Addison’s disease symptoms include fatigue, weight loss, and skin darkening. Learn the warning signs, risk factors, and who is at risk for this condition.
Send us all your questions or requests, and our expert team will assist you.
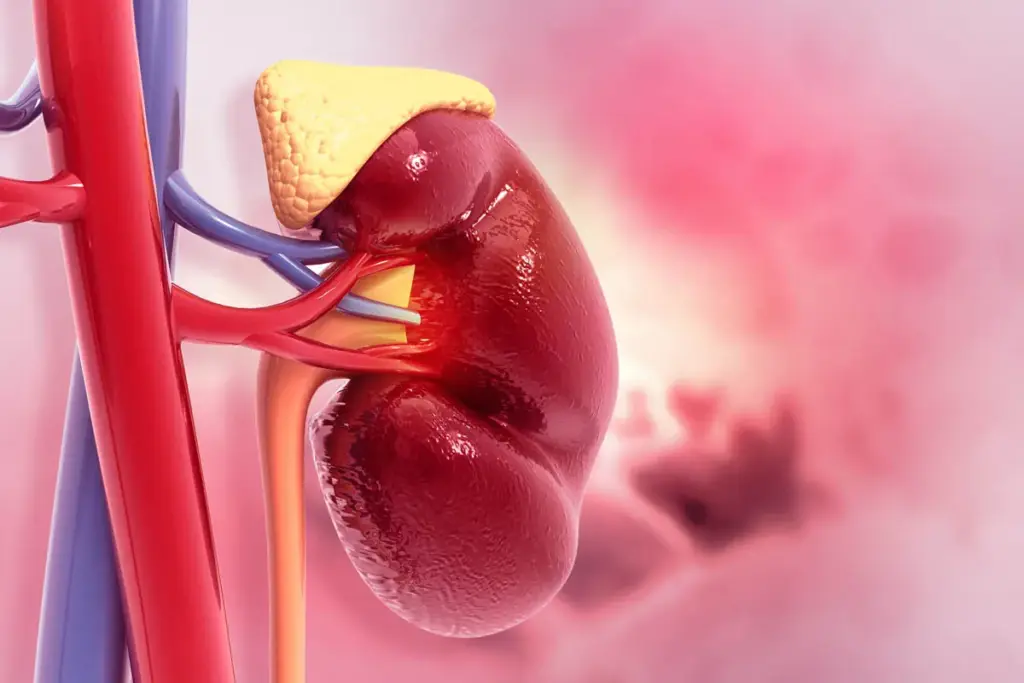
Addison’s disease is often described as a “hidden” illness because the symptoms typically develop very slowly, often over several months or even years. The adrenal glands have a large reserve capacity, meaning symptoms often do not appear until nearly 90% of the adrenal cortex has been destroyed. This slow progression can make early detection difficult, as patients and doctors may attribute the signs to stress or general fatigue.
The “warning signs of Addison’s disease” usually begin with non-specific complaints. Patients may feel a general sense of being unwell without being able to pinpoint the cause. As cortisol and aldosterone levels continue to decline, the body struggles to maintain energy levels and fluid balance, leading to more distinct physical changes.
Key early indicators to watch for include:

While the general symptoms of low cortisol are consistent, there are specific differences depending on the type of adrenal insufficiency. Understanding these nuances helps in distinguishing Primary Adrenal Insufficiency (Addison’s) from Secondary Adrenal Insufficiency.
In this type, the adrenal glands themselves are damaged. The hallmark symptom unique to this type is hyperpigmentation. This occurs because the pituitary gland releases excessive Adrenocorticotropic Hormone (ACTH) to stimulate the failing adrenals. ACTH contains a peptide sequence similar to Melanocyte-Stimulating Hormone (MSH), which stimulates skin cells to produce melanin, causing a “bronze” tan look even in areas not exposed to the sun. Additionally, since the adrenal cortex also produces androgens, women may experience hair loss.
Here, the problem lies in the pituitary gland. Because the pituitary is not producing enough ACTH, the skin does not darken; in fact, skin may appear very pale (alabaster skin). Another key difference relates to mineralocorticoids. In secondary insufficiency, aldosterone levels usually remain normal because they are regulated by the kidneys, not just ACTH. Therefore, patients with secondary insufficiency are less likely to have severe dehydration, salt cravings, or critically low blood pressure compared to those with Addison’s disease.

