Alzheimer’s disease is a complex condition. It is marked by the buildup of amyloid-beta plaques and tau protein in the brain. These changes harm the brain’s cells, causing memory loss and cognitive decline.
Recent studies show that amyloid-beta peptide aggregation and tau protein dysregulation are key in the disease’s development.
At Liv Hospital, we focus on how these proteins harm the brain. New findings suggest that tau protein might be more harmful to the brain than thought. By studying the effects of beta-amyloid plaques and tau protein, we aim to find better treatments for this disease.
Key Takeaways
- Alzheimer’s disease is characterized by the accumulation of amyloid-beta plaques and tau protein.
- The aggregation of these proteins disrupts nerve cell communication and leads to brain cell death.
- Recent research highlights the role of amyloid-beta peptide aggregation and tau protein dysregulation.
- Understanding the impact of these proteins is key to developing effective treatments.
- Liv Hospital is dedicated to advancing research on Alzheimer’s disease and its causes.
The Pathological Hallmarks of Alzheimer’s Disease

Understanding Alzheimer’s disease is key to finding treatments. It’s a complex disorder with specific brain changes.
Defining the Two Primary Markers
The main signs of Alzheimer’s are amyloid-beta plaques and neurofibrillary tangles. Plaques are deposits of amyloid-beta between neurons. Tangles are inside neurons, made of tau protein.
Studies link these signs to Alzheimer’s progression. Knowing about them helps us understand the disease better.
|
Pathological Feature |
Description |
Composition |
|---|---|---|
|
Amyloid-beta Plaques |
Extracellular deposits |
Amyloid-beta peptide |
|
Neurofibrillary Tangles |
Intracellular inclusions |
Hyperphosphorylated tau protein |
“The accumulation of amyloid-beta plaques and neurofibrillary tangles is a hallmark of Alzheimer’s disease, and understanding their role is critical for developing therapeutic strategies.”(2)
Historical Understanding of Alzheimer’s Pathology
Alzheimer’s disease was first identified in the early 1900s by Alois Alzheimer. He found plaques and tangles in a patient’s brain. This discovery has led to a lot of research.
Our understanding of Alzheimer’s has grown a lot. Now, we focus on amyloid-beta and tau protein’s role in the disease.
Understanding Healthy Brain Function
To understand Alzheimer’s impact, we must first grasp how a healthy brain works. The brain is a complex network of neurons that talk to each other. This talking helps with thinking and moving.
“The healthy brain is a remarkable organ, capable of processing vast amounts of information and controlling the body’s functions with precision,” as noted by neurological experts. This complex process depends on the health and function of neurons.
Normal Neuronal Communication
Neurons talk through electrical and chemical signals. This talking is key to all brain activities. The structure of neurons, including microtubules, is vital for this communication.
Tau protein plays a critical role in keeping these microtubules stable. This stability helps nutrients and important molecules move along the axon.
Neurons also need proteins to work right. Proteins help with learning and memory. If proteins don’t work right, it can lead to diseases like Alzheimer’s.
The Role of Proteins in Brain Health
Proteins do a lot in the cell to keep the brain healthy. In healthy neurons, tau protein helps keep microtubules stable. Other proteins help with sending signals and keeping neurons alive. It’s important for the brain to keep these proteins in balance.
As we get older, proteins can start to work wrong. This can lead to diseases. Knowing how proteins work in a healthy brain helps us understand these diseases better.
The role of tau protein in keeping microtubules stable is huge. When tau protein doesn’t work right, it can cause Alzheimer’s. This leads to tangles that mess up how neurons talk to each other.
Tau Protein’s Normal Function in Healthy Neurons
Tau protein is key to keeping neurons healthy. Knowing how it works in healthy neurons helps us understand Alzheimer’s disease better.
We’ll look at tau protein’s role in keeping neurons stable and helping them transport materials. These tasks are vital for the neuron’s structure and function.
Microtubule Stabilization
Tau protein helps keep microtubules stable. Microtubules are important for neuron shape, transport, and cell division. Tau protein binds to them, keeping them stable.
This stability is essential for neuron function. It helps the neuron keep its shape and transport materials well. This is important for brain communication.
