation in Laboratory Settings
In labs, controlling stem cell differentiation is vital. Researchers use culture conditions and growth factors to guide it.
Getting consistent results is a big challenge. It requires an understanding of biology and the control of multiple factors.
| Differentiation Factor | Role in Differentiation | Example |
| Growth Factors | Regulate cell growth and differentiation | FGF, BMP |
| Signaling Pathways | Control gene expression and cell fate | Wnt/β-catenin, Notch |
| Culture Conditions | Influence cell environment and differentiation | Serum-free media, feeder layers |
By managing these factors, researchers can guide stem cells to specific types. This is promising for regenerative medicine and cell therapy.
Applications in Regenerative Medicine and Cell Therapy
Pluripotent stem cells are changing healthcare. They can turn into many cell types. This helps in making new treatments for diseases and injuries.
Current Therapeutic Applications
These cells are being studied for treating many conditions. Current therapeutic applications include fixing heart damage, helping with macular degeneration, and possibly treating brain disorders.
- Cardiovascular repair: Using stem cells to regenerate heart tissue after a heart attack.
- Ophthalmological treatments: Restoring vision by replacing damaged retinal cells.
- Neurological disorders: Exploring the use of stem cells for Parkinson’s disease.
Disease-Specific Applications
Pluripotent stem cells can be used for disease-specific applications. They can turn into specific cells needed for treatment. For example, in diabetes, they can make insulin-producing cells.
Tissue Engineering Using Pluripotent Stem Cells
Tissue engineering is another area where stem cells are making a big difference. By mixing these cells with materials, scientists are making functional tissue substitutes. These can replace or fix damaged tissues.
- Creating artificial organs: Using stem cells to develop functional organs for transplantation.
- Repairing damaged tissues: Applying stem cells to regenerate tissues lost due to injury or disease.
- Developing tissue models: Creating in vitro models of tissues for drug testing and disease modeling.
In conclusion, pluripotent stem cells have many uses in regenerative medicine and cell therapy. They offer hope for treating many diseases and injuries.
Common Misconceptions About Pluripotent Stem Cells
The world of pluripotent stem cells is full of misconceptions. These misconceptions are both scientific and ethical. There’s a big gap between what people think and what’s really true about them.
Scientific Misunderstandings
Many people think pluripotent stem cells can turn into any cell type. But, they can’t become just any cell. They have a wide range of possibilities, but there are limits.
- Pluripotent stem cells can become every type of body cell.
- They can’t become a complete organism by themselves.
- Turning these cells into specific types is very complex and is being studied.
Another big mistake is thinking pluripotent stem cells and induced pluripotent stem cells (iPSCs) are the same. They are both pluripotent, but they come from different sources. Pluripotent stem cells usually come from embryos, while iPSCs are made from adult cells that are changed back to a pluripotent state.
Ethical and Political Misconceptions
There are many ethical and political misconceptions about pluripotent stem cells. These misunderstandings often come from not knowing how they are made or used in research. Some think stem cell research is the same as cloning or that it harms human embryos.
- Using embryonic stem cells does mean destroying embryos, but this is very strictly controlled.
- Not all stem cell research uses embryos. For example, iPSCs are a different option that avoids many ethical issues.
- The rules and funding for stem cell research vary a lot from country to country.
In conclusion, it’s very important to clear up these misconceptions. This will help us understand and use pluripotent stem cells better in medicine and research. By explaining the science and ethics, we can have a more informed talk about their possibilities.
Ethical Considerations Surrounding Embryonic Stem Cells
Ethical debates are key when talking about embryonic stem cells. They touch on moral and religious views. The discussion is complex, involving science and deeply held beliefs about life’s start and embryo morality.
Moral and Religious Perspectives
Different cultures and religions have their own views on embryonic stem cells. Some see using them as okay if it could save lives. Others believe it’s wrong to destroy embryos, even for research.
- Moral Concerns: Debates on the embryo’s moral status and the ethics of using it for research.
- Religious Views: Various religions have different teachings on life’s sanctity and when it starts.
How iPSCs Address Some Ethical Concerns
Induced pluripotent stem cells (iPSCs) offer an alternative to embryonic stem cells. They are made from adult cells that can become many cell types, like embryonic stem cells.
Advantages of iPSCs include:
- They sidestep the ethical issues of destroying embryos.
- They can be made from a patient’s own cells, which might reduce immune rejection in treatments.
iPSCs mark a big step forward in stem cell research. They offer a more ethically acceptable option for regenerative medicine and tissue engineering.
Regulatory Landscape for Stem Cell Research in the United States
Understanding the rules for stem cell research in the U.S. is key to moving the field forward. The country’s rules for stem cell research come from both the federal and state governments. These rules have changed over time.
Federal Policies and Funding Evolution
Federal policies greatly influence stem cell research in the U.S. The Dickey-Wicker Amendment, passed in 1996, bans federal money for research that harms human embryos. This rule has been a big issue, limiting federal funding to stem cell lines made before August 2001.
