Discover effective CKD anemia treatment at LIV Hospital. We offer expert care, iron therapy, and follow-up to improve your energy and health
Send us all your questions or requests, and our expert team will assist you.
The cornerstone of treatment for severe renal anemia is the administration of Erythropoiesis-Stimulating Agents (ESAs). These are synthetic versions of the natural hormone erythropoietin. Drugs like epoetin alfa and darbepoetin alfa are injected under the skin or intravenously to signal the bone marrow to ramp up red blood cell production.
This therapy replaces the missing signal from the damaged kidneys. It is highly effective at raising hemoglobin levels, reducing the need for blood transfusions, and alleviating the profound fatigue associated with the disease. The dosing is carefully titrated based on the patient’s weight and hemoglobin response.
However, ESAs are powerful drugs with significant risks if used aggressively. Raising hemoglobin too high (above 11.5 or 12 g/dL) increases the risk of stroke, heart attack, and blood clots. Therefore, the goal is not to normalize hemoglobin completely, but to maintain it in a safe range that relieves symptoms.
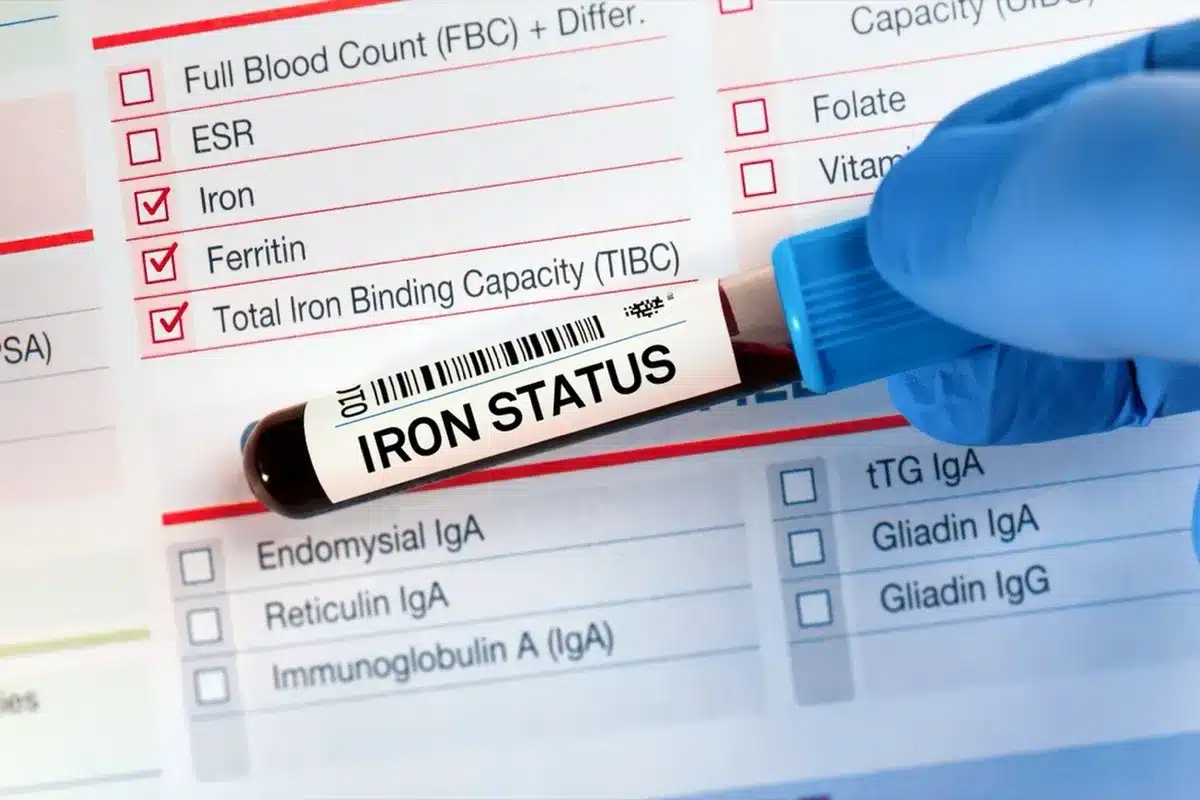
For many kidney patients, oral iron supplements are ineffective due to poor absorption and high hepcidin levels caused by inflammation. Intravenous (IV) iron therapy bypasses the gut entirely, delivering iron directly into the bloodstream where it can be immediately utilized or stored.