“Tau protein’s interaction with microtubules is a key aspect of its normal function, and alterations in this interaction are associated with neurodegenerative diseases.”
Axonal Transport and Structural Support
Tau protein also plays a big role in axonal transport. This is how proteins and other materials move in the neuron. Tau protein helps control this movement by binding to microtubules.
It also supports the neuron’s structure. By stabilizing microtubules, tau protein helps the neuron handle stress and keep its shape.
Comparing tau protein’s role in healthy neurons to those with Alzheimer’s shows its importance. The table below highlights the main differences:
|
Function |
Healthy Neurons |
Alzheimer’s Disease |
|---|---|---|
|
Microtubule Stabilization |
Tau protein stabilizes microtubules, maintaining neuronal structure. |
Hyperphosphorylated tau protein forms neurofibrillary tangles, disrupting microtubule stability. |
|
Axonal Transport |
Tau protein regulates axonal transport, ensuring efficient neuronal communication. |
Abnormal tau protein aggregation impairs axonal transport, contributing to neuronal dysfunction. |
In conclusion, tau protein’s role in healthy neurons is complex. It stabilizes microtubules and helps with axonal transport. Understanding these roles is key to fighting Alzheimer’s disease.
Neurofibrillary Tangles Tau Protein Formation in Alzheimer’s
Alzheimer’s disease is marked by the formation of neurofibrillary tangles. These tangles are made from tau protein that has undergone a pathological change. They are a key part of Alzheimer’s disease.
Hyperphosphorylation Process
In Alzheimer’s, tau protein gets too many phosphate groups. This is called hyperphosphorylation. It’s a key step in making neurofibrillary tangles.
When tau is hyperphosphorylated, it breaks away from microtubules. It then forms insoluble aggregates. This is helped by kinases that add phosphate groups to tau at specific sites.
From Soluble Aggregates to Fibrils
First, hyperphosphorylated tau forms soluble aggregates. Then, these aggregates turn into insoluble fibrils. These fibrils are the main part of neurofibrillary tangles.
Studies show that making tau fibrils is a complex process. It involves the oligomerization of tau protein. These oligomers then form fibrils, which are typical of neurofibrillary tangles. Knowing this process is key to finding treatments for Alzheimer’s.
Spreading Between Neurons
Neurofibrillary tangles are not just static; they spread between neurons. This spread is a big part of how Alzheimer’s disease gets worse. Tau aggregates are released from affected neurons and taken up by others.
This spread of tau pathology is a major factor in Alzheimer’s disease spreading through the brain. Scientists are working hard to understand how this happens. They hope to find new ways to treat the disease.
|
Stage |
Description |
Pathological Features |
|---|---|---|
|
1 |
Initial Hyperphosphorylation |
Tau protein becomes excessively phosphorylated |
|
2 |
Formation of Soluble Aggregates |
Hyperphosphorylated tau forms soluble aggregates |
|
3 |
Maturation into Fibrils |
Soluble aggregates mature into insoluble fibrils |
|
4 |
Spreading Between Neurons |
Tau fibrils spread to neighboring neurons |
The formation of neurofibrillary tangles is a complex process. It starts with the hyperphosphorylation of tau protein. Understanding these steps is vital for finding effective treatments for Alzheimer’s.
“The accumulation of tau protein in neurofibrillary tangles is a defining feature of Alzheimer’s disease, and understanding its formation is key to developing therapeutic interventions.” Medical Expert, Alzheimer’s Researcher
Beta-Amyloid: From Precursor Protein to Plaques
Beta-amyloid plaques are a key sign of Alzheimer’s disease. They come from how amyloid precursor protein is processed. Knowing this helps us understand Alzheimer’s better.
Amyloid Precursor Protein Processing
Amyloid precursor protein (APP) is a membrane protein. It gets cut by enzymes called secretases. This creates beta-amyloid peptides, which tend to stick together.
How APP is processed is very important. Abnormal APP processing means too much beta-amyloid. This is a big part of why Alzheimer’s happens.
Formation of Oligomers and Fibrils
Beta-amyloid peptides form oligomers first. These are small and can dissolve. Then, they turn into fibrils, which are more solid.
Turning into oligomers and fibrils is a big step. Oligomers are very harmful to brain cells. They mess up how cells work and hurt them.
