Learn how anemia in chronic kidney disease is diagnosed. Discover the tests, evaluation methods, and screening process.
Send us all your questions or requests, and our expert team will assist you.
The diagnostic journey for kidney anemia begins with a standard test called the Complete Blood Count (CBC). This test provides a comprehensive inventory of the blood’s cellular components. The primary value monitored is hemoglobin, which measures the protein in red blood cells that carries oxygen.
A diagnosis of anemia is typically made when hemoglobin levels fall below 12.0 g/dL for women and 13.0 g/dL for men. The CBC also measures hematocrit, the percentage of blood volume composed of red blood cells. These two values provide the baseline for diagnosis.
The CBC also provides indices that describe the size and shape of the red blood cells. The Mean Corpuscular Volume (MCV) indicates whether cells are too small (microcytic), suggesting iron deficiency, or too large (macrocytic), suggesting B12/folate deficiency. In kidney anemia, cells are often normal in size (normocytic).
This differentiation is crucial. It helps the medical team determine whether the anemia is solely due to kidney failure or whether additional nutritional factors are involved. It is the first step in unraveling the specific cause of the patient’s low blood count.
The reticulocyte count is a measure of young, immature red blood cells released by the bone marrow. This test evaluates the bone marrow’s response to the anemia. In a healthy person, if hemoglobin drops, the reticulocyte count should rise as the marrow works harder to replace cells.
In kidney anemia, the reticulocyte count is typically inappropriately low or normal. This indicates that the bone marrow is not responding to the anemia, confirming a production problem due to a lack of erythropoietin signal.
If the reticulocyte count is high, it suggests that the marrow is working, but the cells are being destroyed (hemolysis) or lost (bleeding) somewhere in the body. This finding would trigger a search for bleeding ulcers or other non-renal causes of anemia.
This test is a functional assessment of the “factory” (bone marrow). It tells the physician whether the factory is shut down or if the products are being lost after leaving the warehouse.

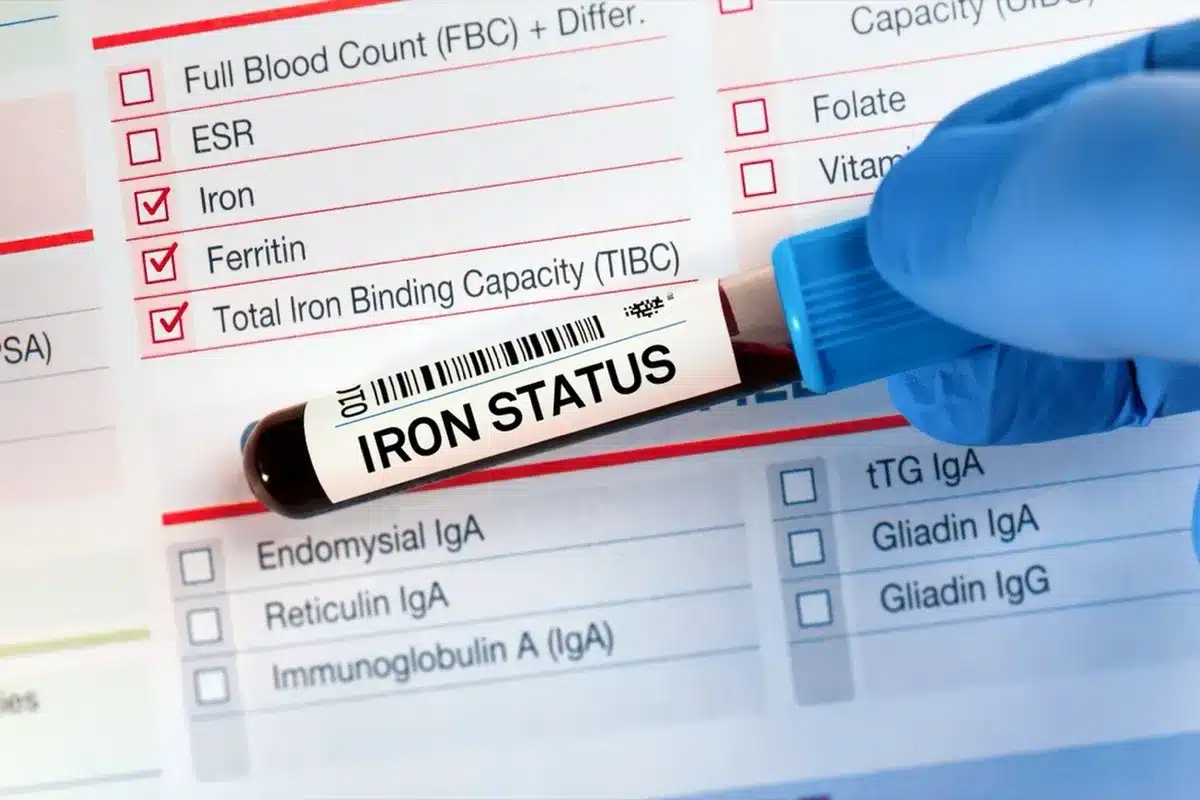
Evaluating iron status in kidney patients requires a specific panel of tests, as standard tests can be misleading. The panel includes serum iron, Total Iron Binding Capacity (TIBC), Transferrin Saturation (TSAT), and Ferritin.
Ferritin measures the total iron stored in the body. However, ferritin is also an acute-phase reactant, meaning it rises during inflammation. A kidney patient may have high ferritin (suggesting plenty of iron) but actually be iron-deficient because the iron is trapped by inflammation.
Transferrin Saturation (TSAT) is often a more reliable indicator of iron availability for red blood cell production. It measures how much iron is actually in transit to the bone marrow. A TSAT below 20% indicates iron deficiency, regardless of the ferritin level.
This nuanced evaluation helps distinguish between absolute iron deficiency (no iron in the body) and functional iron deficiency (iron is present but locked away). This distinction dictates whether the patient needs iron supplements or therapies to mobilize existing iron.
To rule out other causes of anemia, levels of Vitamin B12 and Folate are routinely checked. Deficiency in either of these vitamins impairs DNA synthesis, preventing red blood cells from maturing properly. This results in large, fragile cells that cannot efficiently carry oxygen.
Since kidney patients often have dietary restrictions, these deficiencies are common comorbidities. Identifying and correcting them is a low-risk, high-reward intervention that can significantly improve hemoglobin levels before resorting to hormonal therapies.
Testing also helps rule out pernicious anemia, an autoimmune condition affecting B12 absorption. If these levels are normal, it reinforces the diagnosis of anemia of chronic kidney disease. It is a process of elimination to ensure a pure diagnosis.