IV iron is often required for ESAs to work. Without sufficient iron, the bone marrow cannot produce red blood cells even with ESA stimulation. This combination therapy is the standard of care for dialysis patients and those with advanced CKD.
Infusions are typically given in a clinic setting. Modern iron formulations (such as iron sucrose or ferric gluconate) have a lower risk of allergic reaction than older formulations. The treatment creates a robust iron reserve that supports sustained blood production.

For patients with early-stage kidney disease and mild anemia, oral iron may be the first-line treatment. Ferrous sulfate or ferrous gluconate are common forms. To maximize absorption, patients are advised to take iron on an empty stomach with Vitamin C (or orange juice), which creates an acidic environment that helps iron dissolve.
However, oral iron is notorious for gastrointestinal side effects, including nausea, constipation, and dark stools. These side effects often lead to poor adherence. Newer formulations like ferric citrate or sucroferric oxyhydroxide also act as phosphate binders, treating two kidney problems with one pill.
HIF-PHIs represent a revolutionary new class of oral medications for the treatment of renal anemia. Instead of injecting synthetic hormones, these pills trick the body into thinking it is at a high altitude. They inhibit the enzyme that breaks down Hypoxia-Inducible Factors (HIF).
By stabilizing HIF, these drugs reactivate the body’s natural erythropoietin production, even in damaged kidneys. They also lower hepcidin levels, improving iron absorption and mobilization. This dual mechanism addresses both the hormonal and nutritional roots of the anemia.
Because they are pills, they offer a convenient alternative to injections. They induce a more physiologic, lower level of EPO compared to the high peaks seen with ESAs, which may potentially provide a safer cardiovascular profile. However, long-term safety data is still being gathered.

Transfusions are reserved for acute situations where hemoglobin drops dangerously low or the patient is symptomatic (chest pain, severe shortness of breath). They provide an immediate boost in oxygen-carrying capacity, acting as a bridge until other treatments can take effect.
However, transfusions are not a long-term solution. They carry risks of iron overload, transfusion reactions, and the development of antibodies (sensitization). For patients hoping for a future kidney transplant, sensitization makes it much harder to find a matching donor, so transfusions are avoided whenever possible.
Correcting vitamin deficiencies is a critical adjunct to therapy. Patients with identified deficiencies are prescribed Folic Acid and Vitamin B12 (either oral or injectable cyanocobalamin). This ensures that the red blood cells produced are mature and functional.
