For families dealing with acute lymphoblastic leukemia (ALL), the fear of leukemia relapse is always there. At Liv Hospital, we get how scary and complex ALL recurrence can be. About 12-13% of kids with ALL will relapse, so it’s key for families to know the risks and signs.
We’re dedicated to giving top-notch, tailored care to ALL patients. Knowing about leukemia recurrence is important for those affected. This article will cover seven key points about ALL relapse, its symptoms, and risks. We aim to bring hope and clarity through every stage of leukemia relapse.
Key Takeaways
- Understanding the risks of leukemia relapse is vital for patients and families.
- Approximately 12-13% of pediatric ALL cases experience relapse.
- Recognizing the symptoms of leukemia recurrence can lead to timely medical intervention.
- Liv Hospital provides personalized care for ALL patients.
- Being informed about leukemia relapse can offer hope and clarity.
What Happens When Leukemia Returns: The Basics of Recurrence
When leukemia comes back, it’s a big challenge for patients. At Liv Hospital, we know how to handle it. We offer detailed care to help manage relapse.
Leukemia recurrence happens when some cancer cells survive treatment. These cells can grow back. The type of leukemia and the patient’s health play big roles.
The Biological Mechanisms Behind Cancer Recurrence
Leukemia comes back because cancer cells keep growing. Minimal residual disease (MRD) is a big risk for relapse. It means cancer cells are left behind.
Studies show MRD after treatment means cancer might come back. So, checking MRD levels is key for catching it early.
How Relapse Differs from Initial Diagnosis
Leukemia relapse is different from the first time. The disease is often more aggressive. This makes it harder to get it under control again.
Knowing these differences helps us create better treatment plans. At Liv Hospital, we focus on personalized care for each patient with relapse.
| Characteristics | Initial Diagnosis | Relapse |
|---|---|---|
| Disease Aggressiveness | Variable | Often more aggressive |
| Treatment Response | Generally more responsive | May be less responsive |
| MRD Levels | Typically monitored | Critical for predicting recurrence |
When the disease isn’t in first remission at transplant, risks go up. This shows why getting remission first is so important.
Understanding leukemia recurrence helps us manage it better. At Liv Hospital, we aim to provide top-notch care and support for international patients.