Because uremia can cause platelet dysfunction and gastritis, occult (hidden) gastrointestinal bleeding is a common cause of anemia in kidney patients. A stool guaiac test (Fecal Occult Blood Test) checks for microscopic traces of blood in the stool.
If this test is positive or if iron studies suggest blood loss, the patient may be referred for an endoscopy or colonoscopy. These procedures visually inspect the digestive tract to locate and treat bleeding ulcers, polyps, or vascular malformations.
Treating the source of blood loss is critical. There is no point in stimulating the bone marrow to make more blood if it is constantly leaking out through the gut. This step ensures the “bucket” isn’t leaking before the physician tries to fill it.
The diagnostic workup often includes checking for other endocrine disorders that can cause anemia. Severe hyperparathyroidism, common in kidney disease due to mineral imbalance, can cause fibrosis in the bone marrow, crowding out the red blood cell-producing cells.
Measuring Parathyroid Hormone (PTH) levels helps identify this “calcific” barrier to blood production. Similarly, hypothyroidism (low thyroid function) causes a metabolic slowdown that can result in mild anemia.
Thyroid-stimulating hormone (TSH) is measured to rule out thyroid disease. Treating these underlying endocrine imbalances can often improve anemia without the need for specific anemia drugs. It is a holistic approach to the patient’s hormonal health.
In rare cases where the cause of anemia remains elusive despite extensive blood testing, a bone marrow biopsy may be performed. This involves extracting a small sample of marrow from the hip bone for examination under a microscope.
This test can reveal primary bone marrow disorders, such as myelodysplastic syndrome, pure red cell aplasia, or cancer infiltration. It is a definitive test used when the bone marrow fails to respond to treatment as expected.
While invasive, it provides crucial insights into cellular machinery. It can determine if the marrow is empty (aplastic), full of scar tissue (fibrotic), or producing abnormal cells. This distinguishes renal anemia from hematologic cancers.
C-Reactive Protein (CRP) is a marker of systemic inflammation. Measuring CRP helps the physician determine whether inflammation is driving the anemia by blocking iron utilization and suppressing bone marrow function.
High CRP levels suggest that the patient has “inflammatory anemia” overlapping with kidney anemia. This informs the prognosis, as these patients typically require higher doses of erythropoietin-stimulating agents to overcome the inflammatory resistance.
Understanding the inflammatory burden helps tailor the treatment. It may prompt a search for hidden infections (such as an infected dialysis catheter or a foot ulcer) that are driving the inflammation and anemia.


Send us all your questions or requests, and our expert team will assist you.
For patients with chronic kidney disease, the target hemoglobin is typically 10.0-11.5 g/dL. While this is slightly lower than the normal range for healthy people, pushing it higher with medication carries risks of blood clots and stroke.
Generally, a CBC and reticulocyte count do not require fasting. However, if your doctor is also checking your iron, glucose, or lipid levels at the same time, you may need to fast for 8 to 12 hours for accurate results.
Anemia can be caused by internal bleeding that is not visible. Kidney disease can make you prone to stomach ulcers or gut bleeding. The stool test ensures you aren’t losing blood through your digestive system, which would require a different treatment.
If you have Stage 3-5 CKD, you will likely have your hemoglobin checked every 3 months. If you are starting a new treatment for anemia, checking may be more frequent, such as every 2 to 4 weeks, to adjust the dosage safely.
The procedure is done with local anesthesia to numb the skin and the surface of the bone. You will feel pressure and a brief, sharp sensation when the marrow is withdrawn. There is usually some dull aching at the site for a few days afterwards.




Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)