Last Updated on November 13, 2025 by Ilayda Cengizhan

Type 1 diabetes affects millions worldwide and is getting more common every year. Current treatments have their limits. This makes finding innovative solutions very important. Stem cell therapies are showing great promise.
Stem cell research is bringing exciting results. Some clinical trials have seen up to 80% success rates in certain groups. This breakthrough could lead to new cures and better care for patients. Places like Liv Hospital are leading this research, pushing for advanced treatments.
We’re heading towards a brighter future for those with type 1 diabetes. Stem cell therapy is a ray of hope. As research continues, we’ll see big changes in managing this condition.
Key Takeaways
- Stem cell therapy is emerging as a promising treatment for type 1 diabetes.
- Clinical trials have shown significant success rates with stem cell research.
- Innovative centers are leading the charge in stem cell therapy advancements.
- Potential cures and improved patient outcomes are on the horizon.
- Transformative changes in type 1 diabetes management are expected.
The Global Impact of Type 1 Diabetes

Type 1 diabetes is becoming more common, and it’s important to understand its effects. It’s an autoimmune disease where the body attacks and destroys the cells that make insulin in the pancreas.
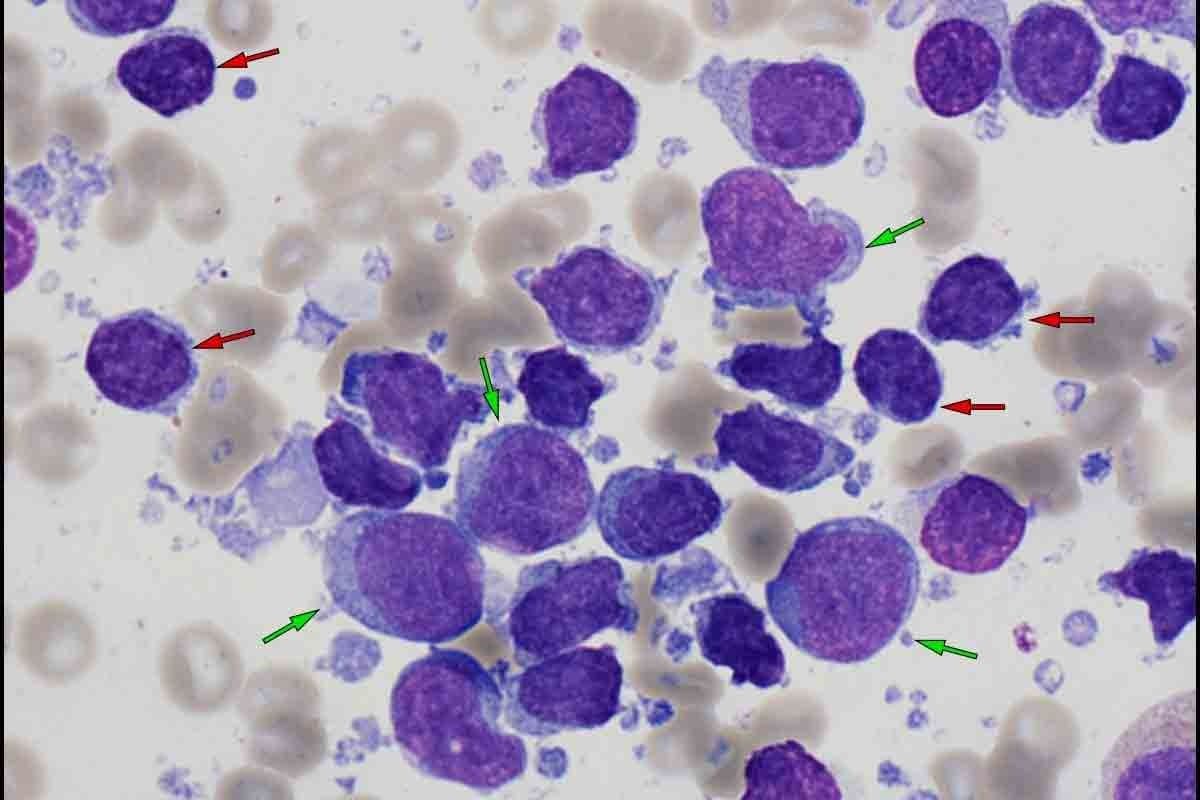
Autoimmune Destruction of Pancreatic Beta Cells
The process of destroying these cells is complex. It involves genetics and environmental factors. This results in a need for lifelong insulin therapy because the body can’t make insulin anymore. The loss of these cells is permanent, making managing type 1 diabetes very hard.
