Last Updated on December 2, 2025 by Bilal Hasdemir

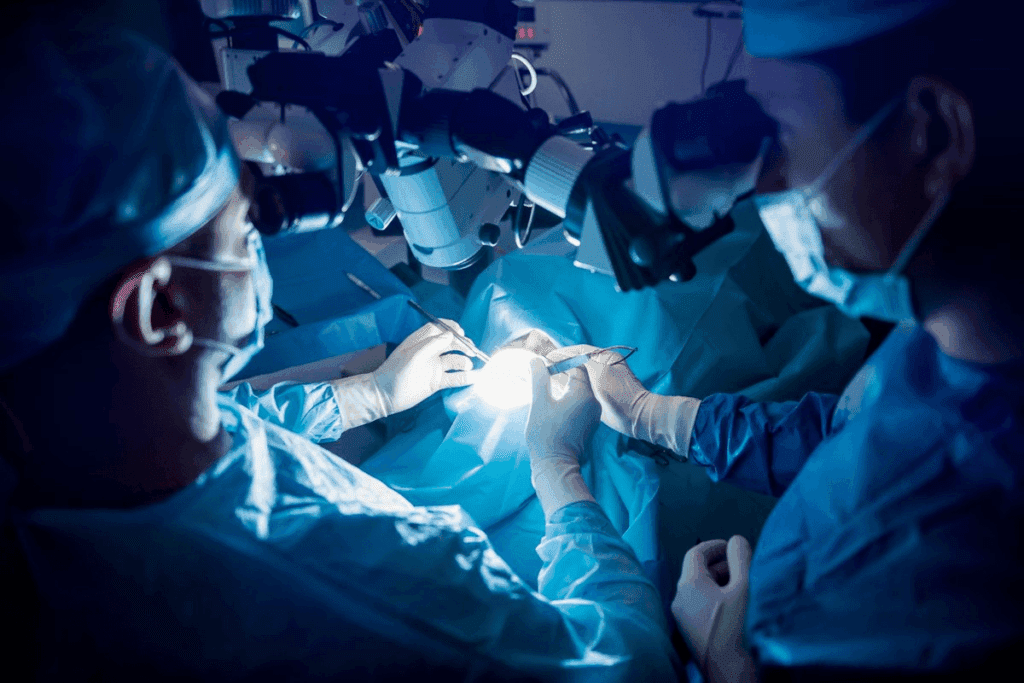
A strategic timeline for pain medication administration is essential for effective pain management after colon surgery.An expert guide to pain medication after colon surgery. Learn the critical options, from IVs to pills, and essential management tips.
At our international healthcare facility, we focus on top-notch medical support and premium service. Our team works hard to make sure patients get all the care they need. This care goes from the first visit to after the surgery recovery.
Key Takeaways
- Effective pain management is critical for recovery after colon surgery.
- Personalized care plans are tailored to individual patient needs.
- Our facility offers extensive medical support and premium service quality.
- Proper Page management strategies can improve patient outcomes.
- We prioritize delivering exceptional international healthcare.
Understanding Pain Management Post-Colon Surgery
Importance of Pain Relief
Pain relief is vital for many reasons. It lowers stress and anxiety, helping with recovery. It also lets patients move around sooner, cutting down on risks like blood clots and pneumonia. We make pain relief a top priority in care after surgery.
The OPERAS study shows how important it is to tailor pain management. It shows that plans made just for each patient can greatly improve results.
Factors Affecting Pain Management
Many things can change how pain is managed after colon surgery. These include:
- The patient’s overall health and medical history
- The type of surgical procedure performed
- The patient’s pain tolerance
- The presence of any comorbidities
Knowing these factors helps doctors create individualized pain management plans. These plans meet the unique needs of each patient.
Factor | Impact on Pain Management |
Overall Health | Pre-existing conditions can affect pain perception and management. |
Type of Surgery | The extent and type of surgery influence the level of post-operative pain. |
Pain Tolerance | Individual differences in pain tolerance affect the approach to pain management. |
Role of the Medical Team
The medical team is key in managing pain. We work with patients to check their pain, adjust plans, and teach about pain relief. Our team includes surgeons, anesthesiologists, nurses, and more. We all work together for complete care.
Highlighting the medical team’s role demonstrates our commitment to personalized and premium care.
Pain management is key after colon surgery. Knowing the different pain meds is important for both patients and doctors. We aim to ease pain without harming the patient.
