Last Updated on October 28, 2025 by
At Liv Hospital, we know how vital a successful bone marrow extraction process is. The harvesting bone marrow procedure is a special surgery. It’s used to get stem cells for bone marrow transplantation. This process needs great care and the latest techniques to protect both the donor and the recipient.
We have a detailed step-by-step guide for the harvesting bone marrow procedure. Our goal is to keep both the donor and the recipient safe and healthy. Our team of experts is committed to top-notch healthcare. They also offer full support to international patients. By understanding the bone marrow transplant surgery, we can see the complexity and care it involves.
Key Takeaways
- The harvesting bone marrow procedure is key for bone marrow transplantation.
- Liv Hospital uses the latest protocols for the best care.
- The process involves a special surgical technique.
- Great care and precision are essential in the bone marrow extraction process.
- Our team focuses on the well-being of both the donor and the recipient.
Understanding Bone Marrow and Its Role in Transplantation

Bone marrow is a key part of our body, found in bones like hips and thighbones. It makes blood cells, which are vital for our health. These cells include red blood cells, white blood cells, and platelets.
The Composition and Function of Bone Marrow
Bone marrow is made up of stem cells, fat cells, and blood vessels. Its main job is to create blood cells that keep us healthy. Stem cells in bone marrow can turn into different blood cells, helping our body fix and grow.
Types of Stem Cells Found in Bone Marrow
Bone marrow has two main stem cell types: hematopoietic and mesenchymal. Hematopoietic stem cells make blood cells. Mesenchymal stem cells can become bone, cartilage, or fat cells. These stem cells are essential for transplant success.
Transplantation Applications and Success Rates
Bone marrow transplants help treat diseases like cancer and blood disorders. Success depends on donor and recipient match, recipient’s health, and the disease type.
| Disease | Success Rate | Number of Transplants |
|---|---|---|
| Leukemia | 60-80% | 1000+ |
| Lymphoma | 50-70% | 500+ |
| Aplastic Anemia | 70-90% | 200+ |
The table shows bone marrow transplant success rates for different diseases. Success rates vary by disease. Yet, bone marrow transplants save lives for many worldwide.
Medical Indications for Bone Marrow Transplants
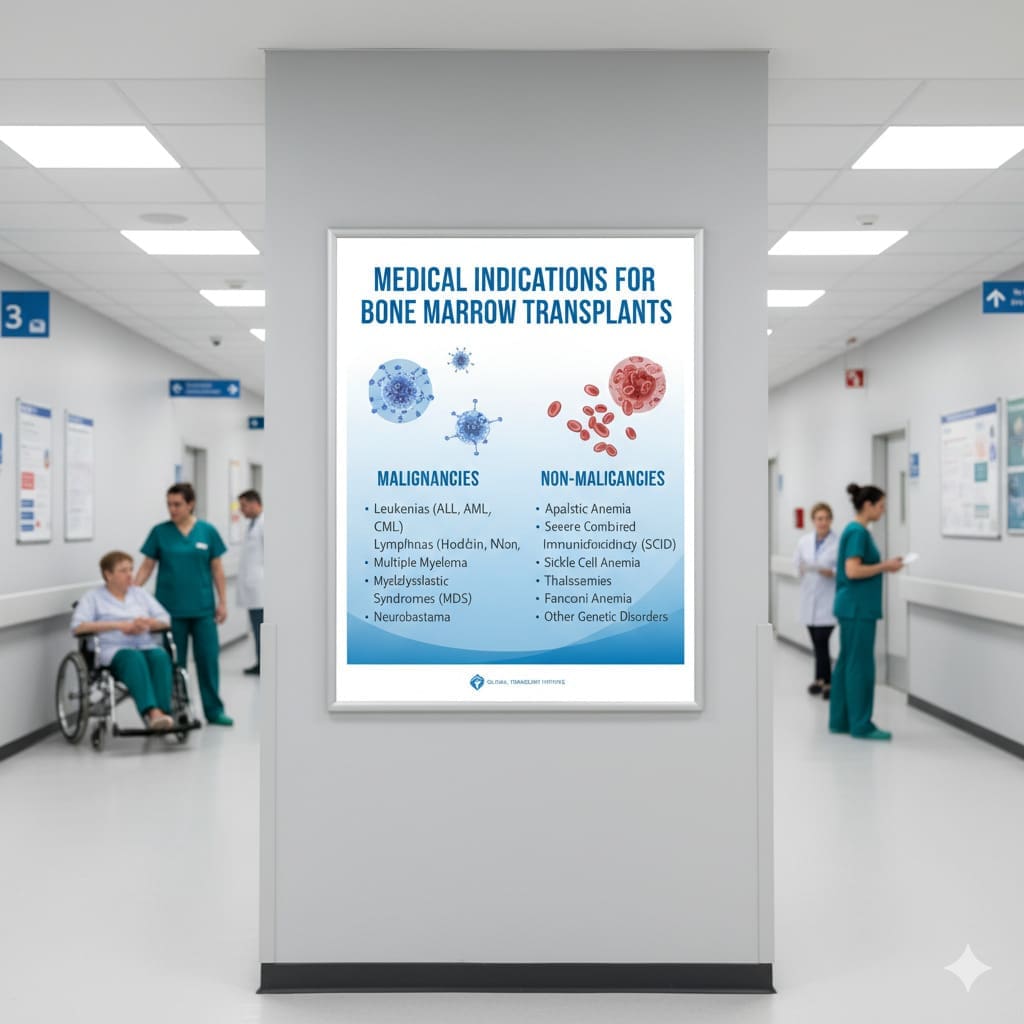
