We are leading the way in a groundbreaking treatment that brings hope to those with severe diseases. Allogeneic stem cell transplantation is a complex process. It replaces a patient’s damaged or diseased stem cells with healthy ones from a donor.
At Liv Hospital, we are experts in this life-saving treatment. We focus on the patient, using the latest technology and care. Our team is skilled in allogeneic hematopoietic stem cell transplantation (HSCT). We aim to give the best care for blood cancers and immune disorders.
Key Takeaways
- Allogeneic stem cell transplantation is a treatment for life-threatening diseases.
- Liv Hospital offers a patient-centered approach to this complex procedure.
- The treatment involves replacing diseased stem cells with healthy donor cells.
- Our expertise ensures the best outcomes for global healthcare seekers.
- We combine advanced technology with compassionate care.
Understanding Allogeneic Stem Cell Transplantation
Allogeneic stem cell transplantation is a complex process. It involves moving stem cells from a donor to a patient. This method is key for treating serious diseases. We’ll look into how it works and its history.
Definition and Basic Concept
Allogeneic stem cell transplantation, or allo-HSCT, is when a patient gets stem cells from someone else. This donor is often a family member or someone who matches the patient’s HLA type. The stem cells come from the donor’s bone marrow or blood.
Historical Development of the Procedure
The idea of allogeneic stem cell transplantation has been around for decades. The first successful transplant was in 1968. Over time, the process has gotten safer and more effective.
Advances in conditioning regimens and HLA typing have helped. To learn more about what happens after a transplant, see Liv Hospital.
Here are some key moments in the history of allogeneic stem cell transplantation:
| Year | Milestone | Description |
|---|---|---|
| 1968 | First Successful Transplant | The first successful allogeneic bone marrow transplant was performed. |
| 1980s | Advancements in HLA Typing | Improvements in HLA typing led to better donor-recipient matching. |
| 2000s | Reduced-Intensity Conditioning | The introduction of reduced-intensity conditioning regimens expanded eligibility for allo-HSCT. |
The allogeneic stem cell transplantation process includes many steps. From finding a donor to caring for the patient after the transplant, each step is important. Understanding these steps helps us see how complex this treatment is.
In conclusion, allogeneic stem cell transplantation is a complex medical procedure. It has a rich history and continues to evolve. By understanding its definition, history, and current practices, we can see its importance in treating serious diseases.
The Science Behind Stem Cell Therapy

Stem cell therapy works because stem cells can fix and grow new tissues. These cells can turn into many types of cells, like muscle or nerve cells. This makes stem cell therapy a hopeful treatment for many diseases.
How Stem Cells Function in the Body
Stem cells act like a repair team inside us. They keep dividing to replace old cells. This keeps our body’s tissues and organs healthy.
Key Functions of Stem Cells:
- Regeneration: Stem cells can repair damaged tissues.
- Differentiation: They can turn into specific cell types.
- Self-renewal: Stem cells can keep themselves going.
The Role of Blood-Forming Cells
Blood-forming cells, or hematopoietic stem cells, are key for making blood cells. They live in the bone marrow and create all blood cell types. In allogeneic stem cell transplantation, they help make new blood cells for the patient.
| Cell Type | Function | Clinical Significance |
|---|---|---|
| Hematopoietic Stem Cells | Produce all blood cell types | Crucial for allogeneic HSCT |
| Red Blood Cells | Carry oxygen throughout the body | Essential for oxygen delivery |
| White Blood Cells | Play a key role in immune response | Vital for fighting infections |
To sum up, knowing how stem cells work and the role of blood-forming cells is key. This knowledge helps us understand stem cell therapy. It shows how allogeneic stem cell transplantation can treat serious diseases.
Types of Stem Cell Transplants: Allogeneic vs. Autologous
Stem cell transplants are divided into two main types: allogeneic and autologous. Each has its own features and uses. Knowing the differences helps doctors choose the best treatment for patients.
Key Differences Between Transplant Types
The main difference is where the stem cells come from. In an allogeneic transplant, they come from another person, like a relative or a stranger. On the other hand, an autologous transplant uses the patient’s own stem cells.
Allogeneic stem cell transplantation (allogeneic HSCT) is chosen when the patient’s bone marrow is sick or damaged. It has the benefit of fighting cancer with the donor’s immune cells. But, it also risks complications like graft-versus-host disease (GVHD).
When Allogeneic Transplantation is Preferred
Allogeneic transplantation is chosen when the patient needs healthy donor stem cells. This is true for some types of leukemia, lymphoma, or blood disorders. Finding a good donor is key to this decision.
Choosing between allogeneic and autologous stem cell transplantation is complex. It depends on the patient’s health, their disease, and if a donor is available. Doctors weigh these factors to pick the best treatment for each patient.
