Last Updated on September 20, 2025 by Saadet Demir
Nearly 30% of patients face complications after a bone marrow transplant. This shows how important post-transplant care is. Knowing the medicines used after this procedure is key for recovery.
Patients needing transplantation get a mix of drugs to stop rejection and handle side effects. The medicines and how much depend on the patient’s needs and treatment details.
Good post-transplant care means finding the right mix of medicines for a smooth recovery. By knowing how these medicines work, patients can better handle their treatment and get better results.
Key Takeaways
- Medications play a key role in post-transplant care.
- Patients need a mix of drugs to stop rejection.
- The medicines and how much depends on the patient’s needs.
- Good post-transplant care means finding the right mix of medicines.
- Understanding the medicines can help patients get better.
Understanding Stem Cell Transplantation
Stem cell transplantation is a complex medical procedure. It has changed how we treat life-threatening diseases. This method uses stem cells to help the body make healthy cells again. It gives hope to patients with certain medical conditions.
Definition and Purpose of Stem Cell Transplants
A stem cell transplant, also known as a bone marrow transplant, replaces damaged or diseased stem cells with healthy ones. The main goal is to re-establish the body’s ability to produce healthy blood cells. This is important for patients with diseases like cancer and autoimmune disorders.
The transplant starts with preparing the patient. This includes chemotherapy and/or radiation therapy. These steps are key to getting rid of diseased cells and making room for new stem cells.
Different Types of Stem Cell Transplants
There are two main types of stem cell transplants: autologous and allogeneic. Knowing the difference is important for patients to make the right choice for their treatment.
- Autologous Stem Cell Transplant: This uses the patient’s own stem cells. They are harvested, stored, and then re-infused after treatment. It’s often used for cancers like multiple myeloma and lymphoma.
- Allogeneic Stem Cell Transplant: This uses stem cells from a donor. The donor can be a family member or someone else. Allogeneic transplants are used for blood disorders and some leukemia types.
Each transplant type has its own risks and considerations. Allogeneic transplants can lead to graft-versus-host disease(GVHD).
The Stem Cell Transplant Procedure Overview
A stem cell transplant is a big medical step. It replaces a patient’s sick or damaged stem cells with healthy ones. These can come from the patient themselves or a donor.