Rising Incidence: 8.7+ Million People Affected Worldwide
More and more people are getting type 1 diabetes, with over 8.7 million affected now. This increase is seen in all age groups, but it’s most noticeable in kids and teens. The table below shows how common it is in different areas.
| Region | Estimated Cases (in millions) |
|---|---|
| North America | 2.5 |
| Europe | 3.2 |
| Asia-Pacific | 2.0 |
| Other regions | 1.0 |
Limitations and Challenges of Lifelong Insulin Dependency
Being dependent on insulin for life is a big challenge. It can lead to low blood sugar, blood sugar swings, and serious long-term problems like nerve damage and eye issues. New treatments, including stem cell therapies, are being looked into to help manage these issues and improve life for those with type 1 diabetes.
Stem Cell Therapy: A Revolutionary Approach to Diabetes 1 New Treatment

Stem cell therapy is a new hope for type 1 diabetes patients. It aims to fix the disease’s root cause, not just its symptoms.
Understanding the Potential of Stem Cells in Diabetes
Stem cells can turn into different cell types. This makes them great for growing new pancreatic beta cells in type 1 diabetes. Researchers are looking into two main types of stem cells:
Mesenchymal Stem Cells (MSCs)
MSCs help with tissue repair and can calm down the immune system. They might help stop the body from attacking pancreatic beta cells.
Pluripotent Stem Cells
Pluripotent stem cells, like iPSCs, can become any cell type. This includes insulin-making beta cells. They’re very promising for fixing damaged pancreatic cells.
Clinical Success Rates: Up to 80% in Select Patient Cohorts
Recent studies show up to 80% success in some patients. These successes mean better blood sugar control and less need for insulin.
Addressing the Root Cause vs. Symptom Management
Stem cell therapy is different from usual treatments. It tries to fix the disease’s cause by growing new beta cells or changing the immune system.
Advance #1: Mesenchymal Stem Cells for Immune Modulation
Mesenchymal stem cells are showing great promise in treating type 1 diabetes. They help control the immune system, which is key in fighting the disease. This approach is changing how we treat type 1 diabetes, focusing on saving pancreatic beta cells.
How MSCs Regulate Autoimmune Responses in Type 1 Diabetes
Mesenchymal stem cells (MSCs) play a big role in managing autoimmune responses. They do this by controlling the immune system’s strength. This includes stopping T-cells from growing and boosting the number of regulatory T-cells.
Promoting Beta Cell Regeneration and Protection
MSCs also help in growing and protecting beta cells. This is important for making insulin naturally again. It’s a two-part action that helps the body’s insulin-making ability.
Clinical Evidence of Improved Glycemic Control
Studies show MSCs can improve blood sugar control in type 1 diabetes patients. This is because they can control the immune system and protect beta cells.
Safety Profile Compared to Traditional Immunosuppression
Using MSCs is safer than traditional treatments. They target the immune system more precisely, which means fewer side effects.
Long-term Outcomes in Recent Studies
Recent studies are showing good results with MSCs in treating type 1 diabetes. Here are some key findings:
| Study | Duration | Outcome |
|---|---|---|
| Study A | 12 months | Improved glycemic control |
| Study B | 24 months | Reduced insulin dependency |
Advance #2: Pluripotent Stem Cell-Derived Islet Replacement
Pluripotent stem cells are a big step towards curing type 1 diabetes. These cells can turn into any cell type. This means they can make islet cells that produce insulin.
Engineering Functional Beta Cells from Stem Cells
We’re getting better at making beta cells from stem cells. Beta cells can control blood sugar levels. This could help people with type 1 diabetes manage their sugar better.
Transplantation Methods and Site Selection
How we transplant islet cells and where we put them matters a lot. Scientists are looking into new ways to do this. They want to use special materials to help the cells work better.