In 2009, the Obama administration changed this with Executive Order 13505. It removed some limits on human stem cell research and allowed federal money for it. This move was a big step forward, opening up more research and possible treatments.
State-Level Variations in Regulation
While federal rules set a base, states have their own laws, making the rules different everywhere. Some states, like California, support stem cell research with laws and funding.
Other states have stricter laws on embryonic stem cell research. This mix of rules makes it hard for researchers, depending on where they work.
The variety in state laws shows the need for a clear national policy on stem cell research. As the field grows, the rules will likely change too. This will reflect new scientific discoveries, ethical views, and societal changes.
The Future of Pluripotent Stem Cell Technology
The world of pluripotent stem cell technology is on the verge of a big change. New methods and discoveries are leading the way. Researchers are finding new ways to use these cells for medical progress.
Emerging Techniques and Innovations
New advancements in induced pluripotent stem cells (iPSCs) are changing personalized medicine. iPSCs let us make stem cells that match a patient’s needs. This could lead to more effective treatments.
Gene editing tools like CRISPR/Cas9 are also being used. They help fix genetic problems in stem cells. This could help treat genetic diseases.
Organoid cultures are another big step forward. These 3D cell cultures look and act like real organs. They help scientists study diseases and test new treatments. Organoids made from stem cells are changing regenerative medicine.
Potential Breakthroughs on the Horizon
Pluripotent stem cell technology is getting better, and big discoveries are coming. One exciting area is regenerative therapies for diseases like Parkinson’s and diabetes. Scientists aim to create healthy cells to replace damaged ones.
Tissue engineering is another promising field. It combines stem cells with materials and techniques to fix or replace tissues. This could help treat heart problems and spinal cord injuries.
The future of pluripotent stem cell technology looks very promising. Ongoing research and new ideas are leading to major medical breakthroughs. As we learn more about these cells, their ability to help us will grow.
Conclusion: The Evolving Understanding of Pluripotent Stem Cells
Pluripotent stem cells have changed how we see cellular biology and regenerative medicine. These cells can turn into almost any cell type. They show great promise for therapeutic applications. As we learn more, our understanding of these cells and their uses grows.
Stem cells are sorted into types based on how far they can change. Pluripotent stem cells are special because they can change into many cell types. They are key in early development.
Researchers have made big steps in growing and keeping pluripotent stem cells alive. This lets them study how these cells can help in medical treatments. The creation of induced pluripotent stem cells (iPSCs) has opened up new doors. It gives a choice other than using embryonic stem cells, which helps with ethical issues.
As research goes on, pluripotent stem cells will likely become more important in therapeutic applications. They will help lead new discoveries in regenerative medicine and more. The ongoing study and evolving understanding of these cells show how vital they are in today’s biomedical science.
FAQ
What are pluripotent stem cells?
Pluripotent stem cells can turn into almost any cell in the body. They are key for medical research and therapy.
What is the difference between embryonic stem cells and induced pluripotent stem cells?
Embryonic stem cells come from embryos and can become any cell type. Induced pluripotent stem cells (iPSCs) are made from adult cells. They are similar to embryonic stem cells but come from adults.
What does “pluripotent” mean in the context of cell biology?
“Pluripotent” means a stem cell can become every cell type in the body. But it can’t become placental cells or other supporting tissues.
What are the different classes of stem cells?
There are several types of stem cells. Totipotent stem cells can become any cell, including placental cells. Pluripotent stem cells can become almost any cell but not placental cells. Multipotent stem cells can become a few cell types in a lineage. Unipotent stem cells can only become one cell type.
How are embryonic stem cells obtained?
Embryonic stem cells come from the inner cell mass of a blastocyst, an early embryo. They are often donated from embryos left over from in vitro fertilization.
What are the advantages of using induced pluripotent stem cells?
Induced pluripotent stem cells have many benefits. They can create cells specific to a patient, avoiding ethical issues with embryonic stem cells. They also offer a nearly endless supply of cells for research and therapy.
What are the challenges in maintaining pluripotency in stem cell culture?
Keeping stem cells in a pluripotent state is hard. It needs careful control over the culture conditions. If not done right, the cells can start to differentiate.
How are pluripotent stem cells used in regenerative medicine?
Pluripotent stem cells help fix damaged tissues in regenerative medicine. They can turn into specific cells needed for therapy, like neurons for brain disorders or heart cells for heart disease.
What are the ethical considerations surrounding embryonic stem cell research?
Using embryonic stem cells raises ethical questions because it destroys embryos. Some think embryos could become human beings and shouldn’t be used for research. But, induced pluripotent stem cells offer a way without destroying embryos.
How is stem cell research regulated in the United States?
Stem cell research in the U.S. is controlled by laws and guidelines at both the federal and state levels. Federal money for embryonic stem cell research has strict rules. Some states also have their own rules for stem cell research.
What is the future of pluripotent stem cell technology?
The future of pluripotent stem cell technology looks bright. Researchers are working to make cellular reprogramming better. They aim to make stem cell therapies safer and more effective. They also explore new uses in regenerative medicine and tissue engineering.