Medical Conditions Treated with Allogeneic Stem Cell Transplantation
Allogeneic stem cell transplantation is a key treatment for many serious diseases. It offers hope to patients around the world. This method helps tackle a variety of life-threatening conditions.
It’s mainly used for blood cancers. Leukemia and lymphoma are the most common reasons for this treatment.
Blood Cancers: Leukemia and Lymphoma
Allogeneic HSCT works well for different types of leukemia. This includes acute myeloid leukemia (AML) and chronic myeloid leukemia (CML). For lymphoma, it’s a chance for a cure, even for those with hard-to-treat cases.
The graft-versus-leukemia effect is a big plus. It lets donor immune cells fight off cancer cells left behind.
Bone Marrow Disorders
Bone marrow issues like aplastic anemia and myelodysplastic syndromes are also treated with this method. It replaces the patient’s bad bone marrow with healthy donor cells. This helps make blood cells again.
Immune System Disorders
Some immune system problems, like severe combined immunodeficiency (SCID), can be fixed with allogeneic HSCT. It brings in healthy donor immune cells to fix the patient’s immune system.
We’re always looking to improve allogeneic stem cell transplantation. We’re finding new uses and better ways to help patients with these tough conditions.
The Donor Selection Process
Finding the right donor is key for allogeneic stem cell transplantation success. We look at Human Leukocyte Antigen (HLA) typing and other factors. This ensures the donor is a good match for the recipient.
Related Donors: Siblings and Family Members
Related donors, like siblings or family members, are often the first choice. Siblings have a 25% chance of being a match, while parents and children are typically a half-match. This makes them great candidates for donation.
Unrelated Donors: Finding Matches Through Registries
When a related donor isn’t available, we turn to unrelated donors in registries. These registries are key for finding a match for patients without a family donor. We search for a donor with the right HLA type, boosting transplant success chances.
Haploidentical Transplants: Partial Matches
For those without a fully matched donor, haploidentical transplants are an option. Haploidentical transplants use a partially matched donor, often a family member. New medical tech has made these transplants possible for more patients.
It’s important for patients and families to understand the donor selection process. Finding the best donor can greatly improve transplant success rates.
Understanding HLA Typing and Matching
HLA typing and matching are key to avoiding problems in stem cell transplants. HLA stands for Human Leukocyte Antigen, a part of our immune system. It’s important for the transplant to work well.
What is Human Leukocyte Antigen (HLA)?
HLA proteins are on the surface of white blood cells and other body tissues. They help our immune system tell our proteins from foreign ones, like viruses.
The HLA system is complex, with many genes involved. These genes have lots of versions, helping our immune system fight off many pathogens.
The Importance of HLA Compatibility
It’s vital for the donor and recipient to match in HLA typing for stem cell transplants. Not matching can cause serious issues, like graft-versus-host disease (GVHD). GVHD happens when the donor’s immune cells attack the recipient’s body.
HLA typing finds out what HLA genes and proteins are in someone. This helps match donors and recipients closely. This reduces the chance of GVHD and other problems.
A close HLA match means better transplant results. This includes lower GVHD risk, better cell growth, and longer survival. The needed HLA match level depends on the transplant type and the condition being treated.
The Allogeneic HSCT Transplant Procedure
The allogeneic HSCT process is complex and carefully planned. It aims to replace a patient’s sick or damaged stem cells with healthy ones from a donor.
Pre-Transplant Evaluation and Preparation
Before the transplant, patients get a detailed check-up. This includes tests to see how well their organs work, check for infections, and look at their nutrition.
Doctors also review the patient’s medical history. They look for any risks or complications that might happen during or after the transplant.
Conditioning Regimens: Preparing the Body
Conditioning regimens are key in allogeneic HSCT. They use chemotherapy and/or radiation therapy to clear out the patient’s bone marrow and weaken their immune system.
The goal is to make room for the donor stem cells to grow and produce new blood cells. The type of conditioning depends on the patient’s health, age, and condition.
