Hematopoietic stem cell transplantation has changed the game for treating serious blood diseases. It gives a second chance to thousands around the world. We’re seeing big steps forward in stem cell therapy, making it easier to find donors and improving treatment plans.Who needs stem cell therapy? Discover the proven candidates and conditions that benefit most from hematopoietic stem cell transplants.
People with certain types of leukemia, lymphoma, or blood diseases find hope in hematopoietic stem cell transplant. Stories like Marine Corps Veteran Keith Cody’s successful bloodless autologous stem cell transplant show how this treatment can change lives.
Key Takeaways
- Hematopoietic stem cell transplantation treats life-threatening blood disorders.
- Advancements in stem cell therapy are improving treatment outcomes.
- Expanded donor access is key for successful transplants.
- New treatment plans are making patient care better.
- Real-life stories show the big impact of this treatment.
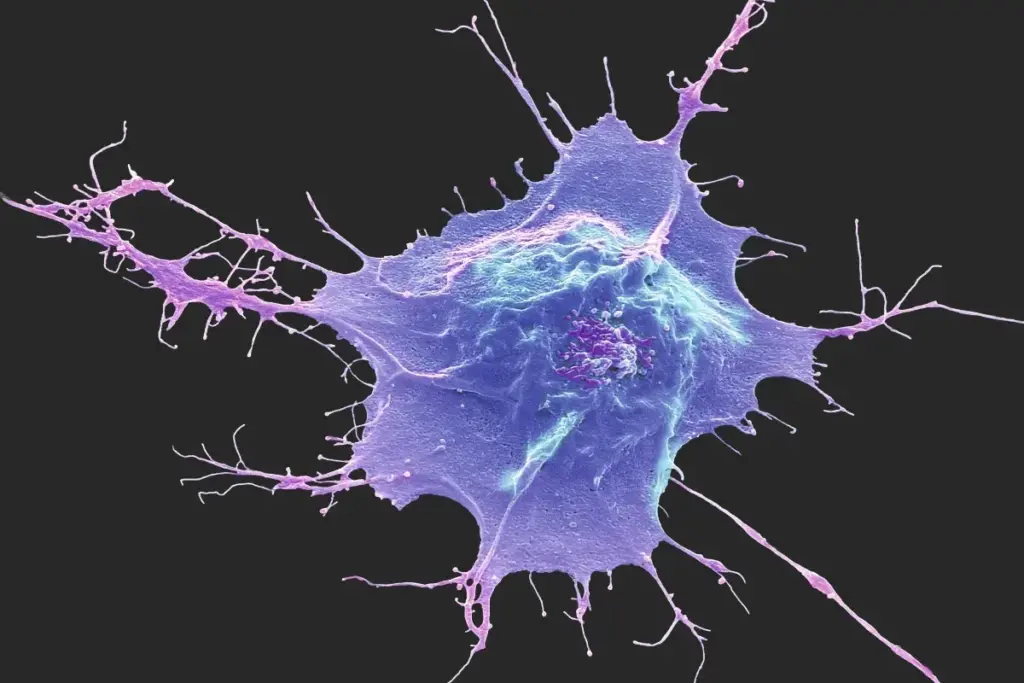
Understanding hematopoietic stem cells and their function
Hematopoietic stem cells are at the heart of our blood-making process. They can turn into different types of blood cells. These cells are key to our health, helping make the blood parts we need for our body’s functions.
What are Hematopoietic Stem Cells?
Hematopoietic stem cells live in our bone marrow. They can grow more of themselves and turn into all blood cell types. This makes them vital for keeping our blood cell supply up.
How These Cells Create Blood Components
Hematopoietic stem cells play a complex and vital role in producing different blood components. They turn into different cells, like red and white blood cells, and platelets. Red blood cells carry oxygen, and white blood cells help fight off infections.