Extracellular Plaque Development
Beta-amyloid fibrils build up outside brain cells. This makes senile plaques, a key sign of Alzheimer’s. These plaques also bring in immune cells, showing the brain is fighting something.
|
Stage |
Description |
Key Features |
|---|---|---|
|
APP Processing |
Cleavage of APP by secretases |
Generation of beta-amyloid peptides |
|
Oligomer Formation |
Aggregation of beta-amyloid peptides |
Formation of small, soluble aggregates |
|
Plaque Development |
Accumulation of fibrils in extracellular space |
Formation of senile plaques, inflammatory response |
Understanding how beta-amyloid plaques form is key to fighting Alzheimer’s. Studying APP processing, oligomer formation, and plaque growth helps find new treatments.
The Brain’s Clearing Mechanisms and Their Failure
The brain has special systems to keep itself clean. These include the glymphatic system and microglial clearance. But in Alzheimer’s disease, these systems can’t keep up.
Glymphatic System Function
The glymphatic system is a new discovery that helps remove waste from the brain. It works best when we sleep. This shows how important sleep is for our brain’s health.
When we’re awake, the glymphatic system doesn’t work as well. It slows down in clearing waste. As we get older, this system gets worse, leading to more toxic proteins in Alzheimer’s.
Microglial Clearance Dysfunction
Microglia are the brain’s immune cells. They help remove waste and pathogens, including amyloid-beta plaques. But in Alzheimer’s, they don’t work right, leading to more amyloid-beta.
Studies link microglial dysfunction to Alzheimer’s risk genes. This shows a connection between the immune system and the disease. Learning more about microglial clearance could help find new treatments.
|
Clearing Mechanism |
Function in Healthy Brain |
Dysfunction in Alzheimer’s |
|---|---|---|
|
Glymphatic System |
Removes soluble amyloid-beta and other waste products |
Reduced efficiency with age, contributing to amyloid-beta accumulation |
|
Microglial Clearance |
Clears pathogens and waste products, including amyloid-beta plaques |
Impaired function, associated with genetic risk factors for Alzheimer’s |
The failure of the brain’s clearing mechanisms is key in Alzheimer’s disease. Learning about these mechanisms and their failure can help us understand the disease better. It also opens up new ways to treat it.
Molecular Mechanisms of Neuronal Damage
The ways neurons get damaged in Alzheimer’s disease are complex. The disease causes proteins to build up, like tau and beta-amyloid. This buildup starts a chain reaction that harms neurons and leads to their death.
Synaptic Dysfunction and Loss
Synaptic dysfunction is a key feature of Alzheimer’s. It starts early in the disease. Beta-amyloid oligomers mess with how neurons talk to each other, affecting their ability to change and adapt.
This messes up the connections between neurons. As these connections fade, thinking skills start to decline.
Mitochondrial Impairment
Mitochondria are vital for cell energy. In Alzheimer’s, they don’t work right because of beta-amyloid and tau. This means neurons don’t get the energy they need.
Without enough energy, neurons can’t survive. They die off, leading to more damage.
Disruption of Calcium Homeostasis
Calcium is important for how neurons work. It helps with sending signals and changing how neurons connect. In Alzheimer’s, beta-amyloid and tau mess with calcium levels.
This causes too much calcium inside neurons. This can lead to neurons getting damaged or dying.
|
Molecular Mechanism |
Description |
Impact on Neurons |
|---|---|---|
|
Synaptic Dysfunction |
Disruption of synaptic plasticity and loss of synapses due to beta-amyloid oligomers |
Cognitive decline, loss of neuronal connections |
|
Mitochondrial Impairment |
Decreased energy production, increased oxidative stress due to beta-amyloid and tau accumulation |
Neuronal death, decreased cellular energy |
|
Disruption of Calcium Homeostasis |
Abnormal increase in intracellular calcium levels due to beta-amyloid and tau pathology |
Excitotoxicity, neuronal damage |
Knowing how neurons get damaged in Alzheimer’s is key. It helps us find new ways to stop or slow down this damage.
Brain Regions Affected by Alzheimer’s Pathology
It’s important to know which brain areas Alzheimer’s affects. This helps us understand how the disease progresses. Alzheimer’s impacts certain brain parts, causing memory loss and cognitive decline.