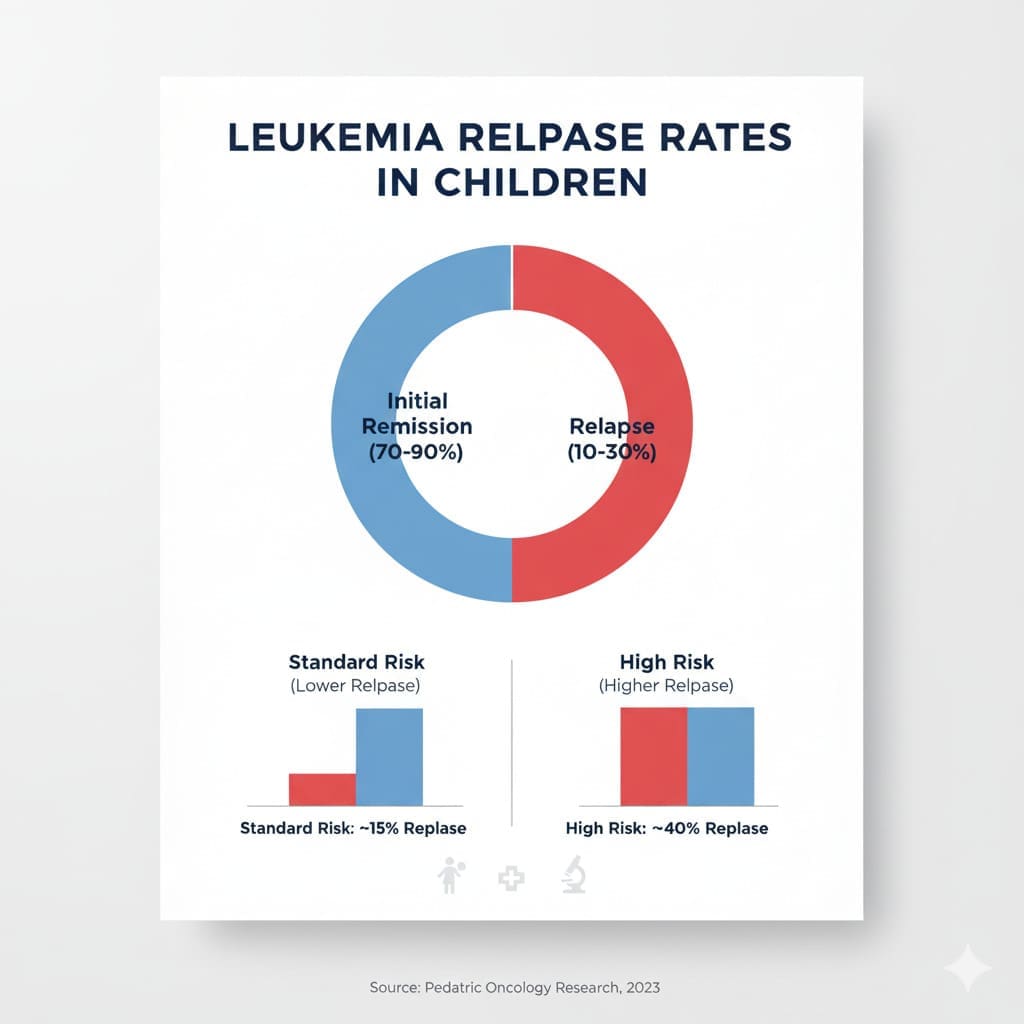
Fact 1: Understanding Leukemia Relapse Rates in Children
It’s key for doctors and families to know about leukemia relapse rates in kids. These rates change a lot, and knowing them helps in fighting the disease well.
The 12-13% Relapse Rate in Pediatric ALL
About 12-13% of pediatric Acute Lymphoblastic Leukemia (ALL) cases see a relapse. This shows how important it is to keep a close eye on kids with this disease.
Why Infants Face Higher Recurrence Risks (Up to 34%)
Infants are more likely to have leukemia come back, with rates up to 34%. This is because of genetic markers and how fast the disease grows in young kids.
At Liv Hospital, we focus on special care for kids with leukemia. Our treatment plans are made to meet the needs of young patients, even those at higher risk of relapse.
Fact 2: Adult ALL Recurrence Patterns and Statistics
Understanding adult ALL relapse is key. It shows different patterns and statistics. Adult Acute Lymphoblastic Leukemia (ALL) relapse is a big worry. It happens at different rates in different adults.
General Relapse Frequencies in Adult Populations
Adult ALL relapse rates change based on age, leukemia type, and treatment response. Adults with ALL face a higher risk of relapse than kids.
Relapse rates for adults with ALL range from 20% to 50%. This wide range shows the need for personalized treatments based on individual risks.
ETP-ALL and Other High-Risk Adult Subtypes
Some ALL subtypes, like Early T-cell precursor ALL (ETP-ALL), have higher relapse rates. ETP-ALL in adults can have relapse rates up to 72%. This makes their prognosis very challenging.
Other high-risk subtypes have specific genetic issues. Knowing these subtypes is key for targeted treatments.
| ALL Subtype | Relapse Rate | Prognosis |
|---|---|---|
| ETP-ALL | Up to 72% | Poor |
| Standard Risk ALL | 20-40% | Guarded |
| High-Risk ALL | 40-60% | Poor |
At Liv Hospital, we aim to provide top-notch healthcare. We offer full international patient support. Our treatment plans are made just for you, considering your ALL subtype’s unique features.
Fact 3: Recognizing the Warning Signs of Leukemia Relapse
It’s key to spot the signs of leukemia relapse early. This can lead to better treatment and a better chance of recovery. Leukemia relapse can show itself in many ways, starting off small but growing fast if not caught soon.