Pre-Transplant Preparation
Before a stem cell transplant, patients go through a lot. This includes:
- Medical checks to see if they’re healthy enough for the transplant.
- Chemotherapy and/or radiation to kill off sick cells and weaken the immune system.
- Finding a good donor, if the transplant is from someone else.
Pre-transplant conditioning is key. It gets rid of cancer cells and makes room for new stem cells. The exact treatment depends on the transplant type and the patient’s health.
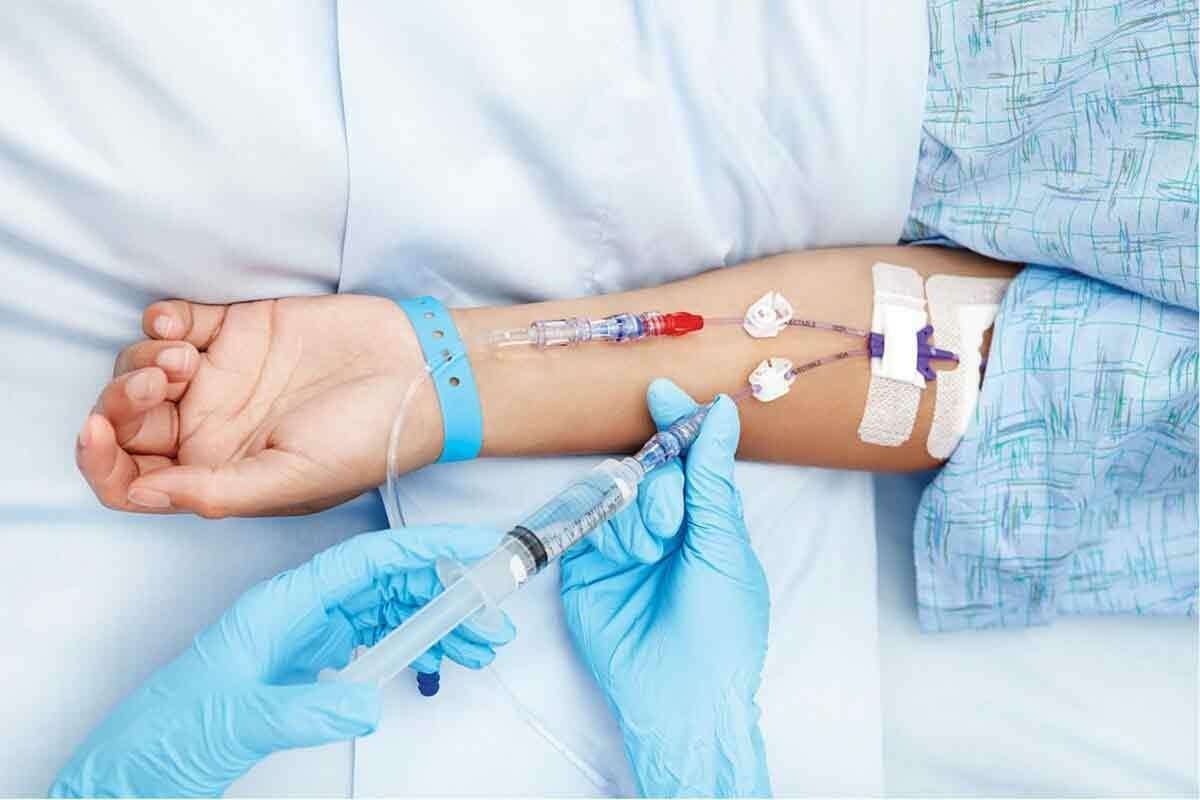
The Transplantation Process
The transplant itself is fast, taking just a few hours. But getting ready and recovering can take weeks or even months.
The actual transplant is quick. But the whole journey, from start to finish, is longer.
Immediate Post-Transplant Care
After the transplant, patients are watched closely for problems. This includes graft-versus-host disease (GVHD) in transplants from someone else. GVHD happens when the donor’s immune cells attack the patient’s body.
| Complication | Description | Management |
| Graft-versus-Host Disease(GVHD) | Immune reaction where donor cells attack recipient tissues. | Immunosuppressive medications, corticosteroids. |
| Infections | Patients are at risk due to suppressed immune systems. | Prophylactic antibiotics, antivirals, and antifungals. |
| Organ Dysfunction | Potential toxicity to organs like the liver and kidneys. | Monitoring organ function, supportive care. |
Patients often stay isolated to avoid infections. They get medicines to help the new stem cells and deal with side effects. The first days after the transplant are very important. Good care can make a big difference in how well the transplant works.
Why Medications Are Essential After Transplant
Medications are key after a stem cell transplant. They help the transplant work and aid in recovery.
Preventing Complications
Medications are vital to avoid problems. Immunosuppressive drugs stop the body from rejecting the new cells. OncoLink says, “Immunosuppressive therapy is a critical part of post-transplant care.”
- Preventing graft-versus-host disease (GVHD)
- Reducing the risk of infections
- Managing possible organ damage
Supporting New Cell Growth
Medications also help new cells grow. Growth factors boost blood cell production. This helps replace lost cells after the transplant.
Some key benefits of growth factors are:
- Helping white blood cells recover
- Lowering infection risk
- Supporting bone marrow recovery
Managing Side Effects
Managing side effects is also important. Medications can ease symptoms like bone pain after stem cell transplant and chemotherapy and mouth sores. This makes recovery better.