Hippocampal and Entorhinal Cortex Vulnerability
The hippocampus and entorhinal cortex are hit hard by Alzheimer’s early on. The hippocampus is key for memory. The entorhinal cortex connects the hippocampus to the neocortex. Damage here messes up memory processing, leading to memory loss in Alzheimer’s patients.
Progression Through Neocortical Regions
As Alzheimer’s gets worse, it spreads to neocortical areas like the temporal, parietal, and frontal lobes. This spread brings more symptoms, showing how different brain parts are affected. The disease’s growth through these areas is a key sign of its progression.
Braak Staging of Tau Pathology
The Braak staging system tracks tau pathology in Alzheimer’s. It divides the disease into stages based on neurofibrillary tangles and neuropil threads. The stages start with I-II, where only the transentorhinal region is affected, and go up to V-VI, with severe neocortical involvement.
|
Braak Stage |
Description |
Pathological Features |
|---|---|---|
|
I-II |
Transentorhinal stage |
Pathology limited to the transentorhinal region |
|
III-IV |
Limbic stage |
Involvement of the hippocampus and other limbic structures |
|
V-VI |
Neocortical stage |
Severe neocortical involvement |
The Braak staging system helps us understand Alzheimer’s progression. It shows how tau pathology changes over time, linking to symptoms.
The Tau-Amyloid Relationship in Disease Progression
The connection between tau protein and amyloid-beta is key to grasping Alzheimer’s disease. Alzheimer’s is marked by the buildup of tau neurofibrillary tangles and amyloid-beta plaques. Scientists are deeply studying how these proteins affect the disease’s progression.
The Amyloid Cascade Hypothesis
The amyloid cascade hypothesis suggests amyloid-beta buildup starts Alzheimer’s disease. It leads to tau hyperphosphorylation, tangle formation, and neuron loss. This idea is backed by genetic studies on familial Alzheimer’s disease, where APP gene mutations increase amyloid-beta.
Amyloid-beta can also cause tau problems, linking the two protein aggregates. For example, amyloid-beta oligomers can make tau more prone to hyperphosphorylation and aggregation.
|
Protein |
Role in Alzheimer’s |
Pathological Features |
|---|---|---|
|
Amyloid-beta |
Primary event in disease pathogenesis |
Extracellular plaques |
|
Tau |
Neurofibrillary tangle formation |
Intracellular tangles |
Evidence for Tau-Driven Pathology
While amyloid-beta is central to the amyloid cascade hypothesis, tau’s role in Alzheimer’s is becoming clearer. Tau’s pathology is linked to cognitive decline and neuron loss.
Studies also show tau can spread between neurons, worsening Alzheimer’s. This spread is thought to be aided by amyloid-beta.
Current Understanding of Their Interaction
The interaction between tau and amyloid-beta is complex and bidirectional. Amyloid-beta can influence tau, and tau can affect amyloid-beta.
Studying the tau-amyloid relationship is vital for finding Alzheimer’s treatments. It helps in creating therapies that target the disease’s root causes.
We’re making strides in understanding Alzheimer’s. Further research into the tau-amyloid relationship is key to finding effective treatments.