Opioids
Opioids are strong pain relievers used after surgery. They block pain signals in the brain and spinal cord. Oxycodone and hydrocodone are examples. But, they can lead to addiction and slow breathing.
It’s common for opioids to be given too much after surgery. We look for better ways to manage pain. We help decide if opioids are right and watch how they’re used.
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
NSAIDs reduce inflammation and pain. They block enzymes that cause pain. Ibuprofen and naproxen are examples. They work well for mild to moderate pain after surgery.
But, NSAIDs can cause stomach problems and kidney issues. They’re safer than opioids for long-term use. They don’t lead to addiction.
Acetaminophen
Acetaminophen is a pain reliever that lowers pain chemicals in the brain. It’s good for mild to moderate pain. It’s often used with other meds.
Unlike NSAIDs, acetaminophen doesn’t reduce inflammation. But, it’s gentler on the stomach. It’s important to take it as directed to avoid liver damage.
Knowing the good and bad of these meds helps us create the best pain plans. We make sure pain relief is effective and safe for each patient.
Opioid Medications After Surgery
Opioid medications play a key role in managing pain after surgery. They are strong pain relievers often given for moderate to severe pain. We will look into the types of opioids, their risks and benefits, and how to use them safely.
Examples of Opioids Prescribed
Several opioid medications are commonly given after surgery. These include:
- Oxycodone: Often used for managing moderate to severe pain.
- Hydrocodone: Combined with acetaminophen, it’s effective for pain relief.
- Morphine: Used for severe pain, mostly in hospitals.
- Fentanyl: A strong opioid, often used in patch form for continuous pain relief.
These medications are effective but must be used carefully due to their risk of dependency and side effects.
Risks and Benefits
Opioid medications have both good and bad sides. They help a lot with pain, making recovery easier. But, they can also lead to dependency, addiction, and side effects like constipation, nausea, and drowsiness.
Benefits | Risks |
Effective pain relief | Risk of dependency and addiction |
Improves recovery comfort | Side effects (constipation, nausea, drowsiness) |
Guidelines for Use
To use opioid medications safely, follow these guidelines:
- Follow the prescribed dosage and duration strictly.
- Be aware of possible side effects and tell your healthcare provider.
- Don’t mix opioids with alcohol or other sedatives.
- Slowly stop taking opioids as your healthcare provider advises to avoid withdrawal.
By following these guidelines, patients can reduce the risks of opioid use and get the most benefits.
Non-Opioid Alternatives
Healthcare providers are now looking at non-opioid options for pain relief after colon surgery. This is to reduce opioid dependency. They aim to find pain management strategies that are effective and safe.
Benefits of NSAIDs
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) are effective for post-surgical pain. NSAIDs reduce inflammation, which is a big part of post-surgery pain. They block enzymes that cause inflammation, helping to ease pain.
Using NSAIDs can help avoid opioid dependency. But, it’s important to follow the dosage to avoid side effects.
Acetaminophen vs. NSAIDs
Acetaminophen and NSAIDs are both used for pain, but in different ways. Acetaminophen helps with pain and fever, while NSAIDs also fight inflammation. The choice depends on your health, surgery type, and pain needs.
Characteristics | Acetaminophen | NSAIDs |
Pain Relief | Effective for mild to moderate pain | Effective for moderate to severe pain with anti-inflammatory effects |
Side Effects | Liver damage with overdose | Gastrointestinal issues, kidney damage with prolonged use |
Usage | Commonly used for general pain relief | Used for pain relief with inflammation |
When to Consider Non-Opioid Options
Non-opioid options are good for those at risk of opioid dependency. can also help. They can be used with non-opioid meds for better pain relief.
Talk to your healthcare provider about non-opioid options for your colon surgery pain. They can help find the best strategy for you.
