Anemia is when there aren’t enough red blood cells or hemoglobin. It’s a big problem for people on dialysis. For those with end-stage renal disease (ESRD), anemia can really hurt their quality of life. It makes them feel tired, sad, and less able to exercise.
At Liv Hospital, we know how important it is to manage anemia well. Treating anemia makes patients feel better and can even save their lives. It’s a big deal for those on dialysis.
Key Takeaways
- Anemia is a common issue for dialysis patients, affecting their quality of life.
- Effective management of anemia is key to better health outcomes.
- Treating anemia can help reduce fatigue, depression, and other symptoms.
- Liv Hospital is dedicated to providing top-notch treatment for anemia.
- Early treatment is essential for managing anemia and lowering mortality risk.
Understanding Anemia in Kidney Failure
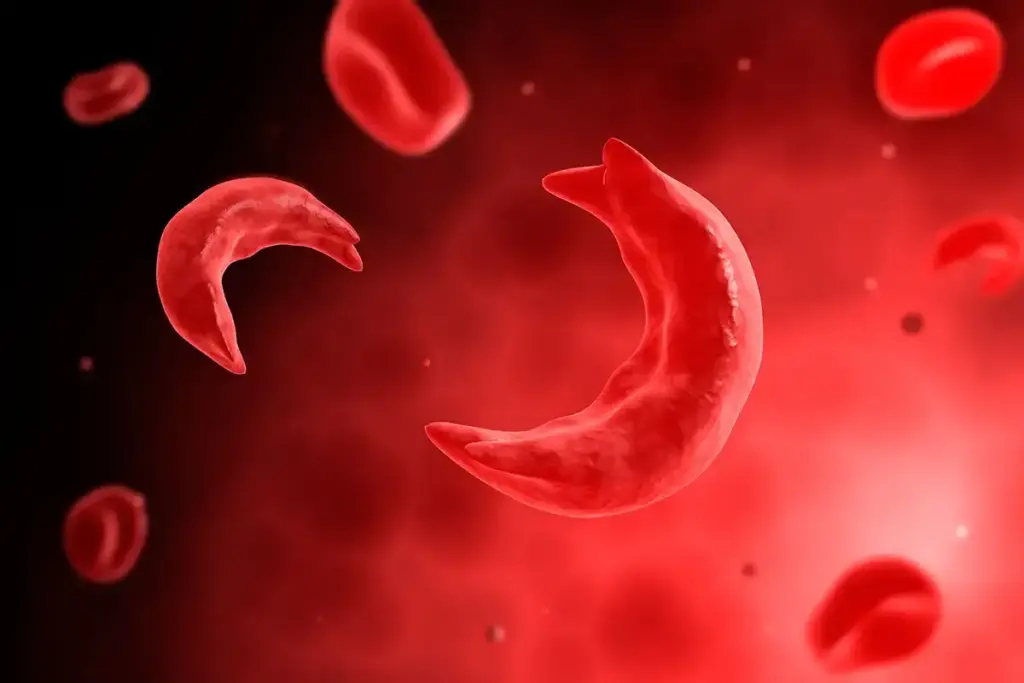
Kidney failure often leads to anemia, a condition where there aren’t enough healthy red blood cells. These cells carry oxygen to the body’s tissues. Anemia makes you feel weak and tired because you lack energy.
Clinical Definition and Diagnostic Criteria
Anemia is defined by a hemoglobin level below 13 g/dL for men and 12 g/dL for women. In kidney failure, anemia is mainly due to a lack of erythropoietin. This hormone is made by the kidneys and helps make red blood cells.
Erythropoietin deficiency is a key factor in anemia for ESRD patients. The kidneys produce erythropoietin when oxygen levels are low. But in kidney failure, they can’t make enough, leading to anemia.
Prevalence and Impact on Patient Outcomes
Anemia is common in ESRD patients, affecting most on dialysis. It not only lowers quality of life but also raises the risk of heart disease and death.
| Condition | Prevalence of Anemia | Impact on Patient Outcomes |
| ESRD Patients | High (>80%) | Increased risk of cardiovascular disease, reduced quality of life |
| Chronic Kidney Disease | Variable (dependent on stage) | Progression of kidney disease, increased morbidity |
It’s important to understand anemia in kidney failure to manage patient care well. By tackling the causes and symptoms, healthcare providers can improve patient outcomes and quality of life.