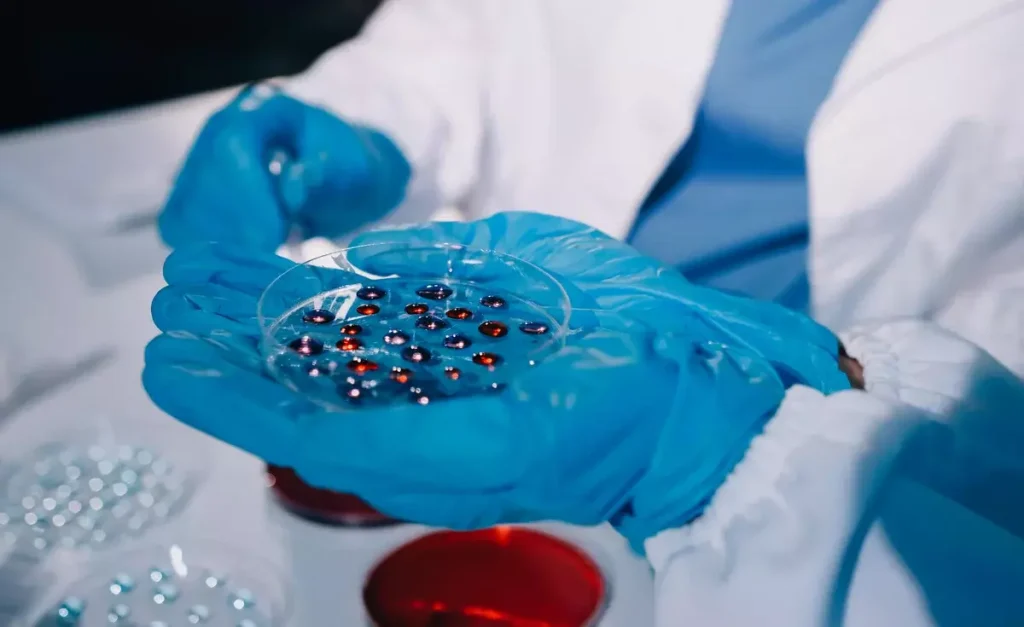
The Transplantation Process
The transplant involves giving the patient donor stem cells through an IV. This is a relatively painless process like getting a blood transfusion.
After the infusion, the donor stem cells go to the bone marrow. There, they start making new blood cells. The patient’s team watches over them, handling any issues and helping them recover.
Post-Transplant Care and Recovery
Recovery after an allogeneic stem cell transplant needs a detailed care plan. It covers both the immediate and long-term needs. This phase is key for managing complications and keeping the patient healthy.
Immediate Post-Transplant Period
The first days after the transplant are risky due to a weak immune system. Close monitoring is vital to catch and treat any problems quickly. We focus on stopping infections, managing pain, and watching for signs of the transplant working.
Patients often stay isolated to avoid infections. They take medicines to prevent certain infections. Blood tests are regular to check blood counts and watch for transplant failure or other issues.
Long-term Follow-up and Monitoring
After the initial recovery, long-term follow-up is essential. Regular visits with the healthcare team are needed to track recovery and manage transplant effects. We also address any new concerns or complications.
Long-term care includes watching for chronic GVHD, managing medications, and supporting physical and emotional healing. We also focus on keeping the patient healthy with vaccinations, lifestyle advice, and preventive measures.
Managing Possible Complications
Dealing with possible complications is a big part of post-transplant care. We watch for GVHD, infections, and other transplant-related issues. Prompt action is key to prevent severe problems.
We teach patients to recognize signs and symptoms of complications. This teamwork helps ensure the best results for those who have had an allogeneic stem cell transplant.
Potential Risks and Complications
Allogeneic stem cell transplantation can save lives but comes with big risks. It’s key to know the possible problems it can cause. Understanding these risks helps patients make informed choices.
Graft-Versus-Host Disease (GVHD)
Graft-versus-host disease is a big risk with this treatment. It happens when the donor’s immune cells attack the recipient’s body. GVHD can be mild or severe and affect many parts of the body.
Acute GVHD usually shows up within 100 days after the transplant. Chronic GVHD can happen later and last for years.
To fight GVHD, we use:
- Medicines to calm down the donor’s immune cells
- Watching for GVHD signs
- Helping with symptoms and preventing more problems
Infections and Immune System Recovery
Getting infections is a big risk after this transplant, mainly in the early days. The immune system is very weak then. We use many ways to stop and treat infections, like:
- Antibiotics and antivirals to prevent infections
- Watching for infection signs
- Helping with care, like keeping the patient isolated and giving them food
Getting the immune system back takes a long time, sometimes years. Patients are more likely to get infections during this time. We teach patients how to stay safe and help them recover.
Other Possible Problems
There are other risks with allogeneic stem cell transplantation, like:
- Damage to organs, like the liver or lungs
- Getting cancer again years later
- Problems with metabolism and hormones
Knowing about these risks is very important for patients and their families. Working with our team helps patients understand and deal with these risks. This way, they can make good choices about their care.
Patient Experience and Quality of Life
Patients going through allogeneic stem cell transplantation face many challenges. These challenges affect their physical and emotional health. The treatment is very stressful and can cause symptoms like fatigue, pain, and emotional distress.
Physical and Emotional Challenges
The physical challenges of allogeneic stem cell transplantation are big. Patients may feel fatigue, pain, and infections that change their daily lives. The emotional side is also tough. Patients might feel anxious, depressed, or overwhelmed by the treatment.
Emotional challenges are as important as physical ones. The fear of the unknown and the stress of treatment can hurt a patient’s mental health. Healthcare providers must help with these emotional challenges.