The Regenerative Capacity of Blood-Forming Stem Cells
Hematopoietic stem cells have a big regenerative power. This makes them important in medical treatments. They are used in stem cell therapy for diseases like leukemia and lymphoma. This treatment can save lives.
Knowing about hematopoietic stem cells and their role is key. It helps us understand our blood-making system and new treatments. Their ability to create blood parts and heal shows how important they are for health and fighting diseases.
The evolution of hematopoietic stem cell transplantation
Hematopoietic stem cell transplantation has seen big changes, improving patient care and results. We’ve seen major steps forward, from early transplant methods to today’s advanced techniques. These changes have greatly increased patient survival and quality of life.
Pioneering Transplant Procedures
The first bone marrow transplant was done in 1968 by. This started a new chapter in hematopoietic stem cell transplantation. Early transplants were mainly for severe combined immunodeficiency and aplastic anemia.
As the field grew, so did our understanding of HLA typing and matching donors. This is key for allogeneic transplants to work. Donor registries and new bm transplantation and bmt transplantation protocols helped reach more people.
Key Scientific Breakthroughs
Several breakthroughs have shaped hematopoietic stem cell transplantation. Better immunosuppression has lowered the risk of graft-versus-host disease (GVHD). Also, new conditioning regimens have made transplants available to more people, including older patients and those with health issues.
Improvements in care, like better infection and organ toxicity management, have also boosted patient results. New therapies, like cellular immunotherapy, are showing promise in making transplants more effective.
Modern Transplantation Techniques
Today, hematopoietic stem cell transplantation is a complex field with ongoing innovations. Modern transplant procedures include haploidentical transplants and cord blood transplants. These options are great for patients who can’t find a matched donor.
Advances in graft manipulation and gene therapy are also on the rise. These advancements are opening up new possibilities for HSCT and improving success rates for patients with limited options.
In conclusion, the journey of hematopoietic stem cell transplantation has been filled with scientific and clinical breakthroughs. As we keep improving stem cell transplant methods and finding new treatments, the future looks bright. We can expect even better results and more treatment options for patients.
Types of hematopoietic stem cell transplants
Stem cell therapy has grown to include many transplant types. Each has its own benefits and things to consider. Hematopoietic stem cell transplantation (HSCT) is a flexible treatment for many blood cancers and non-cancerous conditions.
Autologous Transplants: Using Your Own Stem Cells
Autologous transplants use your own stem cells. They’re often used for some lymphomas and multiple myeloma. First, your stem cells are taken, stored, and then put back after a treatment.
Benefits of Autologous Transplants:
- Less chance of graft-versus-host disease (GVHD)
- Quicker recovery
- They’re cheaper than allogeneic transplants
Allogeneic Transplants: Using Donor Stem Cells
Allogeneic transplants use stem cells from a donor. They’re good for some leukemias or genetic disorders. The donor can be a relative or someone else.
Considerations for Allogeneic Transplants:
- Higher risk of GVHD
- Need for a matching donor
- Potential for fighting cancer
In 2023, about 43% of transplants were allogeneic, and 57% were autologous. This shows autologous transplants are often chosen, but allogeneic are key for some conditions.
Haploidentical Transplants
Haploidentical transplants use donors who are half-matched, usually a family member. They’re great when a full match isn’t available.
Advantages of Haploidentical Transplants:
- More donors available
- Donors can be found quickly
- May fight cancer
Cord Blood Transplants
Cord blood transplants use stem cells from umbilical cord blood. They’re good for kids and some adults with few donor options.
Benefits of Cord Blood Transplants:
- Quick access to cord blood units
- Lower GVHD risk
- Good for many patients
|
Type of Transplant |
Donor Source |
GVHD Risk |
Typical Use |
|---|---|---|---|
|
Autologous |
Patient’s own cells |
Low |
Multiple myeloma, lymphomas |
|
Allogeneic |
Related or unrelated donor |
High |
Leukemias, genetic disorders |
|
Haploidentical |
Half-matched family member |
Moderate |
Patients without a fully matched donor |
|
Cord Blood |
Umbilical cord blood |
Low |
Pediatric patients, some adult patients |
Understanding the different types of hematopoietic stem cell transplants is key. It helps in making the best treatment choices.
