Last Updated on December 1, 2025 by Bilal Hasdemir
Cancer treatment has changed a lot with stem cell therapy. This new method is showing great promise in fighting different cancers.
The National Cancer Institute says stem cell transplants help with blood cancers like leukemia, lymphoma, and multiple myeloma. These transplants help patients make healthy blood cells again.
Stem cell therapy is becoming more important in cancer treatment. It gives patients with these diseases new hope.
Key Takeaways
- Stem cell therapy is used to treat various types of cancers.
- Leukemia, lymphoma, and multiple myeloma are among the cancers treated with stem cell transplants.
- Stem cell transplants help restore the patient’s ability to produce healthy blood cells.
- Cancer treatment is evolving with the use of stem cell therapy.
- Stem cell therapy offers new hope to patients with blood-related cancers.
The Science Behind Stem Cell Therapy for Cancer
Stem cell therapy for cancer works by regenerating damaged tissues and boosting the immune system. This treatment, also known as regenerative medicine, is seen as a hopeful solution for many cancers.
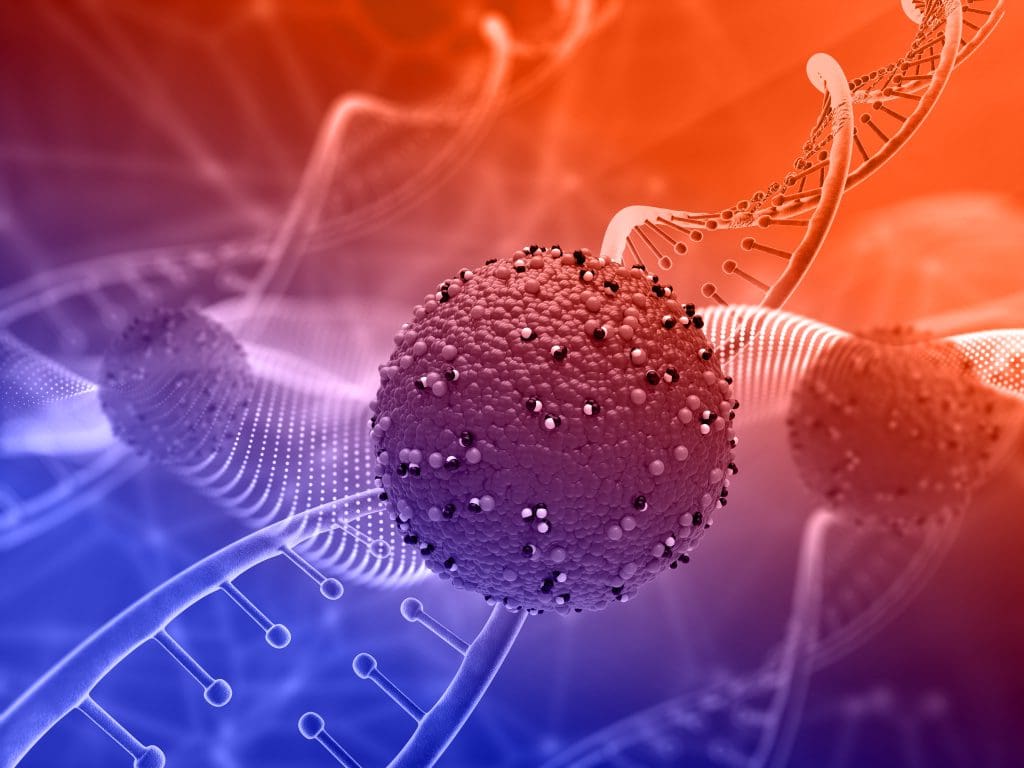
What Are Stem Cells and How They Work
Stem cells are unique because they can grow and change into different cell types. These cells can be directed to fix damaged tissues. This makes them very useful in fighting cancer.
Key characteristics of stem cells include:
- Self-renewal: The ability to maintain their numbers through cell division.
- Differentiability: The capacity to develop into specialized cell types.
The Therapeutic Potencial in Oncology
Stem cells have a big role in fighting cancer because they can target and fix damaged tissues. They can:
- Replace damaged cells with healthy ones.
- Help the immune system fight cancer better.
- Carry treatments right to the tumors.
