Explore advanced kidney disease treatment at Liv Hospital. From 2026 drug therapies to robotic-assisted transplants, we offer world-class renal care in Turkey.
Send us all your questions or requests, and our expert team will assist you.
A diagnosis of kidney disease is no longer a path to limited options. Modern kidney disease treatment has evolved into a highly personalized field where technology, pharmacology, and surgical precision converge. At Liv Hospital, we move beyond basic management, offering international patients access to the latest FDA-approved medications, advanced dialysis modalities, and world-class transplant programs. Our goal is not just to sustain life, but to restore its quality through a multidisciplinary approach that targets the root cause of renal decline.
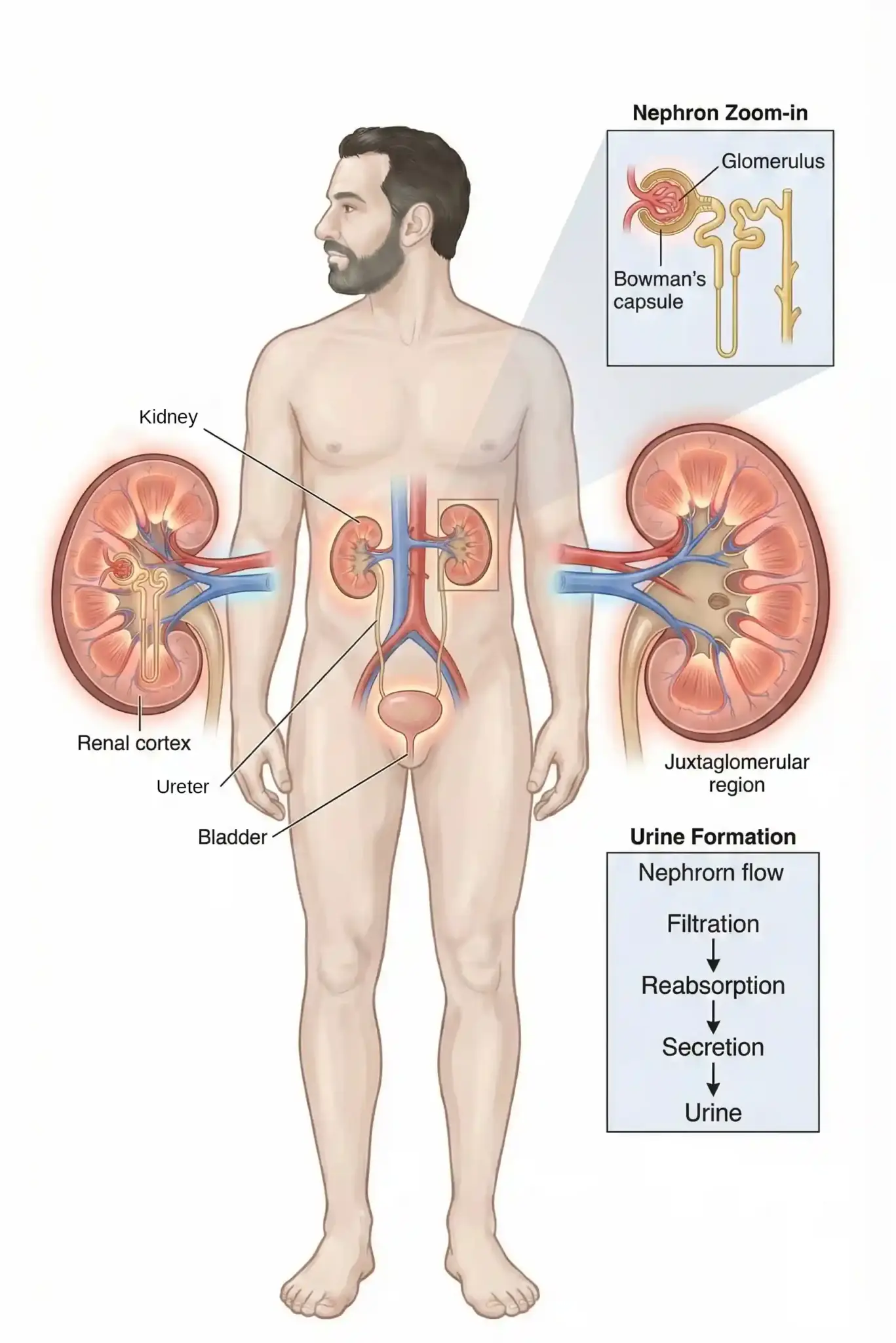
The kidneys are involved in everything from blood pressure to bone density, so treatment must be equally comprehensive. The primary objectives of our nephrology team include:

We are currently in a “Golden Age” of nephrological pharmacology. Many conditions that once led inevitably to dialysis can now be managed with targeted therapies.
When kidneys can no longer perform their duties (End-Stage Renal Disease), dialysis becomes a vital bridge. Liv Hospital’s dialysis center is equipped with the latest “High-Flux” hemodialysis and hemodiafiltration (HDF) technologies, which clear larger “middle molecules” that traditional dialysis might miss.
Our options include:

For many, a transplant is the closest thing to a “cure.” Liv Hospital is a leading international reference center for kidney transplantation, with a success rate of 96% and over 5,000 procedures performed to date.
Send us all your questions or requests, and our expert team will assist you.

Treatment does not end when you leave the hospital. Renal health requires lifelong vigilance. At Liv Hospital, our international patient follow-up program is designed for those returning to the US or other countries.

Medical tourism for nephrology requires a balance of high technology and logistical ease. Liv Hospital provides a seamless experience, including airport transfers, English-speaking patient coordinators, and a “Renal Board” review of your case before you even arrive in Turkey. By combining the surgical expertise of our transplant team with the latest 2026 medical protocols, we provide a level of care that matches top US institutions at a fraction of the cost.
Hemodialysis is typically done three times a week for about four hours at a time, whereas peritoneal dialysis is usually done every day, often while you sleep.
Acute kidney injury can often be reversed if treated quickly, but chronic kidney disease usually involves permanent scarring that cannot be fixed, only managed to prevent worsening.
Anti-rejection medicines can increase your risk of infection, cause weight gain, increase blood pressure, and sometimes increase the risk of developing certain cancers and diabetes.
No, the diet changes depending on your stage of kidney disease; early stages may need low salt, while later stages or dialysis require restrictions on potassium, phosphorus, and fluids.
Life expectancy on dialysis varies widely by age and other health conditions; some people live 5 to 10 years, while others can live 20 years or more with good care.


Shoulder pain is a big problem for many adults. Over 1 million people in the United States go to the doctor for shoulder issues every

Nearly 25% of adults over 55 deal with knee pain. This greatly affects their life quality. As we get older, knee pain becomes more common.
Knee bursitis is a painful condition that affects millions of people worldwide. It causes discomfort and limits mobility. Inflammation of the bursae around the knee

Scoliosis affects millions, causing back pain and lowering quality of life. It’s key to manage scoliosis well to ease pain and avoid more problems. We’ll
Shoulder tendonitis is a common issue that affects millions globally. It causes a lot of pain and makes it hard to move. Inflammation of the

Did you know ignoring Achilles tendonitis can cause chronic problems? These issues can affect your daily life. Untreated, it can turn into chronic achilles tendonitis

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)