“The diversity in hematopoietic stem cell transplants reflects the ongoing advancements in medical science and patient care.”
Blood cancers requiring stem cell therapy
Several types of blood cancers can benefit from stem cell therapy. This offers new hope to patients. Stem cell transplantation is now a key treatment for many blood cancers.
Acute Myeloid and Lymphoblastic Leukemias
Acute myeloid leukemia (AML) and acute lymphoblastic leukemia (ALL) are aggressive blood cancers. They can be treated with stem cell therapy. AML affects the myeloid cells, while ALL impacts the lymphoid cells. Both need quick treatment, and stem cell transplantation is often effective.
Chronic Myeloid and Lymphocytic Leukemias
Chronic myeloid leukemia (CML) and chronic lymphocytic leukemia (CLL) are slower-progressing blood cancers. CML is about uncontrolled growth of myeloid cells, and CLL affects lymphoid cells. For advanced or refractory disease, stem cell therapy is considered.
Hodgkin and Non-Hodgkin Lymphomas
Lymphomas are cancers of the lymphatic system. Hodgkin lymphoma is known for Reed-Sternberg cells, while Non-Hodgkin lymphoma is a diverse group. Stem cell transplantation is used for relapsed or refractory lymphomas.
Multiple Myeloma
Multiple myeloma is a cancer of plasma cells. It can cause bone damage and anemia. Stem cell therapy is often used, mainly in younger patients or those with relapsed disease.
|
Blood Cancer Type |
Description |
Role of Stem Cell Therapy |
|---|---|---|
|
Acute Myeloid Leukemia (AML) |
Aggressive cancer affecting myeloid cells |
Treatment for eligible patients, specially with high-risk disease |
|
Acute Lymphoblastic Leukemia (ALL) |
Aggressive cancer affecting lymphoid cells |
Effective treatment option, mainly for those with high-risk features |
|
Chronic Myeloid Leukemia (CML) |
Slower-progressing cancer affecting myeloid cells |
Considered for advanced or refractory disease |
|
Multiple Myeloma |
Cancer of plasma cells |
Often used, mainly in younger patients or those with relapsed disease |
Stem cell therapy has changed how we treat blood cancers. It offers a chance for cure for patients with these tough conditions.
Non-malignant conditions eligible for transplantation
HSCT is not just for cancer. It also helps those with severe, non-cancerous disorders. These conditions can really hurt a person’s quality of life. We’ll see how HSCT can be a game-changer for these conditions.
Aplastic anemia and bone marrow failure
Aplastic anemia means the bone marrow can’t make blood cells. This leads to infections, anemia, and bleeding problems. HSCT can cure it by replacing the bad bone marrow with good stem cells.
Primary immunodeficiency disorders
These disorders make it hard for the immune system to fight off infections. Patients often get sick easily and may have autoimmune issues. HSCT can fix this by giving them a new immune system.
Inherited metabolic disorders
These genetic disorders mess up how the body breaks down substances. This can harm organs over time. HSCT can give the body new cells that can handle these substances right, stopping the damage.
Hemoglobinopathies: Sickle cell disease and thalassemia
Hemoglobinopathies affect how the body makes hemoglobin. They cause anemia, pain, and organ damage. HSCT can cure it by replacing the bone marrow with healthy cells.
HSCT is not just for cancer. It can also help with many non-cancerous conditions. Knowing the benefits and risks helps patients and doctors choose the best treatment.
Patient selection criteria for HSCT
Choosing the right patients for HSCT is complex. We look at age, how well a patient can function, and the disease’s stage. These factors help us decide if a patient is a good candidate for the treatment.
Age and Physiological Considerations
Age is key when picking patients for HSCT. But, we also look at their overall health. This includes any other health issues they might have.