Experts say stem cell transplantation is key in treating some blood cancers. It offers a chance for a cure for patients with hard-to-treat diseases. This shows how important stem cell therapy is in improving cancer treatment results.
Types of Stem Cell Transplants Used in Cancer Treatment
Stem cell transplants are a key part of cancer treatment. They come in four main types, based on the source of the stem cells and the donor.
Autologous Transplants: Using Your Own Cells
Autologous transplants use the patient’s own stem cells. This method is often used for cancers like multiple myeloma and certain lymphomas. First, the patient’s stem cells are harvested and stored. Then, they are reinfused after high-dose chemotherapy.
Advantages: Lower risk of graft-versus-host disease (GVHD), faster engraftment.
Disadvantages: Risk of reinfusing cancerous cells, may not be suitable for patients with certain types of cancer.
Allogeneic Transplants: Donor-Derived Cells
Allogeneic transplants use stem cells from a donor. This donor can be a sibling, an unrelated donor, or a cord blood unit. The donor’s stem cells are matched to the patient as closely as possible to minimize complications.
Advantages: Has a graft-versus-tumor effect, suitable for patients without suitable autologous cells.
Haploidentical and Cord Blood Transplants
Haploidentical transplants are a type of allogeneic transplant where the donor is a family member who is only half-matched to the patient. Cord blood transplants use stem cells from the umbilical cord blood, which can be obtained from a bank or a directed donation.
Haploidentical Advantages: Almost everyone has a haploidentical donor, often a family member.
Haploidentical Disadvantages: Higher risk of GVHD or rejection.
Cord Blood Advantages: Rapid availability, lower risk of GVHD.
Cord Blood Disadvantages: Limited cell dose, slower engraftment.
| Transplant Type | Donor Source | Advantages | Disadvantages |
| Autologous | Patient’s own cells | Lower GVHD risk, faster engraftment | Risk of reinfusing cancer cells |
| Allogeneic | Matched donor | Graft-versus-tumor effect, suitable for various cancers | GVHD risk, longer engraftment time |
| Haploidentical | Half-matched family member | Almost everyone has a donor | Higher GVHD or rejection risk |
| Cord Blood | Umbilical cord blood | Rapid availability, lower GVHD risk | Limited cell dose, slower engraftment |
The Stem Cell Transplant Procedure: Step by Step
The stem cell transplant process is complex and involves several key steps. It helps treat different types of cancers. The procedure requires careful planning, precise execution, and thorough follow-up care.
Pre-Transplant Evaluation and Conditioning
Before a stem cell transplant, patients undergo a detailed pre-transplant evaluation. This includes various tests to check their health, cancer status, and if they’re a good candidate for the transplant. The National Cancer Institute explains that the conditioning regimen is used to kill cancer cells and get the body ready for the transplant.
The conditioning regimen includes high-dose chemotherapy and/or radiation therapy. This step is vital. It kills cancer cells, makes room for new stem cells, and weakens the immune system to prevent transplant rejection.
Stem Cell Collection and Processing

Stem cells can come from the patient themselves (autologous transplant) or a donor (allogeneic transplant). The collection process takes stem cells from the bone marrow or peripheral blood. For peripheral blood stem cell collection, patients or donors may get medication to move stem cells into the bloodstream, making them easier to collect.
After collection, the stem cells are cleaned and prepared for infusion. This step is essential to ensure the stem cells are of high quality and viable.
The Transplantation Process
The actual transplant involves infusing the prepared stem cells into the patient’s bloodstream through an intravenous line. This process is similar to a blood transfusion and usually takes a few hours.
After infusion, the stem cells go to the bone marrow to start producing new blood cells. The healthcare team closely watches the patient, managing any side effects and complications that may come up.
| Step | Description | Key Considerations |
| Pre-Transplant Evaluation | Comprehensive assessment of patient’s health and cancer status | Overall health, cancer status, suitability for transplant |
| Conditioning Regimen | High-dose chemotherapy and/or radiation therapy | Eradicating cancer cells, preparing body for transplant |
| Stem Cell Collection | Harvesting stem cells from bone marrow or peripheral blood | Source of stem cells (autologous or allogeneic) |
| Stem Cell Processing | Preparing stem cells for infusion | Quality and viability of stem cells |
| Transplantation | Infusing stem cells into patient’s bloodstream | Monitoring for side effects and complications |
Leukemia: The Primary Beneficiary of Stem Cell Therapy
Stem cell therapy has changed how we treat leukemia, giving hope to those with blood cancer. Leukemia is a blood cancer with many types, like Acute Myeloid Leukemia (AML) and Acute Lymphoblastic Leukemia (ALL). This therapy has greatly improved survival rates and quality of life for many.