If Addison’s disease is left untreated, or if a diagnosed patient experiences severe physical stress (like infection or injury) without adjusting their medication, they can enter an acute adrenal crisis, also known as an Addisonian crisis. This is a medical emergency that can be fatal if not treated immediately with intravenous injections of hydrocortisone and saline solution.
It is vital to recognize these “Addison’s disease symptoms” that indicate a crisis state. The onset is sudden and severe, often resembling shock.
Call emergency services immediately if the following symptoms occur:
While the most common cause of Addison’s disease is autoimmune destruction—a factor largely beyond personal control, there are certain elements related to secondary causes and overall adrenal health that fall under “modifiable risk factors”. Managing these can reduce the likelihood of developing insufficiency or triggering a crisis in those who are susceptible.
One significant manageable risk factor involves the use of corticosteroid medications. Long-term use of steroids (like prednisone) for conditions such as asthma or arthritis can suppress the body’s natural cortisol production. If these medications are stopped abruptly, the adrenal glands cannot restart production fast enough, leading to insufficiency. Following a doctor’s tapering schedule strictly is a controllable behavior that prevents this.
Additionally, infection control plays a role. Tuberculosis (TB) is a major cause of Addison’s disease worldwide (though less common in developed nations). Managing risk of exposure to TB and seeking prompt treatment for infections can prevent the adrenal damage associated with these pathogens. For those already diagnosed, “lifestyle” management involves strict adherence to medication schedules and wearing a medical alert bracelet to mitigate the risk of fatal outcomes during emergencies.
Most cases of Addison’s disease stem from non-modifiable factors. Understanding “who is at risk for Addison’s disease” largely centers on genetics and medical history.
Medical Procedures: Individuals who have had surgery to remove part of the adrenal glands (adrenalectomy) for Cushing’s syndrome or tumors are at permanent risk of insufficiency.

While cortisol and aldosterone deficiencies affect both sexes similarly regarding blood pressure and metabolism, “Addison’s disease symptoms” related to androgen deficiency manifest differently in men and women.
The adrenal glands produce dehydroepiandrosterone (DHEA), a precursor to sex hormones. In women, the adrenal glands are the primary source of androgens. Therefore, women with Addison’s disease often experience a loss of axillary (armpit) and pubic hair, dry skin, and a significant decrease in libido (sexual drive).
In men, the testes are the primary producers of testosterone. While the adrenal glands do contribute a small amount, the testicular production is sufficient to maintain secondary sexual characteristics. Consequently, men with Addison’s disease typically do not experience the hair loss or the same degree of sexual dysfunction seen in women, although general fatigue may still impact libido. Both genders, however, are equally susceptible to the fertility issues that can arise from severe, untreated illness.
Assessing “Addison’s disease risk factors” requires looking at the complete clinical picture. A single risk factor, like having a relative with thyroid disease, does not guarantee you will develop Addison’s, but it increases the statistical probability. The “total risk” is highest for individuals who fall into the category of Autoimmune Polyglandular Syndrome.
Send us all your questions or requests, and our expert team will assist you.
The primary warning signs include extreme fatigue that doesn’t improve with rest, unexplained weight loss, salt cravings, low blood pressure (dizziness upon standing), and hyperpigmentation (darkening) of the skin. Gastrointestinal issues like nausea are also common.
Individuals with other autoimmune diseases are at the highest risk. This includes people with Type 1 Diabetes, Hashimoto’s thyroiditis, Graves’ disease, or vitiligo. Those with chronic infections like tuberculosis or HIV are also at increased risk.
Yes. While general symptoms like fatigue and low blood pressure are the same, women often experience specific symptoms related to androgen deficiency, such as loss of pubic and underarm hair and a decrease in sexual drive. Men typically do not experience these sexual side effects to the same degree.
There are few lifestyle causes for primary Addison’s, as it is mostly autoimmune. However, the abrupt cessation of long-term corticosteroid medication is a major lifestyle/behavioral factor that causes secondary adrenal insufficiency. Neglecting treatment for infections like TB also increases risk.
Yes, the predisposition to autoimmune conditions is hereditary. While you may not inherit Addison’s disease directly, you can inherit the genetic susceptibility (gene variants) that makes your immune system more likely to attack your own tissues, increasing the risk of developing it.


Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)