Support Systems and Resources
Support systems are key for patients facing allogeneic stem cell transplantation. Family, friends, and healthcare providers are important. We urge patients to use these resources to handle treatment’s physical and emotional demands.
Some important support systems include:
- Counseling services for emotional and psychological needs
- Support groups for sharing experiences and advice
- Educational resources to understand treatment and what to expect
By giving full support and resources, we aim to improve patients’ quality of life. Our goal is to make sure patients get the care they need to get through this tough time.
Advancements in Allogeneic Stem Cell Transplantation
Research and new technologies are making allogeneic stem cell transplantation better. Patients are now getting treatments that are more effective and safer.
Recent Technological Innovations
In recent years, big steps have been made in allogeneic stem cell transplantation. Improvements in HLA typing have made matching donors and recipients easier. This has lowered the chance of problems like graft-versus-host disease (GVHD). Also, new conditioning regimens help prepare patients better for the transplant.
- Enhanced donor selection processes
- Advanced GVHD prophylaxis techniques
- Better management of post-transplant complications
These new technologies have led to better results for patients. Healthcare teams can now tailor treatments to meet each patient’s specific needs.
Emerging Research and Future Directions
The future of allogeneic stem cell transplantation looks bright. Gene editing technologies and cellular therapies are leading the way. They could bring new ways to treat blood diseases.
- Gene editing for genetic diseases
- Cellular therapies to enhance immune recovery
- Novel approaches to GVHD management
As research keeps moving forward, we’ll see even more new treatments. Healthcare providers will keep giving patients the best care possible.
Conclusion: The Life-Saving Potential of Allogeneic Stem Cell Transplantation
Thanks to new research and technology, this treatment is getting better. It’s helping more people live longer, healthier lives. The impact of this treatment on medicine is huge.
We must keep supporting research in this field. This ensures patients get the best care. Allogeneic stem cell transplantation is a key treatment for many. It keeps getting better, helping those in need.
What is allogeneic stem cell transplantation?
Allogeneic stem cell transplantation is a medical procedure. It treats life-threatening diseases by replacing a patient’s stem cells with healthy ones from a donor.
How does allogeneic stem cell transplantation differ from autologous transplantation?
Allogeneic uses stem cells from a donor. Autologous uses the patient’s own stem cells. The main difference is the source of the stem cells.
What is the role of HLA typing in allogeneic stem cell transplantation?
HLA typing finds compatible donors. It’s key to avoid complications like Graft-Versus-Host Disease (GVHD) and ensure transplant success.
What are the possible risks and complications of allogeneic stem cell transplantation?
Risks include GVHD, infections, organ damage, and secondary cancers. Knowing these risks is vital for patients and caregivers.
What medical conditions are treated with allogeneic stem cell transplantation?
It treats blood cancers, bone marrow disorders, and immune system disorders. These are life-threatening conditions.
How is a donor selected for allogeneic stem cell transplantation?
Donors are chosen based on HLA matching. Family members are first, then unrelated donors from registries.
What is the significance of conditioning regimens in allogeneic HSCT?
Conditioning regimens prepare the body for the transplant. They use chemotherapy and/or radiation to remove diseased cells and weaken the immune system.
What is Graft-Versus-Host Disease (GVHD)?
GVHD happens when donor immune cells attack the recipient’s tissues. It’s a major concern in allogeneic stem cell transplantation.
What support systems are available for patients undergoing allogeneic stem cell transplantation?
Patients have family, friends, and healthcare providers for support. These help with physical and emotional challenges.
What advancements have been made in allogeneic stem cell transplantation?
Advances include better HLA typing and conditioning regimens. Research also explores new therapies like gene editing and cellular therapies.
What is the definition of allogeneic hematopoietic stem cell transplantation (HSCT)?
Allogeneic hematopoietic stem cell transplantation (HSCT) is a procedure. It involves a patient getting stem cells from a donor, often a family member or an unrelated individual.
What is the difference between allogeneic and allogenic stem cell transplant?
Allogeneic and allogenic are the same. They both refer to stem cell transplants using donor stem cells.
References
- National Cancer Institute. “Allogeneic Stem Cell Transplant. In NCI Cancer Terms Dictionary. Retrieved from https://www.cancer.gov/publications/dictionaries/cancer-terms/def/allogeneic-stem-cell-transplant
- Wikipedia. “Hematopoietic Stem Cell Transplantation. Retrieved from https://en.wikipedia.org/wiki/Hematopoietic_stem_cell_transplantation
- PMC Article: PMC6953421. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC6953421/
- American Cancer Society. “Stem Cell Transplant: Treatments and Side Effects. Retrieved from https://www.cancer.org/treatment/treatments-and-side-effects/treatment-types/stem-cell-transplant.html