Infectious diseases specialists diagnose and treat infections from bacteria, viruses, fungi, and parasites, focusing on fevers, antibiotics, and vaccines.
Send us all your questions or requests, and our expert team will assist you.

HIV prevention now goes beyond just changing behavior and includes strong medical strategies. At Liv Hospital, prevention uses medicines to block the ways HIV spreads. This helps people take charge of their sexual health and protects them after accidental exposures. The approach includes Treatment as Prevention (TasP), Pre-exposure Prophylaxis (PrEP), Post-exposure Prophylaxis (PEP), and harm reduction.
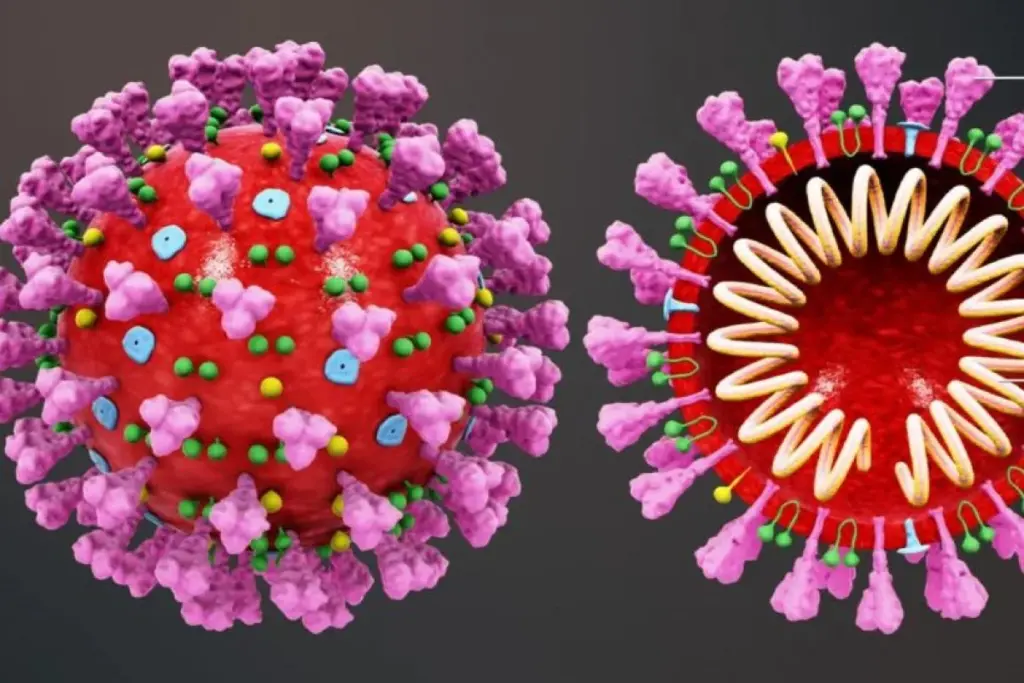
One of the biggest advances in HIV control is the proof that “Undetectable = Untransmittable” (U=U). This means that someone with HIV who takes their medicine and keeps their viral load undetectable for at least six months cannot pass the virus on through sex. Treatment as Prevention (TasP) turns people with HIV from possible sources of infection into part of the solution. When more people are diagnosed and treated, the overall amount of virus in the community drops, helping stop the spread. This idea also helps reduce stigma and encourages more people to get tested.

PrEP is a biomedical intervention for HIV-negative individuals who are at substantial risk of acquiring the infection. It involves taking a specific antiretroviral medication before potential exposure to the virus.

PEP is an emergency medical response for HIV-negative individuals who have had a potential high-risk exposure to HIV (e.g., condom break, sexual assault, needlestick injury).