“Proper management of side effects is key for patients to stick with their treatment plans.” – Expert in Oncology
Understanding the role of medications after a transplant helps patients recover better. Following the medication plan is essential. It prevents problems, supports cell growth, and manages side effects.
Anti-Rejection Medications
Anti-rejection medications are key in post-transplant care. They help the body accept new stem cells. These drugs stop the immune system from rejecting the transplanted cells.
Calcineurin Inhibitors
Calcineurin inhibitors are important for stem cell transplants. Cyclosporine and Tacrolimus are common types. They block calcineurin, a protein that activates T-cells.
“The introduction of calcineurin inhibitors has revolutionized the field of organ and stem cell transplantation,” experts say.
mTOR Inhibitors
mTOR inhibitors, like Sirolimus, prevent rejection. They block the mammalian target of rapamycin (mTOR). This protein is involved in cell growth and survival.
mTOR inhibitors are a good alternative to calcineurin inhibitors. They may reduce side effects from long-term use.
Monitoring and Adjusting Anti-Rejection Medications
It’s important to check the levels of these medications in the blood. Regular blood tests help doctors adjust the dosage. This ensures the medications work well and don’t cause harm.
Adjusting these medications is a careful process. Too little can cause rejection, while too much can lead to infections and other problems.
A leading transplant specialist says, “The key to successful transplant management lies in the careful adjustment of immunosuppressive medications.”
Immunosuppressive Medications
Immunosuppressive drugs help prevent the body from rejecting transplanted cells. They keep the immune system from attacking the new cells.
Corticosteroids
Corticosteroids, like prednisone, are key in fighting off immune reactions. They are used to manage GVHD and stop graft rejection.
Key benefits of corticosteroids include:
- Rapid reduction of inflammation
- Effective in treating acute GVHD
- Can be used in combination with other immunosuppressive agents
Mycophenolate Mofetil (CellCept)
Mycophenolate mofetil stops T and B lymphocytes from growing. It’s often paired with other drugs to prevent GVHD and graft rejection.
Advantages of mycophenolate mofetil:
- Effective in reducing the incidence of GVHD
- Can be used long-term with careful monitoring
- Available in oral and intravenous formulations
Methotrexate
Methotrexate is used to stop GVHD. It blocks dihydrofolate reductase, needed for DNA and cell growth.
| Immunosuppressive Agent | Mechanism of Action | Common Use |
| Corticosteroids | Anti-inflammatory and immunosuppressive | GVHD, graft rejection |
| Mycophenolate Mofetil | Inhibits T and B lymphocyte proliferation | GVHD prevention, graft rejection |
| Methotrexate | Inhibits dihydrofolate reductase | GVHD prevention |
Newer Immunosuppressive Agents
New research aims to create better immunosuppressive drugs. These drugs target specific immune pathways.
The goal is to make treatments safer and more effective. This could reduce side effects like infections and organ damage.
Medications for Graft-Versus-Host Disease (GVHD)
Graft-versus-host disease (GVHD) is a serious issue after stem cell transplants. It needs careful treatment with different medicines. GVHD happens when the donor’s immune cells see the host as foreign and attack.
First-Line Treatments
The first step in treating GVHD is using medicines to calm down the immune system. Corticosteroids, like prednisone, are often the first choice. They are very good at reducing inflammation and can work well if started early.
Other medicines, like calcineurin inhibitors (cyclosporine and tacrolimus), are also used. They stop T-cells from getting too active, which helps prevent GVHD.
Second-Line Treatments
If first-line treatments don’t work or cause too many side effects, second-line options are considered. Mycophenolate mofetil (CellCept) is sometimes used. It stops T and B lymphocytes from growing, which helps reduce the immune response.
Other second-line treatments include sirolimus and rituximab. The right second-line treatment depends on how severe GVHD is, the patient’s health, and what first-line treatments were used.
Emerging Therapies for GVHD
New treatments for GVHD are being researched. Extracorporeal photopheresis (ECP) is one promising method. It removes white blood cells, treats them, and then puts them back in the body. ECP is used for GVHD that doesn’t respond to other treatments.