This means managing any health problems that could affect the transplant’s success.
Performance Status Evaluation
How well a patient can function is also important. We use scales like the Karnofsky Performance Status (KPS) or the Eastern Cooperative Oncology Group (ECOG) to check this. These scales help us see how well a patient can handle daily activities.
|
Performance Status Scale |
Description |
Score |
|---|---|---|
|
Karnofsky Performance Status (KPS) |
Normal activity with some symptoms |
80-100% |
|
Eastern Cooperative Oncology Group (ECOG) |
Restricted activity but able to work |
0-1 |
Disease Stage and Risk Stratification
The disease’s stage and risk level are also important. We check how severe the disease is and how likely it is to get worse. This helps us decide if HSCT is the best treatment option.
“The disease stage and risk stratification play a critical role in determining a patient’s suitability for HSCT,” says an expert in the field.
Psychosocial Assessment Factors
Psychosocial assessment is also a big part of choosing patients. We look at their mental health, support system, and if they can follow post-transplant care instructions.
By carefully looking at these factors, we make sure patients get the best care. This helps them have the best possible results after HSCT.
Global statistics on stem cell transplantation
The world of stem cell transplantation is changing fast. Global numbers show its growing importance. Looking at hematopoietic stem cell transplantation (HSCT), we see it’s becoming more common in medicine.
Current Transplant Volumes Worldwide
In 2023, over 47,700 HSCTs were done globally. This is a big step forward in stem cell therapy. It shows HSCT is being used more to treat blood diseases.
Distribution Between Autologous and Allogeneic Procedures
There’s a shift in transplant types. Autologous transplants are more common, but allogeneic ones are growing. They’re used for genetic disorders and to fight cancer.
This change shows progress in matching donors and improving treatments.
Pediatric Transplant Statistics
In 2023, over 5,400 pediatric transplants were done. This highlights HSCT’s role in treating kids with serious blood diseases. It shows how far pediatric care and transplant tech have come.
Regional Differences in Transplant Access
Access to HSCT varies worldwide. Some places have good transplant programs, but others face big challenges. These include money issues, lack of facilities, and donor registry access.
Let’s look at where HSCT centers and transplants are most common:
|
Region |
Number of Transplants |
Percentage of Global Total |
|---|---|---|
|
North America |
15,000 |
31.4% |
|
Europe |
13,500 |
28.3% |
|
Asia Pacific |
10,200 |
21.4% |
|
Latin America |
4,500 |
9.4% |
|
Other Regions |
4,500 |
9.4% |
As we move forward in stem cell transplantation, it’s key to understand these global numbers. They help us see where we can do better and make this treatment available to more people.
The donor matching and selection process
Donor matching is a complex process. It ensures the donor and recipient are compatible. This is key for the success of hematopoietic stem cell transplantation.
HLA Typing and Compatibility Assessment
Human Leukocyte Antigen (HLA) typing is vital in donor matching. HLA typing checks the genetic markers on white blood cells. It helps see if the donor and recipient are compatible.
- HLA-A, HLA-B, and HLA-Medical Expert.
- High-resolution HLA typing gives detailed genetic information.
- It helps predict the risk of graft-versus-host disease (GVHD).
Finding Matched Related Donors
Related donors, like siblings, are often the first choice. They have a better chance of being a close match. We check family members to find a suitable donor.
- Siblings have a 25% chance of being a match.
- Parents are usually haploidentical, sharing half of their HLA genes with their children.
- Family members undergo HLA typing to see if they’re compatible.
Navigating Unrelated Donor Registries
When a related donor isn’t available, we look at unrelated donor registries. These registries help find a matched donor.
- Registries like the National Marrow Donor Program (NMDP) offer a wide range of donors.
- Donor searches are done worldwide to find the best match.
- Registries help contact and test possible donors.
Alternative Donor Strategies
In cases where a fully matched donor isn’t found, we consider alternative strategies. These include haploidentical donors and cord blood units.