Acute Myeloid Leukemia (AML) Treatment
AML is a fast-growing leukemia that needs strong treatment. Often, stem cell transplants are used, either from the patient or a donor. This replaces the bad bone marrow with healthy cells.

Benefits of Stem Cell Therapy in AML:
- Potential for cure in eligible patients
- Improved survival rates compared to chemotherapy alone
- Reduced risk of relapse
Acute Lymphoblastic Leukemia (ALL) Approaches
ALL is a leukemia that also benefits from stem cell therapy. It’s more common in kids but also affects adults. High-risk patients or those who have relapsed may get a transplant.
Chronic Leukemias and Transplantation
Chronic leukemias, like CML and CLL, may also get stem cell transplants. While drugs are the main treatment for CML, transplants are an option for advanced cases.
The success of stem cell transplants in leukemia depends on many things. These include the type of leukemia, the patient’s age, and health. Here’s a table comparing different leukemias and their responses to stem cell therapy:
| Leukemia Type | Transplant Type | Survival Rate |
| AML | Allogeneic | 40-50% |
| ALL | Allogeneic | 50-60% |
| CML | Allogeneic | 60-70% |
Lymphoma Treatment with Stem Cell Transplantation
Stem cell transplantation is a promising treatment for lymphoma. Lymphoma starts in the lymph system and includes Hodgkin and non-Hodgkin types. It’s used for patients with relapsed or refractory disease.
Hodgkin Lymphoma: When Transplants Are Recommended
Hodgkin lymphoma is often treated with chemotherapy and radiation. But, some patients may need a stem cell transplant. Autologous stem cell transplantation, using the patient’s own cells, is usually recommended.
The choice to use stem cell transplantation depends on the patient’s response to treatment. Research shows it can improve survival for those with relapsed or refractory Hodgkin lymphoma.
Non-Hodgkin Lymphoma: Diffuse Large B-Cell and Other Types
Non-Hodgkin lymphoma includes many types, with diffuse large B-cell being common. For patients with relapsed or refractory disease, stem cell transplantation is considered. Both autologous and allogeneic stem cell transplantation (using donor cells) are options, based on the patient’s condition and donor availability.
| Lymphoma Type | Transplant Type | Recommendation Basis |
| Hodgkin Lymphoma | Autologous | Relapsed or Refractory Disease |
| Non-Hodgkin Lymphoma (Diffuse Large B-Cell) | Autologous/Allogeneic | Relapsed or Refractory Disease, Donor Availability |
Stem cell transplantation is a major step forward in treating lymphoma. It offers effective treatment options for patients with Hodgkin and non-Hodgkin lymphoma.
Multiple Myeloma and the Role of Stem Cell Therapy
Autologous stem cell transplantation is key in treating multiple myeloma. It helps patients live longer and better. This method uses a patient’s own stem cells to fight cancer.
Autologous Transplantation as Standard of Care
Autologous stem cell transplantation uses a patient’s stem cells. These cells are collected, stored, and then given back after treatment. This method is now a main treatment for multiple myeloma.
Benefits of Autologous Transplantation:
- Improved response rates
- Enhanced survival outcomes
- Potential for prolonged remission
Single vs. Tandem Transplants: Comparing Outcomes
Choosing between single or tandem transplants depends on many factors. These include the patient’s age, health, and the type of multiple myeloma. Tandem transplants involve two rounds of treatment a few months apart.
| Transplant Type | Survival Benefit | Toxicity Levels |
| Single Autologous Transplant | Significant improvement in overall survival | Moderate toxicity |
| Tandem Autologous Transplants | Potential for further improvement in survival, even in high-risk patients | Higher toxicity levels due to intensified treatment |
Studies show tandem transplants can help some patients more, but they are riskier. The right choice depends on the patient’s health and risk level.