Other new treatments include mesenchymal stem cells, which can help control GVHD. Also, scientists are looking into targeted therapies that target specific parts of the GVHD process.
Antimicrobial Medications
Antimicrobial medications are key in fighting infections after stem cell transplants. They are very important because the patient’s immune system is weak. This makes them more likely to get sick.
Antibacterial Agents
Antibacterial agents help stop and treat bacterial infections. Fluoroquinolones and beta-lactam antibiotics are common ones. The right antibiotic depends on the infection and the patient’s health.
Antiviral Medications
Antiviral medications are vital for viral infections. Acyclovir is often used to stop herpes simplex virus from coming back. Valganciclovir helps prevent cytomegalovirus (CMV) infections.
Antifungal Treatments
Antifungal treatments are needed to stop and treat fungal infections. These infections can be very dangerous. Fluconazole and voriconazole are used to fight these infections.
Prophylactic vs. Therapeutic Approaches
Antimicrobial medications can be used to prevent or treat infections. The choice depends on the patient’s risk and the type of infection they might face.
| Type of Medication | Examples | Use |
| Antibacterial | Fluoroquinolones, Beta-lactam antibiotics | Prevent and treat bacterial infections |
| Antiviral | Acyclovir, Valganciclovir | Prevent and treat viral infections |
| Antifungal | Fluconazole, Voriconazole | Prevent and treat fungal infections |
Growth Factors and Blood Cell Stimulants
Growth factors and blood cell stimulants are key in post-transplant care. They help the body recover after a stem cell transplant. These medicines support the growth of blood cells.
Granulocyte Colony-Stimulating Factors (G-CSF)
G-CSF boosts the bone marrow to make granulocytes, a type of white blood cell. Filgrastim and Lenograstim are G-CSF types. They help fight infections after stem cell transplants.
Erythropoiesis-Stimulating Agents
ESAs help make red blood cells. Epoetin alfa and Darbepoetin alfa are ESAs. They reduce the need for blood transfusions in patients with anemia.
Thrombopoietin Receptor Agonists
These drugs boost platelet production. Romiplostim and Elthrombopag are used for low platelet count. They help prevent bleeding.
Bone Marrow Stimulant Drugs
Bone marrow stimulant drugs aid in bone marrow recovery after a transplant. They help make white blood cells, red blood cells, and platelets.
Here’s a quick look at the growth factors and blood cell stimulants we’ve talked about:
| Medication Type | Examples | Function |
| G-CSF | Filgrastim, Lenograstim | Stimulate production of granulocytes (white blood cells) |
| Erythropoiesis-Stimulating Agents | Epoetin alfa, Darbepoetin alfa | Stimulate production of red blood cells |
| Thrombopoietin Receptor Agonists | Romiplostim, Elthrombopag | Stimulate production of platelets |
Pain Management Medications
Managing pain is key for those who have had a stem cell transplant. It helps reduce discomfort and speeds up recovery. It also makes life better during the healing time after the transplant.
Managing Bone Pain After Transplant
Bone pain after a stem cell transplant can be treated with certain medicines. Granulocyte-Colony Stimulating Factor (G-CSF) injections can sometimes cause pain. Doctors often suggest using acetaminophen or ibuprofen to ease this pain.
Medications for Mouth Sores and Mucositis
Mouth sores and mucositis are common after stem cell transplants. They cause a lot of pain. Topical anesthetics like lidocaine can help numb the area, giving temporary relief. Gelclair is also used to help heal mouth sores.
Neuropathic Pain Treatments
Neuropathic pain, caused by nerve damage, is hard to manage. Doctors might prescribe gabapentin or pregabalin to help. Sometimes, tricyclic antidepressants are used for their pain-relieving effects.
It’s important for patients to work with their healthcare team to find the best pain management plan. Everyone reacts differently to pain medicines.