Overcoming Challenges in Cell Survival and Function
There are hurdles to overcome with islet cell transplants. We need to make sure the cells survive and work well. To do this, we’re looking at ways to improve blood flow and protect against the immune system.
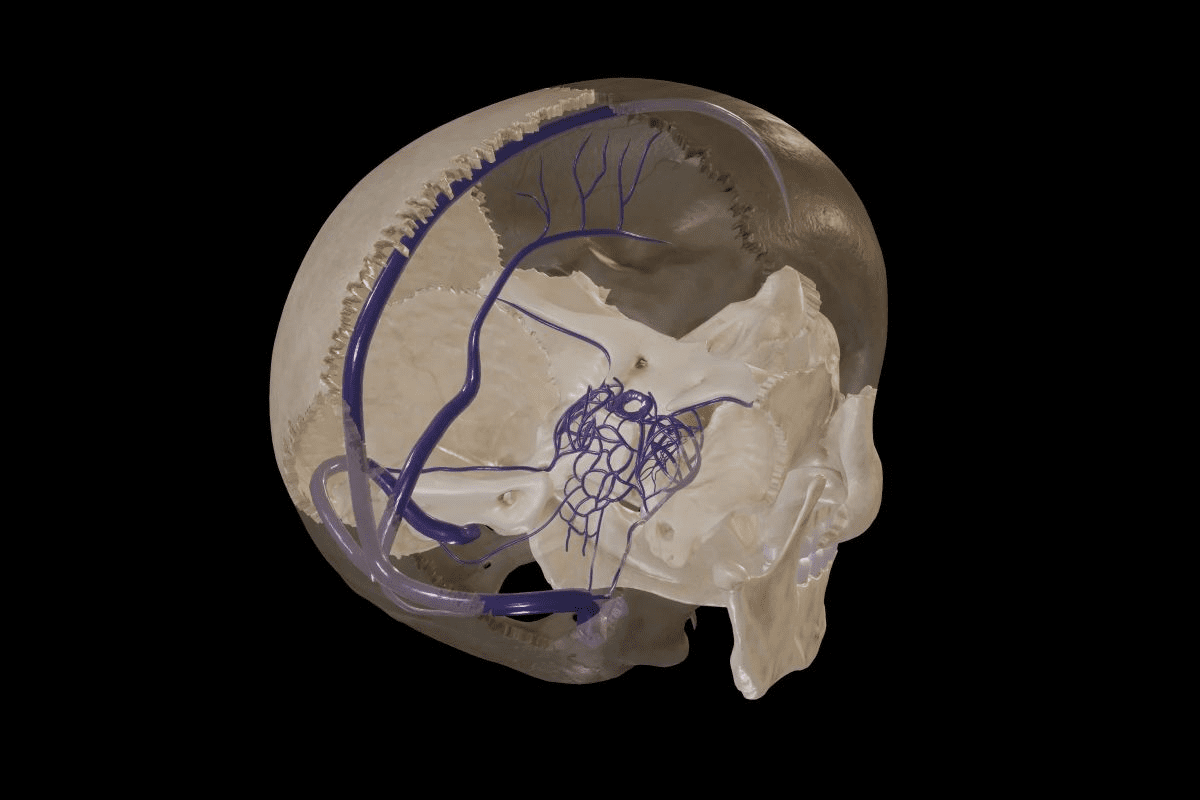
Vascularization Strategies
Good blood flow is key for islet cell survival. We’re working on ways to make more blood vessels around the cells. This is important for their health and function.
Preventing Recurrent Autoimmunity
Another big challenge is stopping the immune system from attacking the new cells. Scientists are exploring ways to keep the cells safe. This could involve using treatments that calm down the immune system.
| Strategy | Description | Potential Benefit |
|---|---|---|
| Vascularization Enhancement | Improving blood vessel formation around transplanted islet cells | Enhanced cell survival and function |
| Immunomodulation | Modulating the immune system to prevent attack on transplanted cells | Reduced risk of recurrent autoimmunity |
Advance #3: VX-880 Therapy and Endogenous Insulin Restoration
VX-880 therapy is leading the way in stem cell treatments. It aims to bring back insulin making in type 1 diabetes patients. Early trials look promising, giving hope to those with this chronic disease.