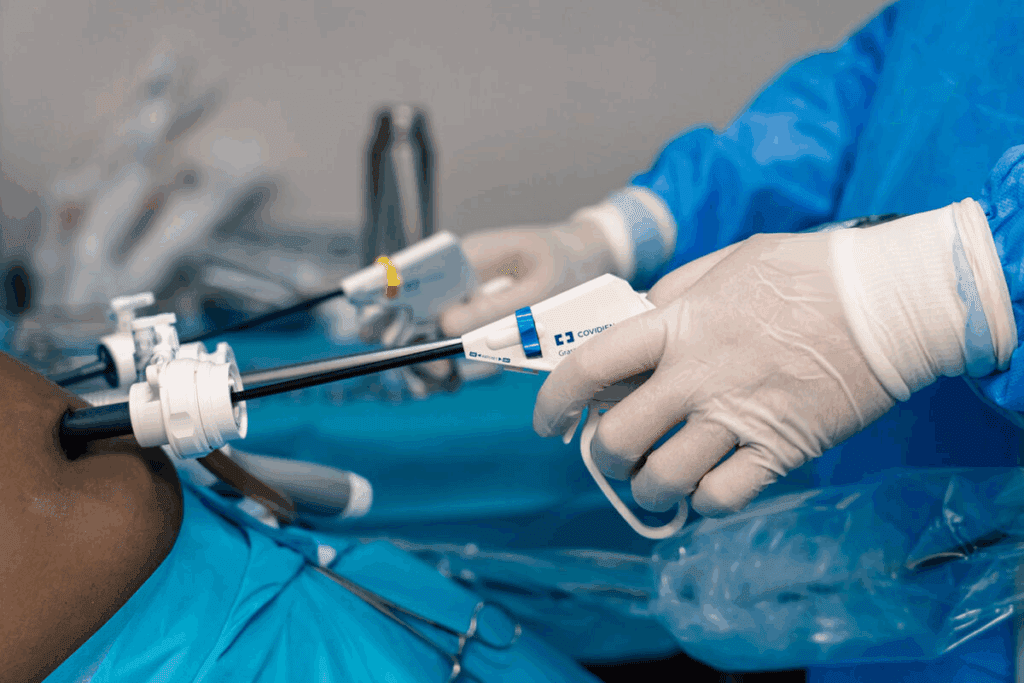
Patient-Controlled Analgesia (PCA)
Patient-Controlled Analgesia (PCA) is a big step forward in managing pain after surgery. It lets patients control their pain by giving themselves medicine when they need it. This can make them feel more comfortable and help them recover better.
What is PCA?
PCA lets patients manage their pain by giving themselves a set dose of pain medicine. This is really helpful after surgery, because it helps them feel better quickly. They use a special pump to get the medicine into their veins fast.
How it Works
The PCA system has a pump that doctors set up to give a certain amount of medicine when the patient presses a button. This lets patients take charge of their pain, which is great for times when they might feel more pain, like when they cough or move. It also has safety features to stop too much medicine from being given.
Advantages of PCA
The benefits of PCA include:
- Improved pain control: PCA lets patients give themselves medicine when they need it, which can make their pain better.
- Increased patient satisfaction: Patients like being able to control their pain, which makes them happier with their care.
- Potential reduction in opioid consumption: PCA might mean patients use less opioid medicine than they would with other methods.
Overall, PCA is a great tool in post-operative care. It balances effective pain management with giving patients more control over their recovery.
A strategic timeline for pain medication administration is essential for effective pain management after colon surgery.
A strategic timeline for pain medication administration is essential for effective pain management after colon surgery. We explain how pain management changes from right after surgery to when it’s no longer needed.
Immediate Post-Operative Period
Right after colon surgery, pain meds are given through IV or epidural. This method quickly relieves pain and works well in the first 24 to 48 hours.
We use patient-controlled analgesia (PCA) or epidural to let patients control their pain. This makes them more comfortable and less worried about pain.
Transitioning to Oral Medic Page ations
When patients can take meds by mouth, we switch from IV or epidural to oral meds. This happens when they can safely take meds orally and their pain is well-managed.
- Oral oxycodons or hydrocodone are used for moderate to severe pain.
- For mild to moderate pain, or as a boost to opioids, NSAIDs or acetaminophen are suggested.
We aim to reduce IV or epidural use while keeping pain under control. This helps patients move around sooner and lowers the risk of bed rest problems.
Discontinuation of Pain Medications
Stopping pain meds is done slowly and based on each patient’s recovery. We check their pain often and change their treatment as needed.
As patients get better, we slowly reduce the amount and how often they take pain meds. This lowers the chance of addiction and keeps them safe from side effects.
We teach patients how to safely use pain meds. This includes knowing the right dose, possible side effects, and why they should follow their treatment plan.
Managing Side Effects of Pain Medications
We know that pain meds are key for healing after colon surgery. But, they can also cause side effects. It’s important to understand these and how to manage them for a smooth recovery.
Common Side Effects
Pain meds, like opioids and NSAIDs, can lead to side effects. Some common ones include:
- Nausea and Vomiting: Opioids can cause this. Anti-nausea meds can help. Stronger opioids make it worse.
- Constipation: Opioids slow down bowel movements. Drinking water and using stool softeners can help.