Oncolink Stem Cell Transplant Resources and Medication Guides
Understanding stem cell transplant medications is easier with OncoLink’s help. OncoLink offers detailed information for those going through stem cell transplants. They provide tools and guides for managing medications and overall care.
Medication Tracking Tools
OncoLink has medication tracking tools for patients. These tools help keep track of medications, dosages, and schedules. They are very useful for managing the complex medication plans after a stem cell transplant.
Educational Materials for Patients
OncoLink’s educational materials are key. They teach patients about their treatment. This includes the purpose of medications, side effects, and how to manage their care.
Support Resources for Caregivers
Caregivers are essential in stem cell transplant care. OncoLink has support resources for them. These resources give caregivers the information and guidance they need to support their loved ones.
Oncolink’s Expert Guidance on Transplant Medications
OncoLink’s team of experts offers guidance on transplant medications. They share the latest treatments and management strategies. This expert advice is valuable for patients and healthcare providers aiming to improve care and outcomes.
With OncoLink’s resources, patients and caregivers can better handle stem cell transplant care. They become well-informed and supported on their journey.
The First 30 Days After Stem Cell Transplant: Medication Timeline
After a stem cell transplant, a special medication plan is key. It helps the new immune system grow and prevents rejection. This time is vital for the transplant’s success. Medications help manage side effects, prevent problems, and help the bone marrow and immune system recover.
Immediate Post-Transplant Medications
Right after the transplant, patients stay in the hospital closely watched. They get important medicines to stop GVHD, manage pain, and fight off infections. These include:
- Immunosuppressants to prevent GVHD
- Antibiotics and antivirals to prevent infections
- Pain management medications to control discomfort
Week 1-2 Medication Adjustments
As recovery starts, the medicine plan changes. This is based on how the patient is doing and any side effects. For example, the dose of medicines to stop GVHD might change based on the patient’s blood counts.
Weeks 3-4 Medication Changes
By weeks 3-4, many patients go home but need careful medicine management. The focus is on helping the bone marrow recover and managing side effects. Growth factors might be used to help make more blood cells.
| Medication Type | Purpose | Timeline |
| Immunosuppressants | Prevent GVHD | Immediate post-transplant to several months later |
| Antibiotics/Antivirals | Prevent infections | Immediate post-transplant to until immune recovery |
| Growth Factors | Stimulate blood cell production | Variable, based on blood counts |
Transitioning to Outpatient Medication Management
When patients go home, they and their caregivers learn about managing medicines. They need to know about side effects and when to get help. This teamwork between the patient, caregivers, and healthcare team helps with a smooth recovery.
Managing medicines well in the first 30 days after a stem cell transplant is key. By knowing the medicine plan and working with their healthcare team, patients can get through this tough time and start recovering.
Managing Medications at Home
After a stem cell transplant, managing medications at home is key for a smooth recovery. It’s important for patients to understand how to manage their medications well.
Creating a Medication Schedule
Creating a medication schedule is a big part of managing medications at home. OncoLink says a schedule helps organize the many drugs patients need after a transplant. Patients should work closely with their healthcare team to make a schedule that fits their life and ensures they take their meds on time.
Storage and Handling Requirements
Storing and handling medications properly is vital. Patients need to know how to store each medication, like if it needs to be refrigerated or kept away from light. It’s also important to keep medications safe from children and pets.
Medication Interactions to Watch For
After a stem cell transplant, patients often take many medications. This can lead to drug interactions. It’s important for patients to tell their healthcare team about all medications they’re taking, including over-the-counter drugs and supplements. This helps avoid harmful interactions.
What Not to Do After Stem Cell Treatment
There are things patients should avoid after stem cell treatment. This includes avoiding foods that could interact with their medications or increase infection risk. Patients should also avoid close contact with sick people and activities that could cause injury or infection.
By following these guidelines and staying informed, patients can manage their medications at home well. This supports their recovery after a stem cell transplant.
