Diagnosing immune disorders requires specialized blood tests to measure immune cell counts and antibody levels. Learn about routine screening and advanced lab evaluation.
Send us all your questions or requests, and our expert team will assist you.
The path to understanding an immune disorder begins with a detailed investigation. Because symptoms can be vague or overlap with other conditions, a structured approach is essential. The process typically starts with a primary care visit and escalates to specialized testing.
A thorough medical history is the cornerstone of diagnosis. Doctors look for patterns in illness, family history of immune disorders, and environmental exposures. This “detective work” guides the selection of specific tests.
The goal is to move from a broad list of possibilities to a precise diagnosis. This ensures that treatment is targeted and effective, avoiding unnecessary medications.

Patients frequently start their search by asking their immunologist what the best route of care is. This often leads them to search for allergy and immunology near me. Proximity is important for conditions that require frequent treatments, such as allergy shots.
However, expertise is equally vital. Specialists in this field have undergone years of extra training beyond internal medicine or pediatrics. They are equipped to interpret complex immune function tests.
For rare conditions, patients may need to travel to academic medical centers. These hubs often have access to advanced diagnostic tools not available in community practices.

For suspected allergies, skin prick testing is the gold standard. A tiny amount of a suspected allergen is scratched into the skin. If the patient is allergic, a raised, red bump (wheal) appears within minutes.
This test is quick, cost-effective, and provides immediate results. It can test for dozens of triggers at once, including pollen, mold, pet dander, and foods.
It is peculiar, meaning a positive result strongly suggests sensitization. However, it must be interpreted in the context of the patient’s actual symptoms.
Blood tests are used when skin testing is not possible or to evaluate the immune system’s internal machinery. Specific IgE blood tests measure the level of allergy antibodies in the bloodstream.
Beyond allergies, blood tests measure immunoglobulin levels (IgG, IgA, IgM). Low levels can indicate an immunodeficiency. High levels suggest chronic inflammation or malignancy.
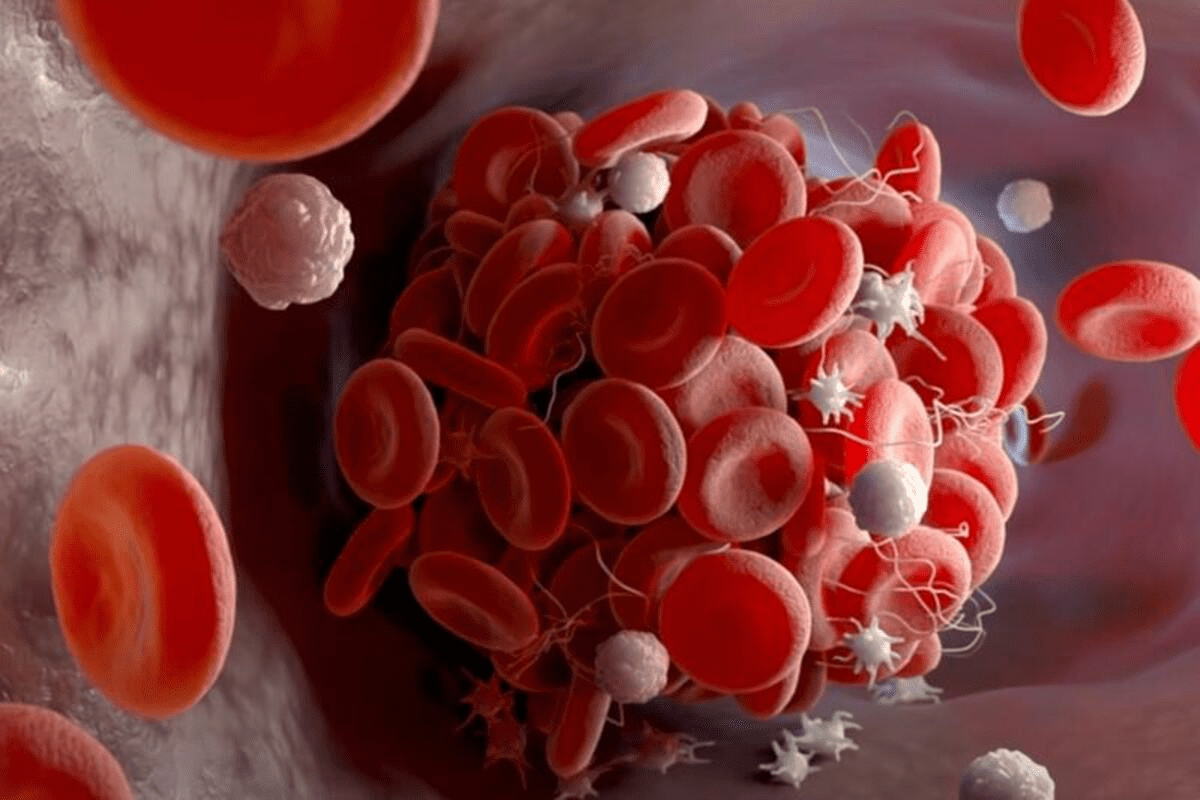
Complete blood counts (CBC) reveal the number and type of immune cells. Abnormalities in white blood cell counts are often the first sign of immune dysregulation.