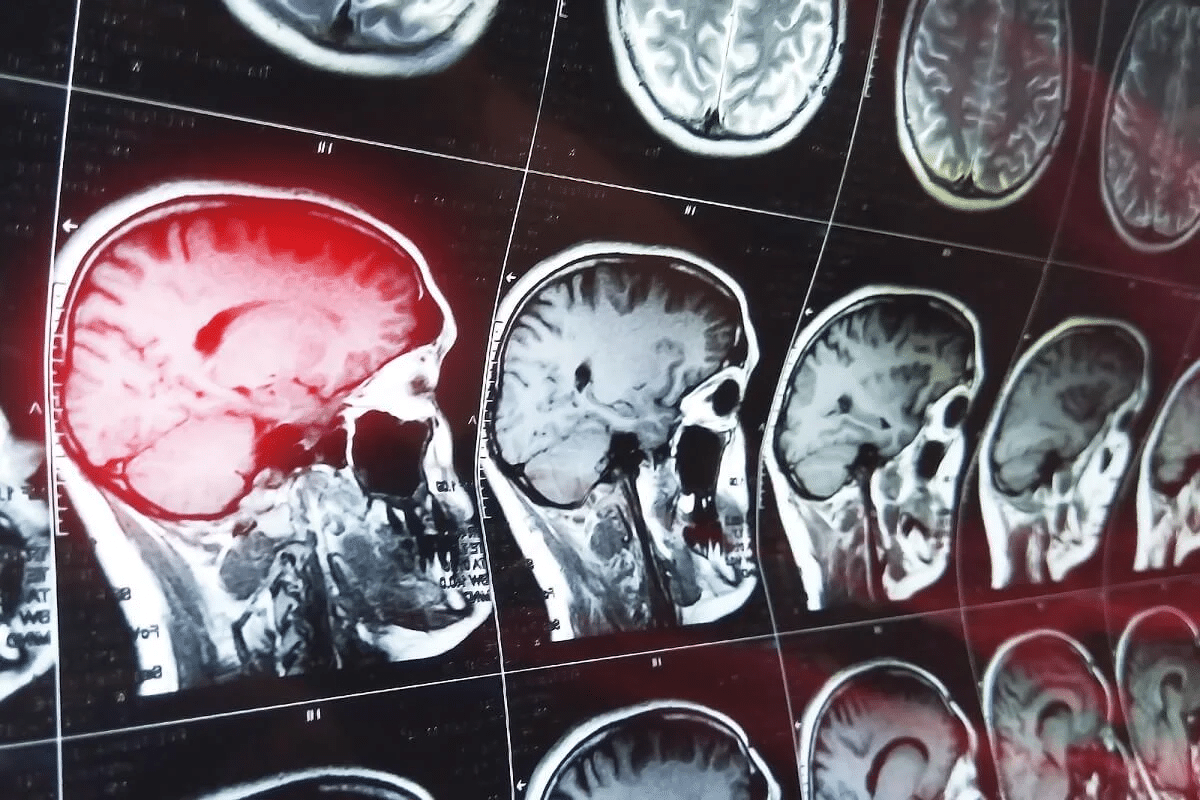
Visualizing Protein Aggregates: Diagnostic Imaging
Diagnostic imaging is key in understanding Alzheimer’s disease. It helps us see protein aggregates in the brain. New imaging methods have made diagnosing and tracking this disease better.
PET Imaging of Amyloid and Tau
Positron Emission Tomography (PET) imaging is a powerful tool. It detects amyloid and tau protein aggregates in the living brain. By using special radiotracers, PET imaging shows where and how much of these proteins are present. This helps us understand the disease and how well treatments work.
Correlation Between Protein Burden and Symptoms
Research shows amyloid and tau protein burden affects Alzheimer’s symptoms. PET imaging lets us study this link in real-time. It helps us see how these proteins lead to cognitive decline and other symptoms.
- Amyloid Burden: High levels of amyloid plaques are linked to faster cognitive decline.
- Tau Pathology: Tau neurofibrillary tangles spread with neurodegeneration and cognitive symptoms.
Emerging Biomarkers in Blood and CSF
Researchers are also looking at biomarkers in blood and cerebrospinal fluid (CSF). These include amyloid-beta, tau protein, and other neurodegeneration markers. Blood-based biomarkers could make diagnosing Alzheimer’s easier and less invasive than PET imaging and CSF analysis.
Studies suggest some biomarkers in blood and CSF can predict Alzheimer’s years before symptoms start. This early detection could lead to better treatment outcomes.
Therapeutic Approaches Targeting Tau and Beta-Amyloid
Our understanding of Alzheimer’s disease is growing. Therapies targeting tau and beta-amyloid are becoming more important. Researchers are working on treatments to slow or stop the disease by focusing on these proteins.
Anti-Amyloid Antibodies and Vaccines
Anti-amyloid antibodies and vaccines are key in Alzheimer’s treatment. They aim to remove beta-amyloid plaques from the brain. This could slow the disease’s progress. Monoclonal antibodies are showing promise in trials by targeting amyloid-beta peptides.
Aducanumab is an anti-amyloid antibody getting a lot of attention. It has shown to reduce amyloid plaques in the brain. Its effect on cognitive decline is being studied, but it’s a big step in anti-amyloid therapy.