Financial Considerations for Transplant Medications
Planning for transplant medication costs is key. These drugs can be very expensive. It’s important for patients and their families to understand the financial side.
Insurance Coverage for Transplant Medications
Insurance is a big help in covering transplant medication costs. Most plans help with the costs of drugs needed after a transplant. But, how much help varies a lot.
Key factors to consider when reviewing insurance coverage include:
- The specific medications covered under the plan
- Any out-of-pocket costs, such as deductibles and copays
- Restrictions or limitations on certain medications
- Coverage for any additional services or supplies needed
A financial expert notes,
“Knowing what your insurance covers is key to handling transplant medication costs. Patients should check their policies closely and ask questions if they’re not sure.”
Patient Assistance Programs
For those struggling financially, patient assistance programs (PAPs) can be a big help. These programs, from drug companies, non-profits, and government, can lower or wipe out medication costs.
Eligibility criteria for PAPs typically include:
- Income level
- Insurance status
- Medical diagnosis and treatment plan
Patients should look into these programs to see if they qualify for help.
Managing Long-term Medication Costs
Managing transplant medication costs over time needs careful planning. Ways to cut costs include:
- Following the doctor’s advice to avoid extra costs from complications or hospital stays
- Keeping an eye on and changing insurance as needed
- Looking into patient assistance programs and other financial help
- Talking to doctors about cheaper options
By being proactive, patients can handle the financial hurdles of transplant care better.
Building Your Immune System After Transplant
Rebuilding your immune system after a stem cell transplant needs both medical care and lifestyle changes. OncoLink says it’s key to guide patients on how to recover their immune system. This process is complex and needs careful management to avoid infections and keep you healthy.
Vaccination Schedule Post-Transplant
Following a vaccination schedule after transplant is very important. Vaccines protect against infections when your immune system is weak. Live vaccines are usually avoided until your immune system is strong enough. But, inactivated vaccines can be given earlier.
- Influenza vaccine: Recommended annually
- Pneumococcal vaccine: Given to protect against pneumococcal disease
- Tdap vaccine: Protects against tetanus, diphtheria, and pertussis
It’s vital to stick to the vaccination schedule your healthcare provider recommends. This schedule can change based on your transplant type and health.
Immune-Boosting Strategies
There are also immune-boosting strategies to help rebuild your immune system. These include:
- Maintaining good hygiene practices, such as frequent handwashing
- Avoiding close contact with individuals who are sick
- Staying physically active, as recommended by your healthcare provider
These steps can lower the risk of infections and help your immune system recover.
Nutritional Support for Immune Function
Nutrition is key for immune function. Eating a balanced diet with vitamins, minerals, and proteins can boost your immune system. Foods that are good for you include:
- Fruits and vegetables high in antioxidants
- Lean proteins such as chicken, fish, and legumes
- Whole grains like brown rice, quinoa, and whole-wheat bread
Drinking plenty of water is also important to stay hydrated.
Lifestyle Factors Affecting Immune Recovery
Lifestyle choices can greatly affect immune recovery. Quitting smoking is very important because smoking weakens the immune system. Also, managing stress through meditation, yoga, or deep breathing can help your immune system recover.
“A healthy lifestyle, including a balanced diet and regular exercise, is essential for immune system recoverypost-transplant.”
” OncoLink Expert Guidance
By combining medical treatments with lifestyle changes, patients can improve their immune system recovery and overall health.
Potential Medication Side Effects and Management
After a stem cell transplant, recovery is not just about getting better. It’s also about dealing with medication side effects. Knowing about these side effects and how to handle them is key to success.
Common Side Effects of Transplant Medications
Medications for transplants are vital but can cause side effects. These include nausea, fatigue, and a higher risk of infections. OncoLink says the severity and presence of these side effects vary among patients.
Managing these side effects requires a few steps. This includes adjusting medication doses, using other drugs to counteract side effects, and making lifestyle changes.