The Relationship Between Dialysis and Anemia

Dialysis and anemia are closely linked, mainly due to a lack of erythropoietin and other ESRD complications. Anemia is common among dialysis patients. It greatly affects their life quality and health.
Erythropoietin Deficiency in ESRD
Healthy kidneys make erythropoietin (EPO), a hormone that helps make red blood cells. In ESRD, kidneys can’t make enough EPO. This leads to anemia. Erythropoietin deficiency is a hallmark of CKD and ESRD, directly correlating with the degree of kidney dysfunction.
Without enough EPO, the body can’t make enough red blood cells. This causes anemia. Anemia affects energy levels and overall health. It also impacts heart health and survival.
Contributing Factors to Renal Anemia
Other factors also cause anemia in dialysis patients. These include functional iron deficiency and chronic inflammation. These can stop the body from making red blood cells. Red blood cells also don’t last as long in ESRD patients.
These factors make managing anemia in dialysis patients complex. It’s important to understand these causes. This helps in finding effective treatments for anemia.
By understanding the link between dialysis and anemia, healthcare providers can give better care. This improves the lives of ESRD patients.
Evidence-Based Treatment Approaches
Treating anemia in dialysis patients needs a mix of therapies. We focus on the patient’s specific needs.
Effective Therapies
Intravenous iron therapy is key for iron deficiency, common in patients with low hemoglobin. Keeping TSAT levels normal is important for iron use.
Erythropoiesis-stimulating agents (ESAs) help make more red blood cells. This improves anemia treatment. We adjust ESA doses to hit target hemoglobin levels safely.
Nutritional Support
Therapies and nutrition are key for managing anemia. We stress the need for enough iron for patients with low hemoglobin. This helps support red blood cell production.
Using these proven treatments, we can better manage anemia in dialysis patients. This improves their life quality and health outcomes.
FAQ:
What is anemia, and how does it affect dialysis patients?
Anemia is when there’s not enough red blood cells or hemoglobin in the blood. It’s common in dialysis patients and can make life harder. It causes fatigue, weakness, and shortness of breath.
Why does ESRD cause anemia?
ESRD leads to anemia because the kidneys don’t make enough erythropoietin. This hormone helps make red blood cells. Without enough, patients don’t have enough red blood cells.
What is the role of erythropoietin deficiency in anemia in ESRD patients?
Erythropoietin is key for making red blood cells. Without enough, patients can’t make enough red blood cells. This leads to anemia.
How does dialysis impact anemia in patients with kidney failure?
Dialysis can affect anemia in several ways. It removes waste but also nutrients like iron. The process can also cause inflammation, making anemia worse.
What are the symptoms of renal anemia?
Symptoms include fatigue, weakness, pale skin, shortness of breath, and dizziness. These symptoms can really affect a patient’s life. It’s important to manage anemia well.
How is anemia diagnosed in patients with kidney failure?
Doctors use blood tests to check for anemia. They look at hemoglobin and hematocrit levels. They also check iron levels and other factors to find the cause and treat it.
What is the normal TSAT level, and why is it important?
TSAT shows how much iron is in the blood. A normal TSAT is between 20% and 50%. It helps doctors diagnose and treat iron deficiency anemia.
Can anemia cause kidney failure?
Anemia is a complication of kidney failure, not a cause. But, untreated anemia can make kidney function worse and affect overall health.
How is anemia treated in dialysis patients?
Treatment includes intravenous iron, ESAs, and nutritional support. It’s important to get enough iron, vitamin B12, and folate.
What is the role of intravenous iron therapy in managing anemia?
Intravenous iron therapy helps replace iron and support red blood cell production. It’s useful for patients who can’t take iron by mouth or have severe deficiency.
How do ESAs work in treating anemia in ESRD patients?
ESAs help make more red blood cells by mimicking erythropoietin. They increase hemoglobin levels, reduce blood transfusions, and improve life quality.
References:
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10719594/