Renal vitamins (specifically formulated B-complex vitamins) are often prescribed to dialysis patients to replace the water-soluble vitamins lost during dialysis. This simple intervention supports the overall efficacy of the anemia management plan.
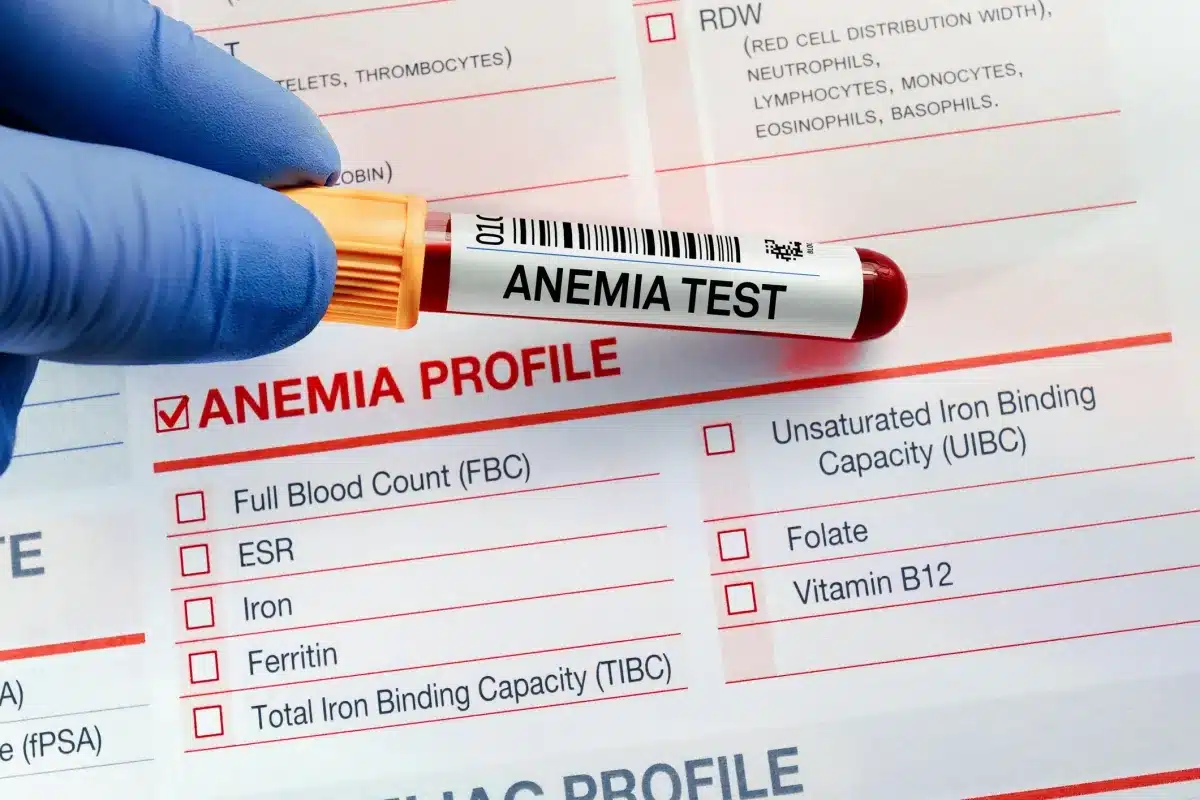
Managing kidney anemia requires vigilant monitoring. Hemoglobin levels are checked frequently (monthly for dialysis patients, quarterly for earlier stages) to ensure the patient stays within the target range. ESAs require dose adjustments based on these trends.
Iron studies are repeated every 3 months to ensure the accelerated blood production does not deplete stores. If ferritin drops too low, iron therapy is re-initiated. This dynamic adjustment prevents the “yo-yo” effect of hemoglobin rising and falling.
Blood pressure monitoring is also part of follow-up, as ESAs can raise blood pressure. The care team looks for signs of adverse events, such as clotting or access thrombosis in dialysis patients. It is a continuous loop of testing, treating, and adjusting.
Effective treatment involves managing the conditions that exacerbate anemia. Controlling hyperparathyroidism removes the barrier to bone marrow fibrosis. Treating infections reduces inflammation and hepcidin levels, making the anemia more responsive to therapy.
Optimizing dialysis adequacy is also crucial. If a patient is underdialyzed, uremic toxins accumulate and suppress bone marrow function. Ensuring the dialysis prescription is sufficient to clear enough toxins is a fundamental step in treating the anemia of ESRD.


Send us all your questions or requests, and our expert team will assist you.
EPO is not a quick fix. It typically takes 2 to 6 weeks to see a noticeable rise in hemoglobin levels. This is because it takes time for the bone marrow to ramp up production and for new cells to mature and enter circulation.
Modern IV iron formulations are generally very safe. The risk of severe allergic reaction is extremely low (less than 1%). Most side effects are mild, such as temporary nausea or a metallic taste in the mouth during the infusion.
Usually, no. Renal anemia is a chronic condition caused by permanent kidney damage. If you stop the medication, your hemoglobin will likely drop again. Maintenance doses are required to keep your levels stable.
Current guidelines suggest a target hemoglobin between 10 and 11.5 g/dL. Aiming for “normal” levels (above 13) with medication has been shown to increase the risk of stroke and heart attack in kidney patients, so the target is lower than for healthy people.
EPO is the gas pedal, but iron is the fuel. Pushing the gas pedal (EPO) without fuel (iron) won’t make the car go. The bone marrow needs a massive amount of iron to build new blood cells when stimulated by EPO.





Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)