When to Contact Your Healthcare Team
It’s important for patients to know when to ask for help from their healthcare team. “If you experience severe symptoms such as difficulty breathing, chest pain, or severe pain, seek immediate medical attention,” doctors advise. Regular visits to the healthcare team can also help catch and manage side effects early.
Strategies to Minimize Side Effects
There are ways to reduce the side effects of transplant medications. These include:
- Following the medication schedule exactly
- Keeping a healthy lifestyle with a balanced diet and exercise
- Drinking plenty of water and managing stress
- Regularly checking in with the healthcare team about side effects
A healthcare professional notes,
“Proactive management of side effects not only improves the quality of life but also enhances the effectiveness of the treatment.”
Long-term Health Monitoring
Long-term health monitoring is vital after a transplant. This includes regular check-ups, watching for late effects of the transplant and its medications, and adjusting treatment plans as needed.
By understanding transplant medication side effects and working with their healthcare team, patients can manage their recovery better. This improves their long-term health outcomes.
Conclusion: The Importance of Medication Adherence After Stem Cell Transplant
Medication adherence is key to a good recovery after a stem cell transplant. It’s important to take all medicines as directed to avoid problems and help new cells grow. This also helps manage side effects.
Guides from Oncolink stem cell transplant offer helpful tips on managing medicines. They help patients understand their treatment plans better. This way, patients can improve their recovery.
It’s critical to follow the medication plan given by doctors. Patients should talk to their healthcare team about their medicines. This helps reduce risks and makes recovery smoother.
FAQ
Why is medication adherence important after a stem cell transplant?
Adhering to medication is vital for a successful recovery. It prevents complications, manages side effects, and supports the new immune system.
What are the possible side effects of transplant medications?
Common side effects include various symptoms. It’s important to know when to contact your healthcare team and how to minimize side effects.
How can I rebuild my immune system after a stem cell transplant?
Following a vaccination schedule and using immune-boosting strategies are important. Nutritional support and a healthy lifestyle also help rebuild the immune system.
What are the financial considerations for transplant medications?
Insurance coverage, patient assistance programs, and managing long-term costs are important financial considerations for transplant medications.
How do I manage medications at home after a stem cell transplant?
Creating a medication schedule and storing medications properly is key. Being aware of interactions helps manage medications at home.
What resources are available for stem cell transplant patients?
OncoLink offers resources like medication guides and educational materials. They also provide support for caregivers to help manage care.
How are pain management medications used in stem cell transplant patients?
Pain management medications help manage bone pain, mouth sores, and neuropathic pain from the transplant.
How are growth factors and blood cell stimulants used in stem cell transplant patients?
Growth factors and blood cell stimulants, like G-CSF, support blood cell production. They reduce the risk of infection and anemia.
What antimicrobial medications are used post-transplant?
Antimicrobial medications, including antibacterial, antiviral, and antifungal treatments, prevent and treat infections in transplant patients.
What medications are used to treat GVHD?
First-line treatments for GVHD include corticosteroids. Second-line treatments may involve other immunosuppressive agents. New therapies are also being explored.
How are immunosuppressive medications used in stem cell transplant patients?
Immunosuppressive medications, like corticosteroids, are used to suppress the immune system. They prevent graft-versus-host disease (GVHD).
What are anti-rejection medications used for?
Anti-rejection medications stop the immune system from rejecting the transplanted stem cells. They include calcineurin inhibitors and mTOR inhibitors.
Why are medications essential after a stem cell transplant?
Medications are key after a transplant. They prevent complications, support new cell growth, and manage side effects.
What are the different types of stem cell transplants?
There are two main types. Autologous uses the patient’s own stem cells. Allogeneic uses stem cells from a donor.
What is a stem cell transplant?
A stem cell transplant replaces damaged or diseased stem cells with healthy ones. It treats various cancers and diseases.