In summary, stem cell transplantation is vital for treating multiple myeloma. Deciding between single or tandem transplants should be based on each patient’s needs and health.
Solid Tumors That Respond to Stem Cell Treatment
Stem cell therapy is showing promise for treating solid tumors. It’s not just for blood cancers anymore. Some solid tumors are also responding well to this treatment.
Neuroblastoma in Children
Neuroblastoma mainly hits kids. It’s been treated with stem cell transplants with good results. Kids with high-risk neuroblastoma often get these transplants.
This treatment has helped some kids live longer. It’s a hopeful sign for neuroblastoma patients.
Testicular Cancer and Germ Cell Tumors
Testicular cancer and germ cell tumors also benefit from stem cell transplants. For some, high-dose chemo followed by stem cell transplant works well.
Emerging Applications in Other Solid Cancers
Researchers are looking into stem cell therapy for other solid tumors. This includes some sarcomas and brain tumors. It’s early, but it’s a promising area.
Stem cell research is growing fast. It’s bringing new hope to cancer patients. It could lead to more treatment options.
Patient Eligibility: Who Can Receive a Stem Cell Transplant
To see if a patient can get a stem cell transplant, doctors look at their health closely. This check is key to see if the treatment will help.
Age and Health Considerations
Age matters a lot when it comes to stem cell transplants. The Canadian Cancer Society says younger people usually do better with these treatments. But, older patients can also get transplants if they’re healthy enough.
Doctors check many things to see if a patient is ready for a transplant. They look at the heart, lungs, and kidneys. They also check for other health issues.
Key Health Considerations:
- Cardiac function
- Pulmonary function
- Renal function
- Presence of comorbid conditions
Disease-Specific Eligibility Criteria
The kind and stage of cancer also matter a lot. Each cancer has its own rules for getting a transplant. These rules depend on how well the cancer responds to treatment and if there’s any cancer left.
| Disease Type | Eligibility Criteria | Transplant Type |
| Acute Myeloid Leukemia (AML) | First remission, high-risk features | Allogeneic |
| Multiple Myeloma | Newly diagnosed, after initial therapy | Autologous |
| Non-Hodgkin Lymphoma | Relapsed or refractory disease | Autologous or Allogeneic |
Choosing to do a stem cell transplant is a personal decision. It depends on the latest research and the patient’s situation.
The Recovery Process After Stem Cell Transplantation
After a stem cell transplant, patients start a long recovery. They need constant medical care. This phase is filled with challenges that must be watched closely.
The First 100 Days: Critical Recovery Period
The first 100 days are very important. Patients face a high risk of infections and graft-versus-host disease (GVHD). The National Cancer Institute says it’s key to keep a close eye on these issues.
Patients see their doctors often. They get blood tests and other checks to see how they’re doing.
Long-term Recovery and Follow-up Care
Recovery goes on for a long time. Doctors watch for late transplant effects like organ damage or new cancers. Each patient gets a care plan that fits their needs.
Having a good care plan is essential. It helps catch problems early and keeps patients healthy.
| Recovery Aspect | First 100 Days | Long-term Recovery |
| Primary Focus | Managing infections and GVHD | Monitoring for late effects and secondary cancers |
| Follow-up Care | Regular check-ups, blood tests, and diagnostic procedures | Tailored follow-up appointments with specialists |
| Patient Needs | Close medical supervision, possible hospital stays | Ongoing support for physical and emotional health |
Side Effects and Complications of Stem Cell Transplants
Stem cell transplants save many lives but have side effects and complications. These can differ a lot between patients. They depend on the transplant type, the patient’s health, and the cancer type.
Immediate Post-Transplant Complications
Right after a transplant, patients face several risks. Infections are a big worry because the immune system is weakened. Graft failure, where the stem cells don’t work, is another issue.
- Infections: Bacterial, viral, and fungal infections can occur due to immunosuppression.
- Graft failure: Failure of the graft to produce blood cells.
- Mucositis: Inflammation and ulceration of the mucous membranes.