- Haploidentical donors, often family members, are a good option.
- Cord blood units are another choice, great for pediatric patients.
- These alternatives have grown the donor pool, increasing match chances.
Understanding the donor matching and selection process shows its complexity and importance. It helps us see why finding a compatible donor is so critical for successful hematopoietic stem cell transplantation.
Donor registries and stem cell sources
Hematopoietic stem cell transplantation relies on finding compatible donors. We must explore the different registries and sources for these transplants. This is key to saving lives.
Bone Marrow Donor Registries Worldwide
Bone marrow donor registries are key for finding donors. More than 9.4 million adults are registered in the U.S. This increases the chances of finding a match for patients. These registries work globally to offer more donors.
Peripheral Blood Stem Cell Collection
Peripheral blood stem cell collection is a common method. It moves stem cells from the bone marrow to the blood. This method is less invasive than traditional bone marrow harvesting.
Cord Blood Banking Networks
Cord blood banking networks are another important source. With over 246,500 cord blood units available, they are vital for quick transplants. Cord blood stem cells are more flexible, helping patients from different backgrounds.
Expanding Donor Diversity Initiatives
Increasing donor diversity is a big challenge. Efforts to diversify donor registries are essential. There’s a push to recruit donors from underrepresented groups. This expands the donor pool and saves more lives.
In conclusion, the world of donor registries and stem cell sources is vast and changing. By supporting these efforts, we can ensure more patients get the transplants they need.
The complete stem cell transplant procedure
Getting a hematopoietic stem cell transplant needs careful planning and checks. This detailed process has several key steps that we will explain.
Pre-transplant Evaluation and Workup
Before the transplant, patients get a full check-up to see if they’re ready. This includes many tests to find any risks. Our team makes sure patients are well-prepared for the transplant.
The pre-transplant workup includes:
- Medical history review
- Physical examination
- Laboratory tests (blood counts, chemistry profiles)
- Imaging studies (X-rays, CT scans)
- Cardiac evaluation (echocardiogram, ECG)
Conditioning Regimen Options
The conditioning regimen is key to the transplant. It gets rid of the old bone marrow and immune system for new stem cells. The right conditioning depends on the patient’s disease, age, and health.
There are different conditioning regimens, such as:
- Myeloablative conditioning
- Reduced-intensity conditioning
- Non-myeloablative conditioning
Stem Cell Collection Methods
Stem cells can come from bone marrow, blood, or cord blood. The choice depends on the transplant type and the patient’s or donor’s health.
Peripheral blood stem cell collection is common. It moves stem cells from bone marrow to blood and then collects them.
The Infusion Process
The stem cell infusion is like a blood transfusion. It goes through a central venous catheter into the bloodstream.
Patients are watched closely during and after infusion for any bad reactions. The stem cells then go to the bone marrow to make new blood cells.
Special considerations in pediatric transplantation
Children getting HSCT need a special plan because their bodies are growing and changing. In 2023, over 5,400 kids got transplants worldwide. This shows how important it is for young people.
Age-Specific Challenges and Protocols
Kids getting HSCT face special challenges. These include how their bodies process drugs, risks to their organs, and the need for special treatment plans. We must think about these things when making treatment plans.
- Adjusting drug dosages based on age and weight
- Monitoring for organ toxicity and managing risks
- Tailoring conditioning regimens to minimize long-term effects
Growth and Developmental Impacts
HSCT can affect how kids grow and develop. We need to think about how it might impact their physical growth, hormone levels, and brain function. It’s important to keep up with their growth and development over time.
Key considerations include:
- Monitoring growth and development milestones
- Assessing endocrine function and managing deficiencies
- Supporting cognitive and educational needs
Family Support Requirements
HSCT is hard not just for the child but for their family too. It’s important to offer support like counseling, financial help, and educational resources. This helps them through the tough times.