Patch testing is used to diagnose contact dermatitis. Unlike prick testing, which looks for immediate reactions, patch testing looks for delayed reactions. Patches containing potential irritants are applied to the back.
These patches remain in place for 48 hours. The patient returns to the clinic to have them removed and the skin evaluated. A second reading is often done a few days later.
This helps identify triggers such as nickel, fragrances, and preservatives found in cosmetics and personal care products. It is crucial for patients with chronic, unexplained skin rashes.
For patients with respiratory symptoms, evaluating lung function is key. Spirometry measures how much air a person can inhale and exhale, and how fast. This helps diagnose asthma and assess its severity.
Fractional exhaled nitric oxide (FeNO) testing measures airway inflammation. High levels indicate allergic inflammation that typically responds well to steroids.
These tests are often repeated over time to monitor treatment effectiveness. They provide objective data to support the patient’s subjective feelings of breathlessness.
Send us all your questions or requests, and our expert team will assist you.
The definitive test for food allergy is the oral food challenge. This is performed under strict medical supervision. The patient gradually increases the amount of the suspected food.
This is done when skin or blood tests are inconclusive. It helps rule out allergies, allowing patients to reintroduce foods safely into their diet.
Because there is a risk of a severe reaction, this must be done in a facility equipped to handle anaphylaxis. It is the gold standard for confirming or clearing a food allergy diagnosis.
Modern diagnosis often involves analyzing DNA. Genetic testing can identify specific mutations responsible for primary immunodeficiencies or autoinflammatory syndromes.
This is particularly important for infants with severe infections. Early identification enables life-saving interventions such as bone marrow transplants.
Advanced molecular testing can also phenotype specific immune cells. This helps doctors understand exactly which part of the immune system is malfunctioning.
In certain areas, large specialized practices provide comprehensive care. For example, a patient might seek out the Northeast Allergy, Asthma, and Immunology Centers, known for their research and scope of services. These regional hubs often employ a multidisciplinary approach.
Groups like allergy, asthma, and immunology associates often have multiple locations, making care accessible while pooling resources for advanced testing. They serve as a bridge between community care and academic research.
These centers often have dedicated infusion suites for biologic therapies and specialized labs for detailed immune competence testing.
To determine if the immune system is working, doctors may test its “memory.” This involves checking vaccine titers. If a patient has received a tetanus shot but still lacks antibodies, it suggests a failure of the adaptive immune system.
Sometimes, a “test immunization” is given. The doctor administers a vaccine (such as the pneumonia vaccine) and checks blood work a few weeks later to see if the body mounted a proper immune response.
This functional testing goes beyond just counting cells; it proves whether those cells can actually do their job.
Diagnosing autoimmune diseases requires looking for autoantibodies—antibodies that attack the self. The Antinuclear Antibody (ANA) test is a standard screen. A positive result leads to more specific testing for lupus, Sjogren’s, or other conditions.
Rheumatoid factor and anti-CCP are checked for joint issues. Thyroid antibodies are measured for thyroid disease.
These tests must be interpreted carefully. Low levels of autoantibodies can be present in healthy people. Clinical correlation with symptoms is mandatory.
Traditional allergy tests use whole extracts (like an entire peanut). Component-resolved diagnostics analyze specific proteins within the allergen.
For example, it can tell whether a patient is allergic to a peanut protein associated with severe reactions, or to a protein associated with mild responses that might be tolerated.
This level of detail helps refine the risk assessment. It can prevent unnecessary dietary restrictions for patients who may tolerate certain forms of the allergen.
Diagnosis is rarely a solo endeavor. Allergy immunology associates often work with pulmonologists, dermatologists, and gastroenterologists.
For example, a patient with Eosinophilic Esophagitis needs both an allergist to manage the food triggers and a gastroenterologist to perform the biopsies.
This collaborative model ensures that all aspects of the immune-mediated disease are evaluated and treated. It provides a holistic view of the patient’s health.
Diagnosing children requires minimizing trauma. Skin tests are often preferred over blood draws as they are less invasive. When blood is needed, pediatric phlebotomy techniques are used.
Reference ranges for immune cells change with age. A normal white blood cell count for a newborn is different from that of a teenager. Specialists use age-appropriate data for interpretation.
Diagnosing asthma in young children who cannot perform spirometry relies heavily on history and trial of medication.
Skin prick test results are available immediately, typically within 20 minutes of the appointment, while blood test results usually take a few days to process in the lab.
No, you must stop antihistamines for 5 to 7 days before skin testing because they block the skin’s reaction, leading to false-negative results.
Genetic testing is not standard for common allergies, but it is crucial for diagnosing primary immunodeficiencies and certain rare autoinflammatory diseases.
A food challenge involves eating small amounts of a potential allergen under strict medical supervision to confirm or rule out a food allergy definitively.
Not necessarily; a positive blood test indicates sensitization (presence of antibodies), but if you can eat the food or breathe the allergen without symptoms, you are not clinically allergic.