The Science and Mechanism Behind VX-880
VX-880 therapy uses stem cells to fix or replace insulin-making cells in the pancreas. This method attacks the core of type 1 diabetes, possibly making external insulin unnecessary.
Breakthrough Clinical Results in Human Trials
Clinical trials with VX-880 therapy have seen major breakthroughs. Patients have better blood sugar control and need less external insulin. These findings are key in the fight to better manage type 1 diabetes.
Patient Outcomes: Reduced Need for Exogenous Insulin
The main advantage of VX-880 therapy is it helps make insulin again. This means patients need less external insulin, improving their lives.
Case Studies of Successful Treatment
Many case studies show VX-880 therapy’s success. For example, one patient’s HbA1c levels dropped a lot, and insulin needs fell significantly.
“The results from the VX-880 therapy trials are encouraging, indicating a possible change in how we treat type 1 diabetes,” said a leading researcher in the field.
- Improved glycemic control
- Reduced need for exogenous insulin
- Enhanced patient quality of life
Advance #4: Off-the-Shelf Stem Cell Approaches
Off-the-shelf stem cell methods are a big step forward in treating type 1 diabetes. These methods use stem cells from donors. This way, they can help many patients, unlike treatments made just for one person.
Allogeneic Stem Cell Products: Advantages and Challenges
Allogeneic stem cell products are cheaper and easier to get than treatments made just for one person. But, they might cause the body to reject them. Also, patients might need to take drugs to stop their immune system from fighting the cells.
“Using off-the-shelf stem cells could make stem cell treatments for type 1 diabetes more available and affordable,” studies say.
The Landmark Phase 1/2 Study Results
A major study showed how well off-the-shelf stem cell treatments work for type 1 diabetes. The study found that 10 out of 12 patients stopped needing insulin. This shows that stem cells from donors could be a big help in managing type 1 diabetes.
10 out of 12 Patients Achieving Insulin Independence
The study found that 10 out of 12 patients could stop using insulin. This is a big win for treating type 1 diabetes.
Duration of Effect: Beyond One Year Without Injections
Many patients stayed off insulin for more than a year. This shows that this treatment could work for a long time.
Scaling Production for Wider Availability
To make these treatments available to more people, we need to make more of them. We also have to keep them safe and effective. Work is being done to make these treatments cheaper and easier to get for patients all over the world.
Advance #5: Encapsulation Technologies Protecting Transplanted Cells
Encapsulation technologies are key in protecting cells for type 1 diabetes treatment. They use biocompatible materials to shield cells from the immune system. This allows cells to exchange oxygen, nutrients, and therapeutic molecules.
Innovative Materials for Cell Encapsulation
Scientists are working on new materials for cell encapsulation. These include alginate-based hydrogels and synthetic polymers. These materials are safe, strong, and last a long time.
Immune Isolation Without Compromising Function
The main aim of encapsulation is to protect cells from the immune system. This is done by designing the material’s pore size. It lets essential molecules pass through while keeping immune cells out.
Enhancing Long-term Viability of Transplanted Cells
To make encapsulated cells last longer, researchers are exploring several areas. They are looking into
Oxygen and Nutrient Delivery Systems
and
Retrievability and Safety Features
. New delivery systems ensure cells get enough oxygen and nutrients. Features for safe removal are also being developed.
Advancements in encapsulation technologies are making stem cell therapies safer and more effective. This brings us closer to finding a cure for type 1 diabetes.
Advance #6: Combination Therapeutic Approaches
Research is showing that mixing different treatments can make stem cell therapy for type 1 diabetes better. This approach uses the strengths of various treatments together to get better results.
Synergistic Effects of Multiple Treatment Modalities
Using different treatments at the same time can help patients more. For example, immunomodulation and cell replacement therapy can work together. They replace damaged cells and also help the immune system not attack the new cells.
| Therapeutic Approach | Benefits |
|---|---|
| Immunomodulation | Regulates autoimmune responses, reducing damage to pancreatic cells |
| Cell Replacement Therapy | Replaces damaged or destroyed pancreatic cells, restoring insulin production |
| Adjuvant Treatments | Enhances the efficacy of stem cell therapy through anti-inflammatory agents and growth factors |
Immunomodulation Combined with Cell Replacement Therapy
One exciting mix is using immunomodulation and cell replacement therapy together. This helps the new cells to work well and live longer. Experts say, “This mix could lead to patients not needing insulin for a long time.”