Graft-versus-Host Disease (GVHD)
GVHD happens when the donor’s immune cells attack the host’s body. It can be acute or chronic. The acute form usually starts within 100 days after the transplant.
| GVHD Type | Time of Onset | Commonly Affected Organs |
| Acute GVHD | Within 100 days | Skin, liver, gastrointestinal tract |
| Chronic GVHD | After 100 days | Multiple organs, including skin, mouth, eyes, liver, and lungs |
Long-term Side Effects and Quality of Life
Survivors of stem cell transplants may face long-term effects. These can include chronic GVHD, infertility, and a higher risk of secondary cancers. It’s important to manage these effects to improve patients’ lives.
The Canadian Cancer Society says it’s key to understand and manage these complications. This helps improve patient care and outcomes.
Becoming a Stem Cell Donor: The Gift of Life
Stem cell donation is a chance to save lives. It helps cancer patients get better and live healthier lives. This journey has many steps and can change lives for the better.
The Donation Process Explained
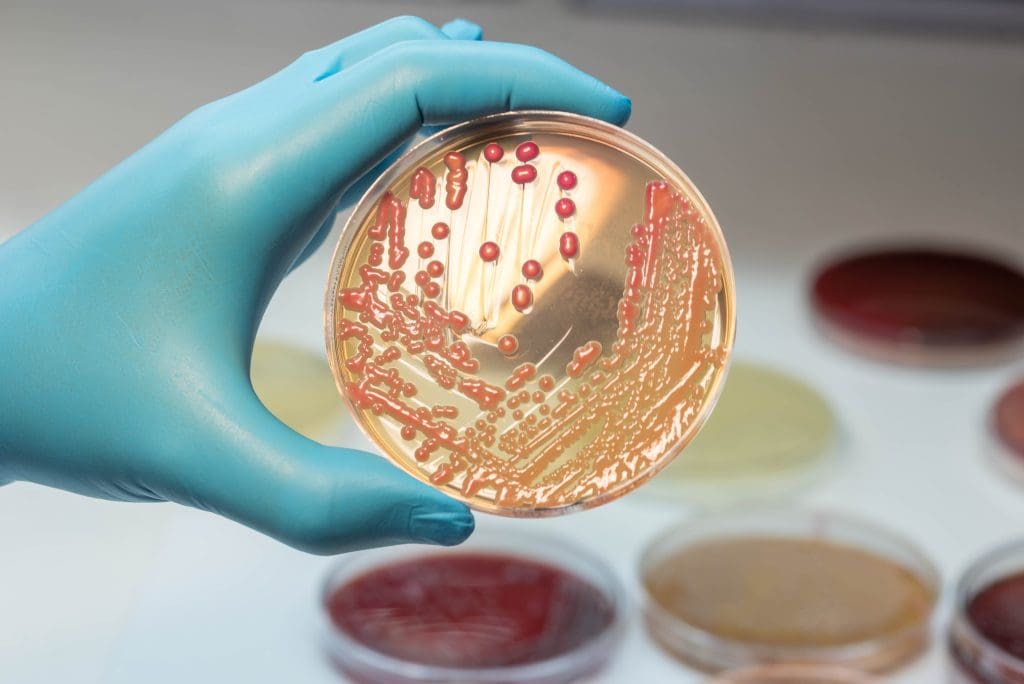
Donating stem cells starts with HLA typing. This test checks if the donor’s immune system matches the recipient’s. It’s key to avoid problems during the transplant.
After matching, the stem cell collection starts. There are two ways: peripheral blood stem cell collection or bone marrow harvest. The first is a blood draw without surgery. The second is a surgery to get stem cells from the bone marrow.
Impact of Donation on Cancer Patients
Stem cell donation gives cancer patients a second chance. It’s a big deal for many. Here are some numbers on how well stem cell transplants work.
| Cancer Type | Transplant Success Rate | Survival Rate |
| Leukemia | 70% | 60% |
| Lymphoma | 65% | 55% |
| Multiple Myeloma | 60% | 50% |
By donating stem cells, you help fight cancer. The process is complex but very important. It brings hope to patients and their families.
Success Rates and Outcomes by Cancer Type
Knowing how well stem cell transplants work is key for both patients and doctors. The success of these treatments changes a lot depending on the cancer type. It’s important to look at the results and survival rates.
Survival Statistics for Blood Cancers
Blood cancers like leukemia and lymphoma have seen big jumps in survival rates thanks to stem cell transplants. The National Cancer Institute says the five-year survival rate for AML patients can be between 30% and 70%. This depends on things like the patient’s age and how far the disease has spread.