Doctors often suggest bone marrow transplants for certain blood cancers or non-cancerous conditions. This treatment is key for serious diseases. The choice to get a transplant depends on the patient’s health history, current condition, and disease severity.
Hematologic Malignancies Requiring Transplantation
Hematologic malignancies affect the blood, bone marrow, and lymph nodes. These include leukemia, lymphoma, and multiple myeloma. For these cancers, a bone marrow transplant is often considered.
This is when the cancer hasn’t responded to usual treatments or has come back. The transplant uses high-dose chemotherapy and/or radiation. Then, healthy stem cells are given to replace the bad cells and fix the bone marrow.
Non-Malignant Conditions Treated with Bone Marrow
Bone marrow transplants also help with non-cancerous conditions. These include severe aplastic anemia, sickle cell disease, and thalassemia major. The aim is to swap the patient’s bad bone marrow with healthy one.
Determining Transplant Eligibility
To see if a patient can get a bone marrow transplant, doctors check several things. They look at the patient’s health, disease details, and if a good donor is available. This includes many tests to make sure the transplant is safe and will help the patient.
They consider the patient’s age, health, and disease stage. They also check for any other health issues and if the patient is mentally prepared for the transplant.
Donor Selection and Preparation Process
The journey to a successful bone marrow transplant starts with choosing the right donor. This process involves several steps to make sure the donor is a good match and ready for the transplant.
HLA Typing and Donor Matching Criteria
Human Leukocyte Antigen (HLA) typing is key in picking a donor. It checks if the donor’s genes match the recipient’s. We use the latest HLA typing methods to find donors who are a good match.
We look at how well the HLA types match, the donor’s age, health, and genetic tests. A good match is important to avoid complications and ensure the transplant works.
Required Pre-Donation Testing and Screening
Before donating, donors go through a lot of tests. These include:
- Infectious disease screening (e.g., HIV, hepatitis)
- Blood tests to check overall health
- Genetic testing for genetic disorders
- Review of medical history for health issues
These tests help find any risks in the donation process. They make sure the donor is healthy enough for the procedure.
Informed Consent and Psychological Preparation
Getting informed consent is very important. We make sure donors know the risks and benefits of bone marrow donation. We talk about the procedure, possible problems, and recovery.