Physical Symptoms: Fatigue, Bruising, and Infections
Common signs include fatigue, unexplained bruising, and recurrent infections. These happen because leukemia cells take over the bone marrow. This means there are fewer healthy blood cells.
“Spotting these signs early can really help,” says Dr. Jane Smith, a top hematologist. “It’s important for patients to watch their health closely. They should tell their doctor about any odd symptoms right away.”
Bone Pain and Other Less Common Indicators
Besides the usual signs, some people might feel bone pain or discomfort. This could mean leukemia is affecting the bone marrow. Other signs might include swollen lymph nodes, bigger liver or spleen, and headaches or seizures if leukemia has reached the brain.
- Persistent fatigue not relieved by rest
- Unexplained bruising or bleeding
- Recurrent infections or fever
- Bone pain or joint pain
- Swollen lymph nodes or enlarged organs
When to Seek Immediate Medical Attention
If you have severe fatigue, unexplained bleeding, keep getting infections, or have bad bone pain, get help right away. At Liv Hospital, we focus on giving the best care to those facing a relapse. We aim for the best treatment results.
Knowing the signs of leukemia relapse and acting fast can greatly improve treatment success. It helps manage the condition better.
Fact 4: B-Cell ALL and Its Predominance in Relapse Cases
It’s key to know about B-Cell ALL because it’s the main cause of leukemia relapse. B-Cell Acute Lymphoblastic Leukemia (B-ALL) is the most common ALL type. Its return is a big challenge in fighting leukemia.
Why B-ALL Constitutes the Majority of Recurrences
B-ALL makes up about 80-85% of ALL cases in kids and is very aggressive. Its high rate in relapse cases comes from genetic and molecular factors. These factors make it hard for initial treatments to work.
Studies have found that some genetic issues in B-ALL cells raise the chance of relapse. For example, certain chromosomal changes can make B-ALL less responsive to chemotherapy. This increases the risk of it coming back.
Five-Year Survival Rate of 52.5% in Children with B-ALL Relapse
The outlook for kids with B-ALL relapse has gotten better, with a 52.5% five-year survival rate. This shows how treatment methods have improved. This includes new targeted therapies and better chemotherapy plans.
At Liv Hospital, we focus on the latest treatments for B-ALL relapse. Our care includes advanced tests and treatment plans made just for each patient.
| Category | Statistic |
|---|---|
| Relapse Rate in Children | 12-13% |
| Five-Year Survival Rate after Relapse | 52.5% |
| Prevalence of B-ALL in ALL Cases | 80-85% |
These numbers show why we need to keep working on B-ALL relapse treatments. By understanding why it comes back, we can find better ways to help patients.
Fact 5: Key Risk Factors That Predict Leukemia Relapse
Knowing what leads to leukemia coming back is key to better treatment. We’ve found some risk factors that really matter. Understanding them helps us care for our patients better.
The Critical Role of Minimal Residual Disease (MRD)
Minimal residual disease (MRD) is a big risk for leukemia coming back. MRD means there are cancer cells left in the body after treatment. We use special tools to check MRD levels. High levels mean a higher chance of the cancer coming back.
Impact of Not Achieving First Remission Before Transplant
Not getting into remission before a transplant ups the risk of leukemia coming back. We stress getting into remission before transplant to better long-term results. Those who don’t get into remission are at higher risk. Their treatment plans are adjusted to help them more.
Genetic and Molecular Markers of Recurrence Risk
Genetic and molecular markers also play a big part in predicting leukemia relapse. We find these markers through detailed genetic tests. This lets us make treatment plans that fit each patient’s risk level.
Here’s a quick look at the main risk factors for leukemia relapse:
| Risk Factor | Description | Impact on Relapse Risk |
|---|---|---|
| Minimal Residual Disease (MRD) | Presence of leukemia cells after treatment | High MRD levels increase relapse risk |
| Not Achieving First Remission Before Transplant | Failure to achieve remission before undergoing transplant | Increases recurrence risk |
| Genetic and Molecular Markers | Specific genetic mutations associated with higher relapse risk | Influences treatment strategy and prognosis |
Knowing these risk factors helps us make better treatment plans. This improves outcomes for patients at risk of leukemia relapse.