Lymphoma patients also have good news. For example, those with Hodgkin lymphoma who get autologous stem cell transplants live longer.
| Cancer Type | Transplant Type | 5-Year Survival Rate |
| Acute Myeloid Leukemia (AML) | Allogeneic | 40% – 60% |
| Acute Lymphoblastic Leukemia (ALL) | Allogeneic | 50% – 70% |
| Hodgkin Lymphoma | Autologous | 60% – 80% |
Factors That Influence Transplant Success
Many things can affect how well a stem cell transplant works. These include the cancer type, the patient’s age and health, and how far the disease has spread. Also, whether the stem cells come from the patient (autologous) or someone else (allogeneic) matters. So does the treatment given before the transplant.
Key factors influencing transplant success include:
- Disease type and stage
- Patient’s age and health status
- Type of stem cell transplant (autologous or allogeneic)
- Conditioning regimen intensity
By knowing these factors and the survival rates for different cancers, patients and doctors can make better choices. This helps in deciding the best treatment options.
Future Directions in Cancer Stem Cell Therapy
The future of cancer treatment is looking bright, thanks to stem cell therapy. Researchers are finding new ways to use stem cells in fighting cancer. This is bringing exciting changes to the field of oncology.
CAR-T Cell Therapy and Stem Cell Approaches
CAR-T cell therapy is a big step forward in cancer treatment. It uses the body’s immune system to fight cancer. By changing T cells to target cancer cells, it has shown great promise in treating blood cancers.
Researchers are now looking at how to use CAR-T cell therapy with stem cells. This could make these treatments even better and safer.
Key benefits of CAR-T cell therapy include:
- Targeted cancer cell destruction
- Potential for long-term remission
- Innovative approach to immunotherapy
Emerging Research and Clinical Trials
The field of cancer stem cell therapy is growing fast. Many clinical trials are underway to find new uses and improve treatments. Researchers are working on better ways to use stem cells and combining them with other treatments.
Ongoing clinical trials are examining:
- The efficacy of stem cell transplants in various cancer types
- New methods for improving stem cell engraftment and reducing complications
- The role of stem cells in cancer relapse and progression
Stem cell therapy is set to be a key player in the future of cancer treatment. With ongoing research and new approaches like CAR-T cell therapy, the outlook for patients is very promising.
Conclusion
Stem cell transplants have changed how we treat cancer, bringing new hope to patients. This method has shown great promise in fighting blood cancers like leukemia and lymphoma. It also works for some solid tumors.
The use of stem cell transplants in cancer treatment is growing. New research and therapies are emerging. Techniques like CAR-T cell therapy are making stem cell therapy even more powerful.
As research keeps moving forward, stem cell transplants will stay key in cancer treatment. The future of cancer care will likely be more personalized and focused. Stem cell therapy will play a big part in this.
FAQ
What is stem cell therapy and how is it used in cancer treatment?
Stem cell therapy, also known as stem cell transplantation, uses stem cells to replace damaged cells. It’s used in cancer treatment to help the bone marrow make healthy blood cells after chemotherapy or radiation.
What types of stem cell transplants are used in cancer treatment?
There are several types of stem cell transplants for cancer treatment. These include autologous (using the patient’s own stem cells), allogeneic (using donor stem cells), haploidentical (using half-matched donor stem cells), and cord blood transplants (using umbilical cord blood stem cells).
What is the difference between autologous and allogeneic stem cell transplants?
Autologous stem cell transplants use the patient’s own stem cells. These are collected, stored, and then re-infused after conditioning. Allogeneic stem cell transplants use donor stem cells, which can help fight cancer cells.
How is a stem cell transplant performed?
The stem cell transplant process involves several steps. First, there’s a pre-transplant evaluation and conditioning to get rid of cancer cells and weaken the immune system. Then, the patient gets stem cells infused.
What is the recovery process like after a stem cell transplant?
Recovery after a stem cell transplant is long and tough. The first 100 days are key, with close monitoring for complications and graft-versus-host disease (GVHD). Long-term care is also important for the patient’s health.
What are the possible side effects and complications of stem cell transplants?