Preparing mentally is also key. We offer counseling and support. This helps donors deal with the emotional side of donation.
| Donor Evaluation Criteria | Description | Importance Level |
|---|---|---|
| HLA Typing | Genetic compatibility testing | High |
| Infectious Disease Screening | Testing for infectious diseases | High |
| Medical History Review | Evaluation of donor’s medical history | Medium |
| Psychological Evaluation | Assessment of donor’s mental preparedness | Medium |
By carefully checking these criteria, we make sure donors are well chosen and prepared. This helps make the bone marrow donation process successful.
The Harvesting Bone Marrow Procedure: Overview and Planning
Bone marrow harvesting is a detailed process. It’s key for a successful bone marrow transplant. Each step is planned carefully to get the best marrow quality.
Procedure Duration and Resource Requirements
The bone marrow harvesting time can be 1 to 3 hours. It depends on the case’s complexity and marrow volume. A skilled team and the right tools are essential for success.
Here’s what we need:
- Specialized surgical equipment
- Monitoring devices for patient safety
- A sterile environment to minimize infection risk
Team Composition and Responsibilities
The team includes surgeons, anesthesiologists, nurses, and support staff. Each plays a vital role in the procedure’s success.
| Team Member | Responsibilities |
|---|---|
| Surgeon | Performs the bone marrow harvesting, ensuring safe and effective extraction. |
| Anesthesiologist | Administers anesthesia and monitors the patient’s vital signs during the procedure. |
| Nursing Staff | Assists during the procedure, prepares the patient, and manages post-procedure care. |
Facility and Equipment Preparation
Preparing the facility and equipment is vital. We make sure all tools are sterilized and ready. A clean environment is also critical to avoid complications.
With thorough planning and preparation, we aim for a successful bone marrow harvesting procedure. This ensures the best outcome for our patients.
Pre-Operative Protocol and Anesthesia Administration
Before the bone marrow extraction surgery, we follow a strict pre-operative protocol. This makes sure the procedure is a success and keeps the donor safe and comfortable.
Patient Preparation and Positioning
Getting the donor ready is essential for a good bone marrow harvesting. They lie on their stomach to make it easy to get to the bone marrow. “The right position is key for a successful procedure,” as bone marrow harvesting guidelines say. We make sure they’re comfy and stable to avoid any movement during the surgery.
General Anesthesia Induction and Monitoring
We use general anesthesia to keep the donor comfortable. We watch their vital signs closely during the surgery. Anesthesia guidelines for surgical procedures tell us to be ready for any issues. Our advanced monitoring tools help keep everything safe.
Surgical Site Preparation and Draping
After the donor is set and the anesthesia kicks in, we clean and prepare the area. We clean the area around the posterior iliac crest and cover it with sterile drapes to prevent infection. As
“The sterile technique is key to avoiding surgical site infections,”
our surgical team follows this rule closely during the bone marrow harvesting.
By carefully following these steps, we make sure the bone marrow extraction goes smoothly. This helps the bone marrow transplant surgery succeed.
Step-by-Step Bone Marrow Extraction Technique
To successfully harvest bone marrow, we must follow a detailed step-by-step technique. This ensures we get enough high-quality marrow for transplantation.
Posterior Iliac Crest Identification and Marking
The first step is to identify and mark the posterior iliac crest. This area is key because it tells us where to put the bone marrow needle. We use images and knowledge of anatomy to find and mark this spot.
Needle Insertion and Advancement Methodology
After finding the posterior iliac crest, we insert the needle. We move the needle slowly through the bone into the marrow. This step needs precision to avoid harm and place the needle right in the marrow.
We advance the needle gently, sometimes twisting it to go through the bone cortex.
Aspiration Technique and Volume Management
We use a syringe attached to the needle to aspirate the marrow. We manage the volume to get enough without stressing the donor.
The aspiration is done carefully to protect the marrow cells. This way, we get high-quality marrow.
Site Rotation and Multiple Harvest Strategy
To get more marrow, we rotate the site and harvest from different spots. This method helps us collect enough marrow safely.
| Harvest Location | Aspiration Volume (mL) | Needle Gauge |
|---|---|---|
| Posterior Iliac Crest | 50-100 | 11-13 |
| Anterior Iliac Crest | 30-70 | 11-13 |
By following this detailed technique, we make sure the procedure is safe and effective for everyone involved.
