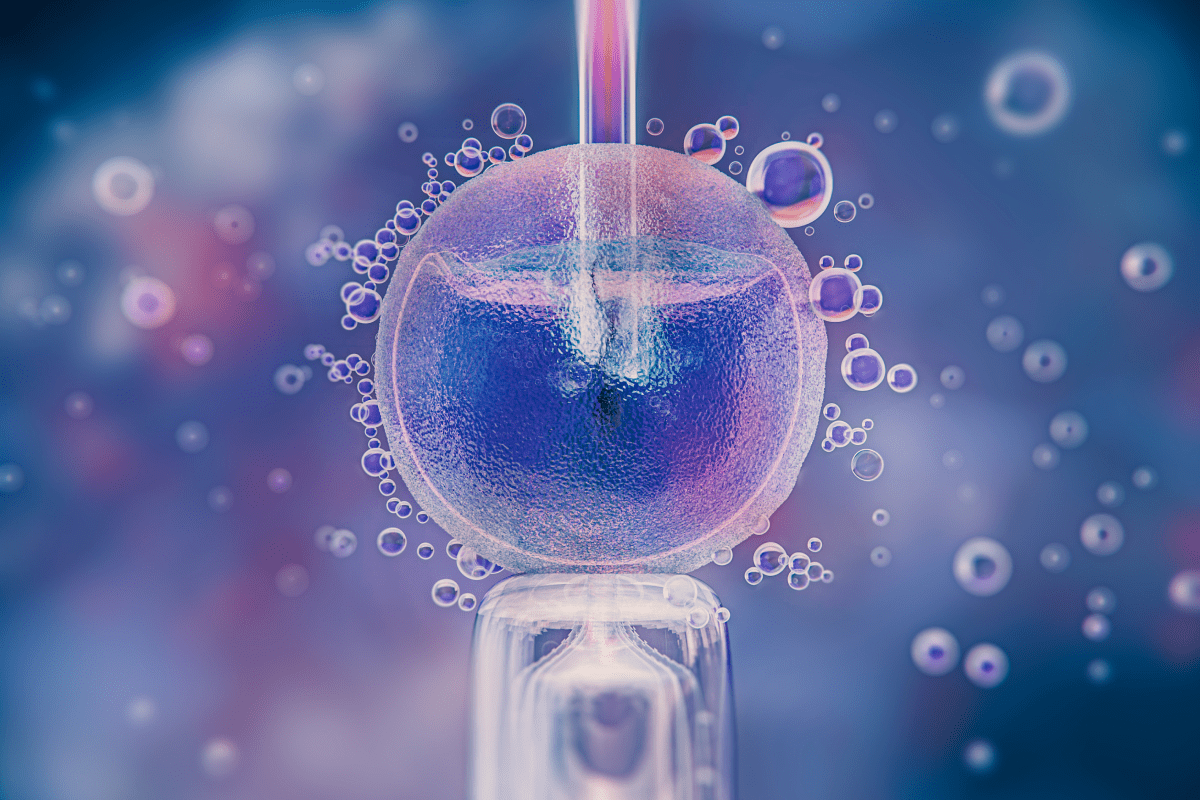
ICSI is a specialized fertilization technique where a single sperm is injected directly into an egg. It is a key procedure within Assisted reproductive technology ICSI.
Send us all your questions or requests, and our expert team will assist you.
Intracytoplasmic Sperm Injection (ICSI) is an advanced laboratory technique used as part of In Vitro Fertilization (IVF). Unlike conventional IVF, where thousands of sperm are placed around an egg to fertilize it naturally, ICSI manually injects a single sperm directly into the center (cytoplasm) of the egg. This technique dramatically increases the chances of fertilization when there is severe male factor infertility.
ICSI is one of the most powerful tools in Assisted reproductive technology ICSI. It bypasses many common barriers to fertilization, such as poor sperm motility or sperm that cannot penetrate the egg’s outer layer. The procedure is performed under a high-power microscope by a skilled embryologist at LIV Hospital.

Intracytoplasmic Sperm Injection (ICSI) is the procedure of injecting a single, carefully selected sperm into the cytoplasm (the inner substance) of an oocyte (egg) to achieve fertilization.
The term’s etymology precisely describes the action: Intra means ‘within,’ and cytoplasmic refers to the inner cellular fluid of the egg. The full term means “injection of sperm within the cytoplasm.” This technique provides absolute certainty that the sperm is placed where it needs to be to potentially fuse with the egg’s nucleus. ICSI revolutionized the treatment of severe male infertility when it was introduced in the early 1990s.

ICSI is a specific step performed during the larger IVF process. Understanding its unique role is important for patients considering IVF with ICSI.
ICSI is primarily utilized when infertility is caused by factors that prevent sperm from fertilizing the egg naturally, making it a powerful tool within Assisted reproductive technology ICSI.
The core of the ICSI procedure is cellular and laboratory-based, but it relies on the proper function of the reproductive organs and the controlling endocrine system.

ICSI is arguably one of the most significant breakthroughs in reproductive medicine since IVF itself. It has made fatherhood possible for virtually all men, regardless of the severity of their sperm count or quality issues, as long as viable sperm can be obtained. ICSI effectively eliminated severe male factor infertility as an untreatable cause of childlessness.
The success of IVF with ICSI is now routine, providing hope where previously there was none. It has also enabled the widespread use of Preimplantation Genetic Testing (PGT) by ensuring that only one sperm is involved in the fertilization, preventing contamination from other sperm that could interfere with genetic analysis.
The successful execution of the ICSI procedure relies on the highly specialized skills of a multidisciplinary team at LIV Hospital.

Send us all your questions or requests, and our expert team will assist you.
Reproductive Endocrinology is a medical subspecialty focused on the hormones and reproductive organs related to fertility. A specialist manages infertility and performs treatments like IVF and ICSI.
Fertility specialists treat conditions that affect a couple’s ability to conceive, including endometriosis, Polycystic Ovary Syndrome (PCOS), and male factor infertility. They also treat recurrent pregnancy loss.
The main types include In Vitro Fertilization (IVF), which is the cornerstone, as well as Intrauterine Insemination (IUI), and the specialized ICSI technique. These methods help sperm and egg meet and result in a pregnancy.
You should see a specialist if you are under 35 and have not conceived after one year of regular, unprotected intercourse, or if you are over 35 and have not conceived after six months. If you have known issues, you should see one immediately.
A fertility specialist focuses on helping you become pregnant, while an obstetrician focuses on caring for you during the pregnancy and delivering the baby. They work closely together as your care progresses.


Guide to the ideal location where in the uterus does the embryo implant (upper posterior wall). Knowing embryo implantation location is key for a healthy
Explaining the best location where do embryos implant in the uterus for successful pregnancy. Embryo implantation is a key step in human reproduction, starting a
The bloating after embryo transfer is filled with hope and worry. People watch their bodies for signs of a successful embryo implantation. Knowing what to

FET ultrasound is key in modern fertility treatments. It helps place embryos exactly in the uterus. This makes IVF treatments more successful for many people.
The Depo-Provera shot is a popular birth control option for many women. But, it’s important to know what happens when you stop using it. This
The Depo-Provera injection, also known as the Depo shot, is a top-notch birth control option. It has a success rate of over 99% in preventing

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)