“The future of type 1 diabetes treatment lies in combining different therapeutic approaches to achieve a cure.”
Adjuvant Treatments Enhancing Stem Cell Efficacy
Adjuvant treatments, like anti-inflammatory agents and growth factors, are key to making stem cell therapy work better. They help the new cells to survive and function well.
Anti-inflammatory Agents
Anti-inflammatory agents reduce inflammation at the transplant site. This helps the cells to live longer.
Growth Factors and Signaling Molecules
Growth factors and signaling molecules make the transplanted cells work better. They help control blood sugar levels.
Advance #7: Gene-Edited Stem Cells
Gene-edited stem cells are a big step forward in treating type 1 diabetes. They use new gene editing tech to make stem cell treatments better and safer.
CRISPR and Other Gene Editing Technologies in Diabetes
CRISPR and other gene editing tools are changing how we treat type 1 diabetes. CRISPR technology lets us make precise changes to the genome. This helps create stem cells that can avoid being rejected by the immune system and work better.
Creating Immune-Resistant Beta Cells
One big challenge in treating type 1 diabetes with stem cells is the immune system attacking the beta cells. Gene editing can make immune-resistant beta cells. This might mean we need less drugs to keep the immune system in check.
Enhanced Functionality Through Genetic Optimization
Gene editing does more than just protect beta cells from the immune system. It also makes them work better. By tweaking their genes, researchers hope to boost their insulin-making abilities and overall performance.
Safety Considerations and Regulatory Hurdles
Gene-edited stem cells are promising, but there are safety and regulatory issues to tackle. Making sure these treatments are safe and work well is key. This means we need to do a lot of testing and validation.
Current Research Status and Timeline to Clinical Use
Research on gene-edited stem cells for type 1 diabetes is moving forward. Many studies are showing promising results. While it’s hard to say exactly when these treatments will be available, the progress is hopeful.
Accessibility, Cost, and Future Availability
Stem cell treatments are changing how we treat Type 1 Diabetes. But, their high cost is a big problem. We need to work on making these treatments more accessible and affordable for everyone.
Current Cost Barriers to Stem Cell Treatments
The cost of stem cell treatments for Type 1 Diabetes is too high for many. High production costs and complex treatment processes make them expensive. This makes it hard for people to get this life-changing treatment, leading to unfair health outcomes.
Insurance Coverage and Healthcare Policy Evolution
As stem cell therapies grow, we need better insurance and healthcare policies. Insurance companies are starting to see the long-term benefits of these treatments. But, we need policy changes to make sure everyone can get them.
Efforts to Scale Production and Reduce Costs
To make treatments more accessible, researchers and makers are working hard. They’re trying to:
- Make manufacturing more efficient
- Use automation to save money
- Work together with public and private groups to share costs
Public-Private Partnerships
Public-private partnerships are key in moving stem cell therapies forward. They bring together resources and skills. This helps make treatments available to more people.
Patient Advocacy Initiatives
Patient groups are also very important. They help make treatments more accessible and affordable. By raising awareness and pushing for policy changes, they ensure patients’ needs are met.
Ongoing Research and Future Directions
Stem cell therapy for type 1 diabetes is getting a lot of attention. New research is leading to exciting breakthroughs. This is thanks to ongoing clinical trials and new technologies.
Current Clinical Trials to Watch
Many clinical trials are looking into stem cell therapy for type 1 diabetes. These studies are key to figuring out if stem cells can help patients.
Emerging Technologies on the Horizon
New technologies like gene editing and biomaterials are being studied. They could make stem cell therapy even better by improving how well cells work.
Integrating Stem Cell Therapy with Artificial Intelligence and Biomonitoring
Stem cell therapy is being combined with AI and biomonitoring. AI helps make treatments more personal. Biomonitoring lets doctors keep an eye on patients’ health in real time.
Personalized Treatment Approaches
Personalized medicine is a big deal in stem cell therapy. Tailoring treatments to each patient can lead to better results and fewer side effects.