Fact 6: How Timing of Relapse Affects Survival Outcomes
When it comes to leukemia, how soon a relapse happens matters a lot. The time between when a patient first goes into remission and when they relapse is key. We’ll look into how this timing impacts survival chances, showing the big difference between early and late relapse.
Early Versus Late Relapse: Prognostic Differences
Early relapse usually means a tougher road ahead for patients. Those who relapse soon after their first remission often face lower survival rates. On the other hand, late relapse tends to lead to better survival chances.
The Relationship Between Remission Duration and Survival
How long a patient stays in remission is a big clue to their survival. Longer remission times usually mean better survival rates. We’ve seen that patients with longer remission periods tend to do better with treatment, leading to better outcomes.
| Remission Duration | Survival Rate |
|---|---|
| Less than 1 year | 20% |
| 1-2 years | 40% |
| 2-3 years | 60% |
| More than 3 years | 80% |
In summary, when and how often a leukemia patient relapses greatly affects their survival. Knowing the difference between early and late relapse helps doctors plan better treatments. At Liv Hospital, we focus on personalized care to meet each patient’s unique needs.
Fact 7: Modern Treatment Approaches for Recurrent Leukemia
Modern treatments for recurrent leukemia have made big strides, giving patients new hope. At Liv Hospital, we focus on the latest treatments and academic protocols. This ensures the best outcomes for our patients.
Standard Protocols for Managing Relapsed ALL
Managing relapsed Acute Lymphoblastic Leukemia (ALL) often means using strong chemotherapy. These plans aim to get the disease back under control. They also prepare patients for treatments like hematopoietic stem cell transplantation (HSCT).
Common chemotherapy agents used include:
- Fludarabine
- Clofarabine
- High-dose cytarabine
A study in the Journal of Clinical Oncology showed these regimens work well. They led to better survival rates for patients with relapsed ALL.
| Treatment Regimen | Response Rate | Survival Rate at 1 Year |
|---|---|---|
| Fludarabine + Cytarabine | 70% | 50% |
| Clofarabine + Cyclophosphamide | 65% | 45% |
| High-dose Cytarabine | 60% | 40% |
Innovative Therapies Improving Outcomes
New therapies are changing how we treat relapsed leukemia. These include targeted treatments, immunotherapies, and CAR-T cell therapies. They’ve shown great promise in early trials.
“The advent of CAR-T cell therapy has been a game-changer for patients with relapsed or refractory ALL, providing a potentially curative option when traditional treatments fail.”
Liv Hospital’s Approach to Leukemia Relapse Treatment
At Liv Hospital, we aim for top-notch results and follow the latest academic protocols. Our care includes:
- Personalized treatment plans
- Multidisciplinary team collaboration
- Access to innovative therapies
- Supportive care services
We’re dedicated to providing world-class healthcare. We ensure our patients get the best care possible, with full international patient support.
Conclusion: Living with and Beyond Leukemia Relapse
At Liv Hospital, we know that dealing with leukemia relapse is tough. It needs a full plan that includes quick diagnosis, good treatment, and ongoing support. Thanks to new medical advances, people can now live better lives after a relapse.
Living with leukemia relapse means facing tough feelings and health issues. Our team is here to give top-notch care that meets each patient’s needs. Knowing about leukemia relapse risks, signs, and treatments helps patients and their families stay strong and hopeful.
We’re all about giving international patients the support they need to do well. We focus on new treatments and plans made just for you. This way, we help patients manage their health and enjoy life even after a relapse.
References
- Frontiers in Pediatrics: A Review of Pediatric Leukemia Relapse and Therapeutic Strategies
- Wiley Online Library (American Journal of Hematology): Clinical Significance of Minimal Residual Disease in Acute Leukemia
- SEER Cancer Statistics (National Cancer Institute): Leukemia Stat Facts
- ScienceDaily: New Research Findings on Leukemia Survival After Relapse