- Drowsiness and Dizziness: Be careful when standing up to avoid falls.
- Itching or Rash: Some people get itching or rashes from certain meds.
Strategies to Mitigate Discomfort
To lessen side effects, try these strategies:
- Adjusting Medication: Changing the dosage or type of pain med might help.
- Supportive Care: Anti-nausea meds, stool softeners, or other treatments can help manage side effects.
- Monitoring: Regular check-ins with healthcare providers can lead to quick help.
When to Contact a Healthcare Provider
Know when to call a healthcare provider for side effects. Contact them if you experience:
- Severe or Persistent Side Effects: If side effects are bad, get worse, or don’t get better with support.
- Signs of Allergic Reaction: Trouble breathing, fast heartbeat, or swelling in the face, lips, or throat.
- Concerns About Medication: Any questions or worries about pain meds or their side effects should be talked about with a healthcare provider.
By understanding and managing pain medication side effects, we can help our patients recover more comfortably after colon surgery.
Individualized Pain Management Plans
A strategic timeline for pain medication administration is essential for effective pain management after colon surgery.know each patient is different. We create individualized pain management plans for the best recovery.
Page>
Factors Influencing Individual Plans
Many things shape personalized pain management strategies. These include:
- Patient’s medical history and current health status
- Type Page of surgery performed and complexity
- patient pain tolerance and previous experiences with management>
- Potential interactions with other medications
- We tailor pain management plans based on these factors. For example, patients with opioid use history need different strategies than those who are opioid-naive.
Factor | Consideration | Impact on Pain Management |
Medical History | Previous surgeries, allergies, and health conditions | Guides the selection of appropriate pain medications |
Pain Tolerance | Patient’s previous experiences with pain | Influences the dosage and type of pain medication |
Current Medications | Potential interactions with pain medications | Affects the choice of pain management strategy |
Importance of Communication with Healthcare Providers
- Effective> communication between patients and healthcare providers is crucial for successful pain management plans. We encourage our patients to share their pain levels, concerns, and any side effects from medications.
- By working together, we can adjust pain management plans as needed. This ensures the best comfort and recovery for our patients. Our team is dedicated to providing compassionate and thorough care during the recovery process.
Conclusion and Recommendations
A strategic timeline for pain medication administration is essential for effective pain management after colon surgery.at different ways to handle pain, like opioids and non-opioid options. We also talked about patient-controlled analgesia.
Key Takeaways for Optimal Recovery
Good pain management is just part of getting better. We stress the need for follow-up care. This helps patients get the right support and advice as they heal.
This way, patients can reach their recovery goals and live better lives.
Importance of Ongoing Care
Follow-up care is vital for checking on patients, solving problems, and tweaking pain plans. We aim to give our patients top-notch care and support. This ensures they get the best results.
By focusing on pain management and follow-up, we help patients feel more confident in their recovery. This boosts their quality of life.
FAQ
Q: What types of pain medications are commonly used after colon surgery?
A: We use opioids, NSAIDs, and acetaminophen to manage pain after colon surgery. The choice and amount depend on the patient and their pain level.
Q: How do I manage side effects of pain medications?
A: Side effects like nausea, constipation, and drowsiness are common. Stay hydrated, follow your medication schedule, and talk to your doctor to feel better.
Q: What is Patient-Controlled Analgesia (PCA) and how does it work?
A: PCA lets patients control their pain by giving themselves medication. It uses a machine to deliver medication through an IV, providing quick relief.
Q: How long will I need to take pain medications after colon surgery?
A: How long you’ll need pain meds depends on your recovery and surgery type. We switch from IV to oral meds in a few days and gradually stop them as your pain lessens.
Q: What are the benefits of non-opioid pain medications?
A: Non-opioid meds like NSAIDs and acetaminophen help manage pain without the risks of opioids. They’re often used with other methods for best results.
Q: How can I ensure effective pain management after colon surgery?
A: Good pain management comes from talking to your doctor, following their plan, and reporting any changes. Having support for daily tasks and emotional needs is also key.
Q: What are the risks associated with opioid use after surgery?
A: Opioids can lead to addiction, breathing problems, and constipation. We carefully prescribe them, using the least amount needed for the shortest time, and watch for any complications.
Q: Can I take pre-operative medications for pain management after colon surgery?
A: We review your pre-surgery pain meds and adjust them as needed for post-surgery pain. Some meds might need to be changed or stopped to avoid bad interactions.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/36453199/