Predictive Models for Patient Selection
Researchers are working on predictive models. These models use AI and patient data to figure out who will benefit most from stem cell therapy.
| Research Area | Current Status | Potential Impact |
|---|---|---|
| Stem Cell Therapy | Ongoing clinical trials | Improved glycemic control |
| Gene Editing | Emerging technology | Enhanced cell functionality |
| AI Integration | Research in progress | Personalized treatment approaches |
Conclusion
We’ve looked into the big steps forward in stem cell therapy for type 1 diabetes. This disease affects millions globally. New treatments are showing great promise, helping people control their blood sugar better and use less insulin.
Seven major advancements in stem cell therapy have been highlighted. These include mesenchymal stem cells and pluripotent stem cells. They also include gene-edited stem cells. These could help fix the damage to pancreatic beta cells caused by type 1 diabetes.
As research keeps moving forward, we’re expecting better results for those with type 1 diabetes. This could mean a better life for them. The future of stem cell therapy looks bright, and we’re excited to see what’s next.
FAQ
What is stem cell therapy for type 1 diabetes?
Stem cell therapy for type 1 diabetes is a new way to treat the disease. It uses stem cells to make insulin again and control the immune system. This could even reverse the disease.
How do mesenchymal stem cells (MSCs) help in type 1 diabetes treatment?
MSCs help by controlling the immune system and growing new beta cells. They also help manage blood sugar levels. This makes them a promising treatment for type 1 diabetes.
What are pluripotent stem cells, and how are they used in type 1 diabetes treatment?
Pluripotent stem cells can turn into different cell types, like insulin-making beta cells. They are used to make new beta cells for transplant. This could help type 1 diabetes patients make insulin again.
What is VX-880 therapy, and how does it work?
VX-880 therapy uses stem cells to make functional beta cells. These cells are then transplanted to restore insulin production. This could reduce the need for insulin shots.
What are off-the-shelf stem cell approaches, and what are their advantages?
Off-the-shelf stem cell approaches use stem cells that can be made in large quantities. These can be used for many patients. This makes treatment more accessible and affordable.
How do encapsulation technologies protect transplanted cells?
Encapsulation technologies use special materials to cover transplanted cells. This protects them from being rejected by the immune system. It also keeps them working properly.
What are combination therapeutic approaches in stem cell therapy for type 1 diabetes?
Combination therapeutic approaches use different treatments together. This includes things like controlling the immune system and replacing cells. It aims to get better results by working together.
How do gene-edited stem cells work, and what are their benefits?
Gene-edited stem cells use CRISPR to make beta cells that the immune system won’t attack. This could make the cells work better and last longer.
What are the current cost barriers to stem cell treatments for type 1 diabetes?
The main cost barriers are the high prices of making and testing stem cell treatments. Also, getting approval from regulators costs a lot. These costs make treatments hard to afford.
How is insurance coverage and healthcare policy evolving for stem cell therapies?
Insurance and healthcare policies are changing to cover more stem cell treatments. They are trying to make treatments cheaper and more available for patients.
What is the future of stem cell therapy for type 1 diabetes?
The future looks bright for stem cell therapy in type 1 diabetes. Researchers are working hard to make treatments better, cheaper, and more accessible. This could change how we treat the disease.
Are stem cell therapies for type 1 diabetes available now?
Some stem cell therapies are in clinical trials, but they’re not widely available yet. Patients should talk to their doctors to learn about current options and trials.
What are the benefits of integrating stem cell therapy with artificial intelligence and biomonitoring?
Using artificial intelligence and biomonitoring with stem cell therapy could improve results. It could help tailor treatments to each patient. This could lead to better health outcomes
References
- Harvard Stem Cell Institute (HSCI): https://www.hsci.harvard.edu/news/new-therapy-treating-type-1-diabetes
- STAT: https://www.statnews.com/2025/06/20/stem-cell-therapy-type1-diabetes-study/
- DVC Stem: https://www.dvcstem.com/post/can-stem-cells-treat-diabetes
- National Institutes of Health: https://pmc.ncbi.nlm.nih.gov/articles/PMC7778150/
- U.S. Food and Drug Administration (FDA): https://www.fda.gov/news-events/press-announcements/fda-approves-first-cellular-therapy-treat-patients-type-1-diabetes