Processing Harvested Bone Marrow for Transplantation
Processing bone marrow is a detailed task. It’s essential to keep stem cells alive and healthy. This step is key to a successful transplant.
Initial Filtration and Anti-Coagulation
The first step is initial filtration. It removes bone spicules, debris, and fat. Filters with small pores are used to clear out contaminants.
Next, anti-coagulation is done. This stops the bone marrow from clotting. An anti-coagulant like heparin or acid-citrate-dextrose (ACD) is added.
Stem Cell Concentration Methods
After filtering and anti-coagulating, stem cells are concentrated. This is done through density gradient centrifugation or cell separation. The goal is to get the stem cells alone.
We use automated cell separators to improve the stem cell quality.
Quality Assessment and Cell Counting
After concentrating stem cells, their quality is checked. This includes counting cells and checking their health. Flow cytometry and trypan blue exclusion are used.
The results show if the bone marrow is ready for transplant.
Cryopreservation Techniques for Delayed Transplantation
If the transplant is delayed, the stem cells are frozen. This is called cryopreservation. Cryoprotectants prevent damage from ice crystals.
The frozen cells are stored in liquid nitrogen. When it’s time, they’re thawed and ready for the transplant.
Immediate Post-Procedure Donor Management
The time right after the procedure is key for taking care of the donor. We watch them closely and provide support. Moving the donor from the operating room to the recovery area is our main goal.
Recovery Room Monitoring Parameters
In the recovery room, we keep a close eye on the donor’s vital signs. This includes heart rate, blood pressure, and oxygen levels. Continuous monitoring helps us catch any problems early.
We also check how awake the donor is, their pain, and comfort. The recovery room team is ready to handle any issues that might come up. They make sure donors feel safe and comfortable.
Pain Management and Hydration Protocol
Managing pain is a big part of taking care of donors after the procedure. We use both medicine and other methods to help with pain. Each donor gets a pain plan that fits their needs and health history.
Drinking enough water is also important for donors. We make sure they get enough fluids to replace lost blood and stay hydrated. This helps prevent dehydration and supports their recovery.
Early Complication Assessment and Intervention
Bone marrow harvesting is usually safe, but complications can happen. Our team is always on the lookout for signs of trouble, like bleeding or infection.
By catching problems early, we can act fast to keep the donor safe. This is a big part of our care for donors. It shows our dedication to providing top-notch, patient-focused care.
Potential Complications and Risk Mitigation
It’s important to know the risks of bone marrow harvesting to manage them well. The procedure is mostly safe, but there are dangers both donors and doctors should watch out for.
Procedure-Related Complications
Bone marrow harvesting can cause several problems. These include:
- Pain and discomfort at the harvest site
- Infection or bleeding at the needle insertion site
- Damage to surrounding tissues or nerves
- Reaction to the anesthesia used during the procedure
To lower these risks, careful planning, precise technique, and good post-procedure care are key.
Anesthesia-Related Complications
Because bone marrow harvesting often uses general anesthesia or conscious sedation, there are anesthesia-related risks. These can include:
- Respiratory complications
- Cardiovascular issues
- Allergic reactions to anesthetic agents
We make sure our anesthesia team is skilled and that donors get a full pre-anesthetic check-up to reduce these risks.
Long-Term Donor Considerations
While bone marrow harvesting is usually safe in the long run, donors should think about possible long-term effects. These include:
| Consideration | Description | Mitigation Strategy |
|---|---|---|
| Persistent Pain | Some donors may have pain or discomfort that lasts after they recover. | Good pain management and follow-up care. |
| Fatigue | Donors might feel tired or weak after the procedure. | Rest, proper nutrition, and slow return to activities. |
| Emotional Impact | The donation process can affect donors emotionally. | Supportive care and counseling services. |
Knowing these long-term considerations helps donors prepare for their recovery and overall health.