Vertical transmission control is one of the greatest success stories in HIV prevention. It involves a cascade of interventions:
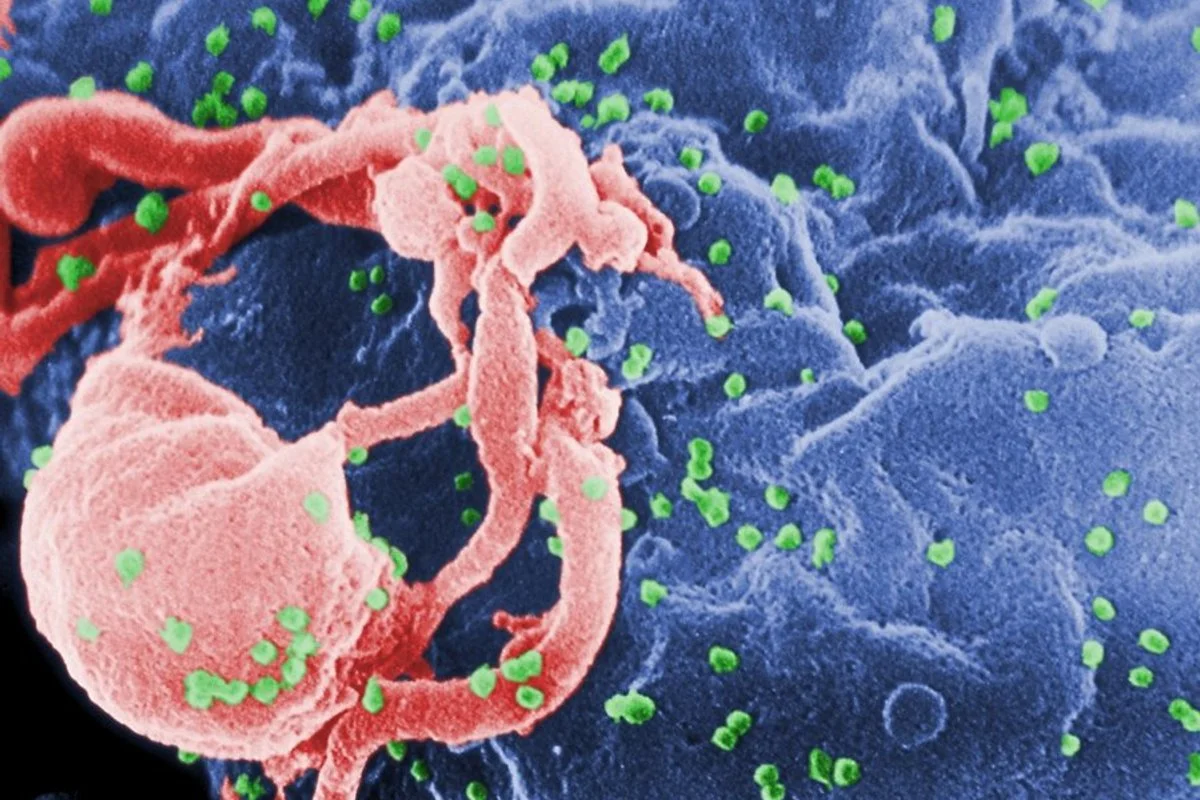
Prevention also addresses the route of transmission via injection drug use. Harm reduction strategies focus on minimizing the risks associated with drug use without necessarily requiring the cessation of use. This includes needle and syringe exchange programs to ensure access to sterile equipment and prevent the sharing of needles, which is a highly efficient mode of transmission.

While biomedical interventions are powerful, barrier methods (condoms) remain a cornerstone of prevention. They are the only method that protects against both HIV and other sexually transmitted infections (syphilis, gonorrhea, chlamydia). Comprehensive sexual health education promotes risk awareness, regular testing, and the negotiation of safer sex practices. The integration of barrier methods with biomedical tools like PrEP offers the highest level of protection.
Public health control relies on surveillance systems to track infection rates and molecular clusters. Partner notification services (contact tracing) are essential. When a person is diagnosed, public health officials or clinicians assist in notifying past partners that they may have been exposed, advising them to get tested and linking them to care or PrEP. This interrupts forward transmission networks.
Send us all your questions or requests, and our expert team will assist you.
PrEP (Pre-exposure Prophylaxis) is a preventive medication taken before exposure by people who are HIV-negative but at risk, acting like a daily shield against the virus. PEP (Post-exposure Prophylaxis) is an emergency medication taken after a potential exposure has occurred (like a condom breaking or a needlestick). PEP must be started within 72 hours, whereas PrEP is ongoing.
The scientific consensus for U=U (Undetectable = Untransmittable) applies specifically to sexual transmission. While an undetectable viral load significantly reduces the risk of transmission via breastfeeding or needle sharing, the risk is not scientifically defined as zero in the same absolute terms as sexual transmission. However, the risk is drastically lower than with a high viral load.
PrEP is highly effective, but its protection is strongly linked to adherence. For sexual protection, daily dosing provides the highest level of safety (about 99%). If doses are missed, the drug’s concentration in body tissues drops, and protection decreases. Taking it consistently ensures there is enough drug in the body to block the virus if exposure occurs.
PrEP protects specifically against HIV, but it offers no protection against other sexually transmitted infections (STIs) like gonorrhea, chlamydia, or syphilis, nor does it prevent pregnancy. Therefore, condoms are still recommended to provide comprehensive protection against the full range of STIs and for reproductive health control.
Nephrology focuses on the kidney’s role in the long-term regulation of
If you believe you have been exposed to HIV within the last 72 hours, you should go to an emergency room or a sexual health clinic immediately and ask for PEP (Post-exposure Prophylaxis). Time is critical; the sooner PEP is started, the better it works. You will be tested and, if appropriate, given a 28-day course of medication to prevent infection.
base (bicarbonate) and acid excretion. Pulmonology focuses on the lung’s role in the rapid regulation of carbon dioxide levels. Both are vital, but handle different parts of the Acid-Base control system.


Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)