Side effects and complications of stem cell transplants include immediate issues, GVHD, and long-term effects like infertility, secondary cancers, and organ damage.
How do I become a stem cell donor?
To become a stem cell donor, register with a donor registry like the National Marrow Donor Program (NMDP). The process starts with a simple registration, followed by a medical screening and, if chosen, a donation procedure.
What are the success rates and outcomes of stem cell transplants for different types of cancer?
Success rates and outcomes of stem cell transplants vary by cancer type and patient health. Survival rates for blood cancers like leukemia and lymphoma have greatly improved with stem cell transplants.
What is the future of stem cell therapy in cancer treatment?
The future of stem cell therapy in cancer treatment looks promising. New research and clinical trials are exploring CAR-T cell therapy and gene editing. These advancements aim to improve treatment results and expand stem cell therapy use in cancer.
Can stem cells cure cancer?
Stem cells might cure certain cancers, like blood cancers like leukemia and lymphoma. But, the success of stem cell therapy depends on many factors, including cancer type, stage, patient health, and treatment approach.
What is the role of stem cell transplantation in treating multiple myeloma?
Autologous stem cell transplantation is a key treatment for multiple myeloma. It improves survival rates and quality of life. The choice between single or tandem transplants depends on the patient’s specific situation and disease.
Are stem cell transplants used to treat solid tumors?
Yes, stem cell transplants are used for some solid tumors, like neuroblastoma, testicular cancer, and germ cell tumors. Research is also looking into using stem cell therapy for other solid cancers.
What is stem cell therapy and how is it used in cancer treatment?
Stem cell therapy, also known as stem cell transplantation, uses stem cells to replace damaged cells. It’s used in cancer treatment to help the bone marrow make healthy blood cells after chemotherapy or radiation.
What types of stem cell transplants are used in cancer treatment?
There are several types of stem cell transplants for cancer treatment. These include autologous (using the patient’s own stem cells), allogeneic (using donor stem cells), haploidentical (using half-matched donor stem cells), and cord blood transplants (using umbilical cord blood stem cells).
What is the difference between autologous and allogeneic stem cell transplants?
Autologous stem cell transplants use the patient’s own stem cells. These are collected, stored, and then re-infused after conditioning. Allogeneic stem cell transplants use donor stem cells, which can help fight cancer cells.
How is a stem cell transplant performed?
The stem cell transplant process involves several steps. First, there’s a pre-transplant evaluation and conditioning to get rid of cancer cells and weaken the immune system. Then, the patient gets stem cells infused.
What is the recovery process like after a stem cell transplant?
Recovery after a stem cell transplant is long and tough. The first 100 days are key, with close monitoring for complications and graft-versus-host disease (GVHD). Long-term care is also important for the patient’s health.
What are the possible side effects and complications of stem cell transplants?
Side effects and complications of stem cell transplants include immediate issues, GVHD, and long-term effects like infertility, secondary cancers, and organ damage.
How do I become a stem cell donor?
To become a stem cell donor, register with a donor registry like the National Marrow Donor Program (NMDP). The process starts with a simple registration, followed by a medical screening and, if chosen, a donation procedure.
What are the success rates and outcomes of stem cell transplants for different types of cancer?
Success rates and outcomes of stem cell transplants vary by cancer type and patient health. Survival rates for blood cancers like leukemia and lymphoma have greatly improved with stem cell transplants.
What is the future of stem cell therapy in cancer treatment?
The future of stem cell therapy in cancer treatment looks promising. New research and clinical trials are exploring CAR-T cell therapy and gene editing. These advancements aim to improve treatment results and expand stem cell therapy use in cancer.
Can stem cells cure cancer?
Stem cells might cure certain cancers, like blood cancers like leukemia and lymphoma. But, the success of stem cell therapy depends on many factors, including cancer type, stage, patient health, and treatment approach.
What is the role of stem cell transplantation in treating multiple myeloma?
Autologous stem cell transplantation is a key treatment for multiple myeloma. It improves survival rates and quality of life. The choice between single or tandem transplants depends on the patient’s specific situation and disease.
Are stem cell transplants used to treat solid tumors?
Yes, stem cell transplants are used for some solid tumors, like neuroblastoma, testicular cancer, and germ cell tumors. Research is also looking into using stem cell therapy for other solid cancers.