Vitamin B12 is key for healthy red blood cells, nerve function, and DNA. Deficiencies in vitamin B12 can cause fatigue, weakness, and nerve issues. At

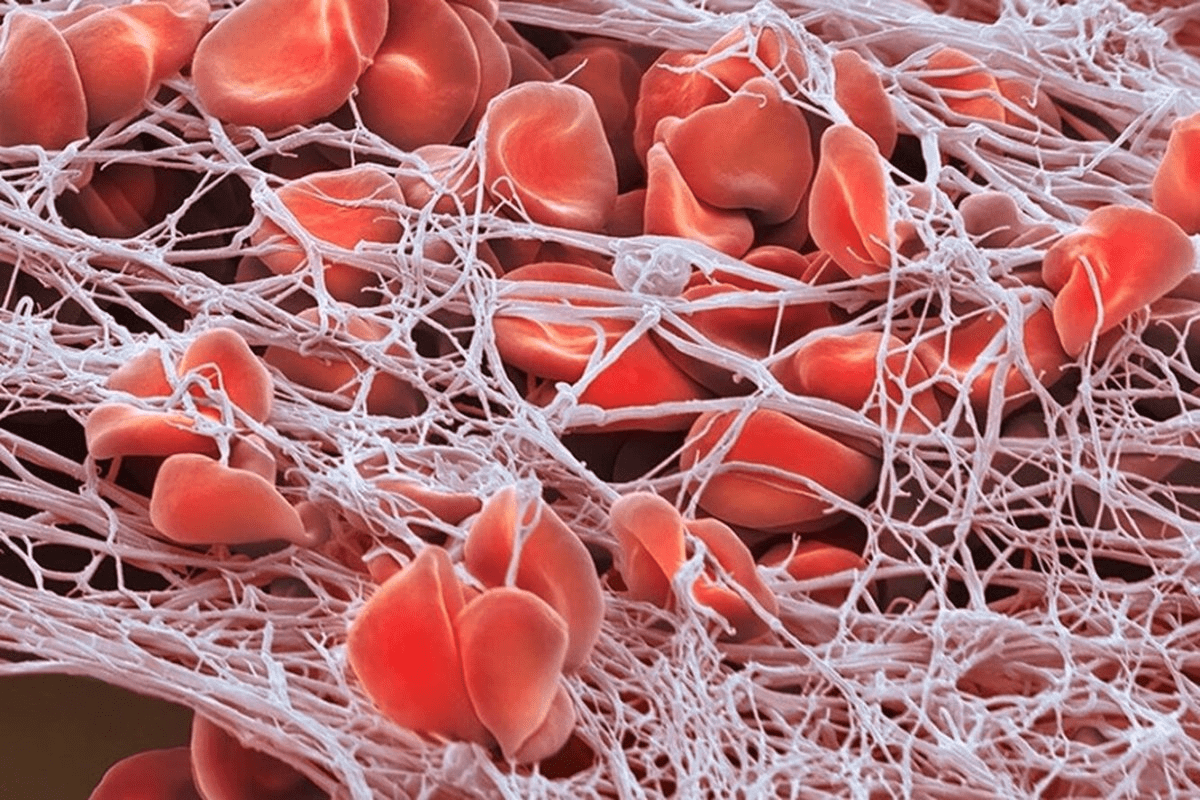
We look into the complex link between lupus anticoagulant and blood clotting issues. We dive deep into the details of antiphospholipid syndrome (APS). Lupus anticoagulant
Abnormal red cells can signal a health problem. It’s important to understand their meaning for proper diagnosis and treatment. Red cells carry oxygen in our
Did you know millions of people worldwide have hematological disorders that affect their blood and its parts? These issues can greatly change a person’s life,
Deficiency anemia treatment is a key topic in global health because nearly one-third of the world’s population has anemia. This condition happens when the body

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)