Donor Recovery Timeline and Bone Marrow Regeneration
Knowing how long it takes to recover is key for bone marrow donors. It helps them plan and get back to their usual life. The recovery journey has different stages, from right after the procedure to when the bone marrow fully regenerates.
First 48 Hours Post-Procedure Care
The first 48 hours after bone marrow harvesting are very important. Monitoring for any issues and following the doctor’s advice are critical. Donors should rest and not do too much.
“The first 48 hours are key for a smooth recovery,” says Dr. Jane Smith, a bone marrow transplant expert.
Donors might feel tired, have pain, and discomfort at the site. It’s important to manage pain well and stay hydrated.
One Week to One Month Recovery Expectations
After the first 48 hours, donors start to feel better slowly. They can start doing light things in one to two weeks. But, it’s important to listen to their doctor about when to start doing more.
By the end of a month, most donors have made a lot of progress. But, how fast they recover depends on their health and the procedure’s extent.
Complete Bone Marrow Regeneration Process
Bone marrow regeneration takes 4 to 6 weeks. During this time, the body makes new marrow. This is important for the donor to get back to full health.
Return to Normal Activities Guidelines
Donors should slowly get back to doing things, avoiding heavy work. The time it takes to get back to normal varies. It depends on how well they’re recovering.
By following these guidelines, bone marrow donors can recover safely. They can then get back to their usual life, feeling healthy and full of energy.
Alternative Stem Cell Collection Methods Compared
Stem cell collection has grown beyond just bone marrow. New methods offer different benefits and challenges. It’s key to know their differences and uses in stem cell transplants.
Peripheral Blood Stem Cell Collection
Peripheral blood stem cell (PBSC) collection is a popular choice. It moves stem cells from bone marrow to blood using growth factors. Then, apheresis collects these cells. PBSC collection is less invasive than bone marrow harvesting and can be done as an outpatient.
Cord Blood Banking and Utilization
Cord blood banking collects stem cells from the umbilical cord and placenta after birth. These cells are frozen for future use in transplants. Cord blood stem cells are immunologically naive, which lowers the risk of graft-versus-host disease. This makes them a good choice for some patients.
Comparative Analysis of Collection Efficiency
Stem cell collection methods vary in efficiency. Factors like stem cell yield, collection ease, and risks are important. PBSC collection usually gets more stem cells than cord blood, which is better for adult transplants. But, cord blood is easier to find and can be used with less strict HLA matches.
Selecting the Optimal Collection Method
Choosing the right stem cell collection method depends on many things. These include the patient’s health, the transplant type, and donor availability. A multidisciplinary approach is needed to pick the best method for each case. This balances the benefits and risks of each technique.
Understanding the various stem cell collection methods helps healthcare providers make better choices. This improves outcomes in stem cell transplants.
Conclusion
Understanding the bone marrow harvesting process is key for successful bone marrow transplant surgery. This complex task includes choosing the right donor, doing detailed HLA typing, and following a precise procedure. It’s all about getting the best bone marrow for the transplant.
This guide shows how important teamwork is in bone marrow donation. From the first screening to aftercare, a coordinated effort is vital. It helps reduce risks and improves results for both donors and those receiving the transplant.
As we keep improving in bone marrow transplantation, we need to make our methods better. The bone marrow harvesting process is a critical part of this surgery. It requires skill, knowledge, and care for the patients.
Following the guidelines and best practices helps ensure bone marrow donation is done carefully. This improves the success of bone marrow transplant surgery. It also makes a big difference in the lives of patients all over the world.
FAQ
What is bone marrow harvesting?
Bone marrow harvesting is a medical process. It takes bone marrow from a donor’s body, usually from the hip. This marrow is then given to someone else who needs it.
What are the risks associated with bone marrow harvesting?
Risks include pain, bleeding, and infection. There’s also a chance of damage to the bone or tissue. These risks are rare but serious.
How is a bone marrow donor selected?
Donors are chosen based on HLA typing. This ensures they match the person who will receive the marrow. They also go through health checks to make sure they’re a good match.
What is the bone marrow extraction process?