Family support encompasses:
- Psychological counseling for the child and family members
- Financial assistance programs to help with treatment costs
- Educational resources on HSCT and post-transplant care
Long-Term Follow-Up in Children
It’s very important to keep up with kids who have had HSCT over time. This means watching for any late effects, managing ongoing health issues, and making sure they’re doing well overall.
- Regular monitoring for late effects of HSCT
- Managing chronic health issues related to the transplant
- Supporting the child’s overall well-being and quality of life
Survival rates and transplant outcomes
Hematopoietic stem cell transplantation has seen big improvements in survival rates and patient outcomes. As medical tech and treatment methods get better, it’s key to know what makes a transplant successful. This is important for patients, doctors, and researchers.
Current Survival Statistics
Recent studies show one-year survival rates after transplant can be as high as 84%. This boost in survival is thanks to better donor matching, treatment plans, and care after transplant. We keep watching these numbers to learn more about HSCT long-term results.
Factors Affecting Transplant Success
Many things can affect how well a transplant works. These include the patient’s health, the disease stage, donor match, and treatment plan. Also, the transplant team’s skill and post-transplant care are very important.
Knowing these factors helps us make treatment plans that fit each patient. This way, we can increase their chances of a successful transplant.
Quality of Life Considerations
Survival rates are just part of the story. How well a patient feels after transplant is also key. Many patients see big improvements in their life quality after HSCT. They can do normal or almost normal things again. But, some might face issues like GVHD or other long-term problems.
We help patients deal with these issues and improve their overall health.
Measuring Long-term Outcomes
It’s vital to follow up with patients over time to see how well the transplant worked. This means keeping an eye on their health, handling any problems, and giving support when needed. By tracking these outcomes, we can make our treatments even better.
We’re dedicated to giving our patients the best care. This care goes beyond the transplant, helping them live a healthy and fulfilling life afterwards.
Complications and management strategies
HSCT is a lifesaving treatment but comes with complications. It’s a complex process that can lead to various issues after the transplant.
Acute and Chronic Graft-Versus-Host Disease
Graft-versus-host disease (GVHD) is a big problem with allogeneic HSCT. It happens when the donor’s immune cells attack the recipient’s body. Acute GVHD shows up within 100 days, causing skin issues, liver problems, or stomach problems. Chronic GVHD can happen months or years later, affecting many organs and causing long-term health issues.
To manage GVHD, doctors use immunosuppressive drugs, choose donors carefully, and try new treatments like CAR T-cell therapy. This therapy might help with GVHD and improve the graft-versus-tumor effect.
Infection Prevention and Treatment
Infections are a big worry after HSCT because the treatment weakens the immune system. To prevent infections, doctors use antibiotics, vaccines, and good hygiene. It’s important to watch for infection signs and treat them quickly with the right medicines.
Organ Toxicity Management
The treatment can harm vital organs like the liver, lungs, and heart. Managing this damage means checking the patient’s health before the transplant, choosing gentler treatments, and watching them closely after. It’s also key to manage symptoms and prevent more damage.
Long-term Health Monitoring
Keeping an eye on health long-term is critical for HSCT patients. They need regular check-ups to catch late transplant effects like cancer, hormone problems, and mental health issues. Survivorship care plans help find and manage these problems early, improving life quality.
Advancements expanding access to stem cell therapy
The field of stem cell therapy is seeing big changes. New ways to match donors and safer treatment plans are key. These steps help patients get better and more people can get stem cell transplants.
Novel Donor Matching Approaches
New studies show better donor matching is making HSCT more successful. points to more people getting transplants. Advanced HLA typing helps match donors and recipients better.
New algorithms are also being developed. They predict transplant success based on donor and recipient traits. This helps doctors choose the best donor.
Haploidentical Transplant Innovations
Haploidentical transplants use a family member as a donor. These transplants are becoming more common. The focus is on lowering GVHD risk and improving survival rates.
Our team is leading in these advancements. We use new techniques to remove T-cells from the donor graft. This has shown great promise in trials.