Tau-Focused Interventions
Researchers are also looking into tau-focused interventions. These aim to stop neurofibrillary tangles from forming or to clear them. Tau-targeting antibodies and tau aggregation inhibitors are being explored.
Tau-focused therapies are important because tau pathology is linked to cognitive decline in Alzheimer’s. By tackling tau, these treatments could slow or stop the disease’s progression.
Combination Therapies Under Investigation
Researchers are now looking at combination therapies targeting both tau and beta-amyloid. These aim to tackle the multiple causes of Alzheimer’s disease.
Combination therapies might pair anti-amyloid antibodies with tau-targeting agents. Early trials are checking their safety and effectiveness. This offers hope for more effective treatments in the future.
Conclusion
Understanding how tau protein and beta-amyloid work together is key to fighting Alzheimer’s disease. These proteins cause brain damage and lead to memory loss. This is why Alzheimer’s is so hard to treat.
We’ve learned a lot about Alzheimer’s through studying tau protein and beta-amyloid. This research helps us find new ways to stop brain damage. It also shows how the brain tries to clean itself but fails in Alzheimer’s.
As we learn more about Alzheimer’s, knowing about tau protein and beta-amyloid becomes more important. This knowledge helps us find better ways to diagnose and treat the disease. By studying these proteins, we can create new treatments that target the disease’s root causes.
FAQ
What are the primary pathological markers of Alzheimer’s disease?
The main signs of Alzheimer’s disease are amyloid-beta plaques and neurofibrillary tangles. These are made of tau protein.
How does tau protein function in healthy neurons?
Tau protein helps keep neurons stable. It does this by supporting microtubules and helping with axonal transport.
What is the process of forming neurofibrillary tangles in Alzheimer’s disease?
Neurofibrillary tangles form when tau protein is over-phosphorylated. This leads to the creation of soluble aggregates. These then form fibrils.
How do beta-amyloid plaques form in Alzheimer’s disease?
Beta-amyloid plaques come from amyloid precursor protein processing. This results in oligomers and fibrils that build up as plaques outside cells.
What is the role of the brain’s clearing mechanisms in Alzheimer’s disease?
The brain’s clearing systems, like the glymphatic system and microglial clearance, are key. They help remove amyloid-beta and other waste. Their failure leads to amyloid-beta plaque buildup.
What are the molecular mechanisms underlying neuronal damage in Alzheimer’s disease?
Neuronal damage in Alzheimer’s disease is caused by several factors. These include synaptic dysfunction, mitochondrial impairment, and calcium homeostasis disruption. All these contribute to neurodegeneration.
Which brain regions are affected by Alzheimer’s pathology?
Alzheimer’s disease impacts many brain areas. These include the hippocampus, entorhinal cortex, and neocortical regions. The disease’s progression is tracked by the Braak staging of tau pathology.
What is the relationship between tau and amyloid-beta in Alzheimer’s disease progression?
The relationship between tau and amyloid-beta is complex. Both the amyloid cascade hypothesis and tau-driven pathology are supported. Their interaction is key to understanding disease progression.
How is diagnostic imaging used in Alzheimer’s disease?
Diagnostic imaging, like PET imaging, is used to see amyloid and tau aggregates. It helps link protein burden to symptoms. It also identifies new biomarkers.
What therapeutic approaches are being explored to target tau and beta-amyloid in Alzheimer’s disease?
Therapies targeting tau and beta-amyloid include anti-amyloid antibodies and tau-focused interventions. Combination therapies are also explored. These aim to slow or halt disease progression.
How do Alzheimer’s disease brain changes affect nerve cells?
Alzheimer’s disease changes disrupt normal neuronal function. The buildup of amyloid-beta plaques and neurofibrillary tangles leads to neurodegeneration.
What is the impact of Alzheimer’s disease on brain function?
Alzheimer’s disease severely impairs brain function. It affects memory, cognition, and daily activities. As the disease progresses, disability increases.
Reference
Government Health Resource. Evidence-Based Medical Guidance. Retrieved from https://jamanetwork.com/journals/jamaneurology/fullarticle/1817720