First, the donor’s hip is located. Then, a needle is inserted to get the marrow. The whole process is done under anesthesia to make it painless.
How is harvested bone marrow processed for transplantation?
The marrow is first filtered and then its stem cells are concentrated. It’s checked for quality and frozen for later use in the transplant.
What is the recovery time for bone marrow donors?
Donors usually recover in a few days to weeks. Most can get back to normal in one to two weeks. It takes several weeks for the bone marrow to fully regenerate.
Are there alternative methods for stem cell collection?
Yes, there are other ways to collect stem cells. These include taking them from the blood or from umbilical cord blood. The choice depends on the recipient’s needs and the donor’s health.
What is the success rate of bone marrow transplants?
Success rates vary. They depend on the condition being treated, the match between donor and recipient, and the recipient’s health.
How is pain managed after bone marrow harvesting?
Pain is managed with medicine and other treatments. This helps the donor feel better and recover faster.
Can bone marrow donors experience long-term complications?
Rarely, donors might face long-term issues. These could be damage to the bone or tissue. They’re closely monitored and given advice on managing any long-term effects.
What is the role of HLA typing in bone marrow donation?
HLA typing is key. It makes sure the donor and recipient are compatible. This reduces the risk of complications and improves the transplant’s success.
References
Texas Children’s Hospital. Bone Marrow Harvest. Available at: https://www.texaschildrens.org/content/conditions/bone-marrow-harvest
Together by St. Judeâ„¢. Stem Cell Collection from Bone Marrow. Available at: https://together.stjude.org/en-us/treatment-tests-procedures/procedures/stem-cell-collection-from-bone-marrow.html
Blood & Marrow Transplant Information Network (BMT Infonet). How Blood Stem Cells Are Collected. Available at: https://bmtinfonet.org/transplant-article/how-blood-stem-cells-are-collected
National Marrow Donor Program (NMDP). Donate Bone Marrow “ Join the Registry. Available at: https://www.nmdp.org/en/get-involved/join-the-registry/donate-bone-marrow
National Center for Biotechnology Information (NCBI). Bone Marrow Harvest “ StatPearls. Available at: https://www.ncbi.nlm.nih.gov/books/NBK608245/
FAQ
What is bone marrow harvesting?
Bone marrow harvesting is a medical process. It takes bone marrow from a donor’s body, usually from the hip. This marrow is then given to someone else who needs it.
What are the risks associated with bone marrow harvesting?
Risks include pain, bleeding, and infection. There’s also a chance of damage to the bone or tissue. These risks are rare but serious.
How is a bone marrow donor selected?
Donors are chosen based on HLA typing. This ensures they match the person who will receive the marrow. They also go through health checks to make sure they’re a good match.
What is the bone marrow extraction process?
First, the donor’s hip is located. Then, a needle is inserted to get the marrow. The whole process is done under anesthesia to make it painless.
How is harvested bone marrow processed for transplantation?
The marrow is first filtered and then its stem cells are concentrated. It’s checked for quality and frozen for later use in the transplant.
What is the recovery time for bone marrow donors?
Donors usually recover in a few days to weeks. Most can get back to normal in one to two weeks. It takes several weeks for the bone marrow to fully regenerate.
Are there alternative methods for stem cell collection?
Yes, there are other ways to collect stem cells. These include taking them from the blood or from umbilical cord blood. The choice depends on the recipient’s needs and the donor’s health.
What is the success rate of bone marrow transplants?
Success rates vary. They depend on the condition being treated, the match between donor and recipient, and the recipient’s health.
How is pain managed after bone marrow harvesting?
Pain is managed with medicine and other treatments. This helps the donor feel better and recover faster.
Can bone marrow donors experience long-term complications?
Rarely, donors might face long-term issues. These could be damage to the bone or tissue. They’re closely monitored and given advice on managing any long-term effects.
What is the role of HLA typing in bone marrow donation?
HLA typing is key. It makes sure the donor and recipient are compatible. This reduces the risk of complications and improves the transplant’s success.