Gene Therapy Integration
Gene therapy is a new tool in stem cell therapy. It can fix genetic disorders by changing stem cells. This is a big hope for patients with genetic diseases.
We’re working with researchers to add gene therapy to our HSCT programs. This gives new hope to patients with no other options.
Reduced Toxicity Protocols
HSCT’s biggest challenge is its toxicity. New protocols are less harmful but just as effective. Our team is working on these protocols to improve patient care.
We aim to give our patients the best care with fewer side effects. This is our commitment.
|
Advancement |
Description |
Benefit |
|---|---|---|
|
Novel Donor Matching Approaches |
Advanced HLA typing and predictive algorithms |
Improved transplant success rates |
|
Haploidentical Transplant Innovations |
T-cell depletion techniques |
Reduced risk of GVHD |
|
Gene Therapy Integration |
Genetic modification of stem cells |
Potential cure for genetic disorders |
|
Reduced Toxicity Protocols |
Less harmful conditioning regimens |
Minimal side effects for patients |
Conclusion: The future landscape of stem cell transplantation
Hematopoietic stem cell transplantation has come a long way. Researchers are now looking into new ways to make this therapy even better. This includes growing organs in labs and changing genes to help patients.
New ways to match donors and use gene therapy are on the horizon. These changes will make stem cell therapy more accessible. Also, new methods to reduce side effects are being developed. This will help patients have better lives after their treatment.
The future of stem cell transplantation looks very promising. With ongoing research, we can expect big improvements. We’re dedicated to providing top-notch healthcare to patients from around the world. By staying ahead in stem cell therapy, we aim to give the best care possible.
FAQ
What is a hematopoietic stem cell transplant?
A hematopoietic stem cell transplant replaces a patient’s damaged stem cells with healthy ones. This can be from the patient themselves (autologous) or a donor (allogeneic).
What conditions are treated with hematopoietic stem cell transplantation?
This treatment is for blood cancers like leukemia and lymphoma. It also treats non-malignant conditions such as aplastic anemia and primary immunodeficiency disorders.
How are donors matched for stem cell transplants?
Donors are matched by Human Leukocyte Antigen (HLA) typing. This checks if the donor’s and recipient’s immune systems are compatible. Various strategies are used to find a good match.
What are the different types of stem cell transplants?
There are several types. Autologous uses the patient’s own stem cells. Allogeneic uses donor stem cells. Haploidentical uses stem cells from a partially matched family member. Cord blood transplants use stem cells from umbilical cord blood.
What is the significance of donor diversity in stem cell transplantation?
A diverse donor pool is key for finding matches, mainly for patients from ethnic minority groups. Efforts to increase diversity aim to help patients worldwide find suitable donors.
What are the possible complications of hematopoietic stem cell transplantation?
Complications include graft-versus-host disease and infections. Organ toxicity and long-term health issues are also risks. Strategies to manage these include infection prevention and long-term health monitoring.
How have advancements in stem cell therapy improved patient outcomes?
Advances like new donor matching and gene therapy have improved outcomes. These changes have also made stem cell therapy more accessible to more patients.
What is the role of cord blood in stem cell transplantation?
Cord blood is a valuable source of stem cells. It’s a good option for patients without a matched donor. Cord blood transplants can cure various blood disorders.
What are the considerations for pediatric patients undergoing hematopoietic stem cell transplantation?
Pediatric patients face unique challenges. These include age-specific issues and impacts on growth and development. Family support and long-term care are also important.
What are the current survival rates for patients undergoing hematopoietic stem cell transplantation?
Survival rates depend on disease type, stage, and donor match. Ongoing monitoring of these factors aims to improve outcomes for patients.
What is the future of hematopoietic stem cell transplantation?
The future looks promising with ongoing research. Advances like improved donor matching and gene therapy will lead to better outcomes. This will make the treatment more accessible to more patients.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC4830270/