Last Updated on October 28, 2025 by
We are seeing a big change in how we fight cancer with CAR T-cell therapy. It’s a new way to use a patient’s own immune system to attack cancer.
This method uses chimeric antigen receptor technology to make T cells better at finding and killing cancer cells. It’s a personalized treatment that has worked well for some types of leukemia and lymphoma.
At Liv Hospital, we aim to provide top-notch healthcare. We make sure our patients get the best care possible. Our focus on new cancer treatments like CAR T-cell therapy is changing how we fight cancer.
Key Takeaways
- CAR T-cell therapy is a revolutionary form of immune cell therapy.
- It uses chimeric antigen receptor technology to engineer T cells to fight cancer.
- This therapy has shown high remission rates in certain types of leukemia and lymphoma.
- Liv Hospital is committed to delivering world-class healthcare with international patient support.
- Our innovative approach to cancer care is transforming the oncology landscape.
The Revolutionary Approach of CAR T-Cell Therapy in Oncology
CAR T-cell therapy is changing oncology, giving hope to those with hard-to-treat blood cancers. This new treatment is a big step forward in cancer care.
This therapy takes T cells from a patient, changes them to fight cancer, and puts them back. It’s a custom treatment for each patient.
From Conventional Treatments to Cellular Immunotherapy
Old treatments like chemo and radiation are common but have big side effects. CAR T-cell therapy uses the body’s immune system instead.
This new method is more precise and might be safer. It’s a big leap in cancer treatment, giving hope to those who’ve tried everything else.
How CAR T-Cell Therapy Transforms Cancer Care
CAR T-cell therapy changes cancer care in many ways. It’s a treatment made just for the patient, using their T cells to find and kill cancer cells.
It’s also very effective against some blood cancers, like leukemia and lymphoma. This means better chances of getting better and living a better life.
As we keep working on CAR T-cell therapy, we learn more about cancer and find better ways to treat it. This is key to improving cancer care and helping patients all over the world.
The Science Behind CAR T-Cell Treatment

CAR T-cell treatment is a leading edge in immunotherapy. It uses genetically modified T cells to fight cancer more effectively. This method has changed oncology, giving hope to those with blood cancers.
Understanding Chimeric Antigen Receptor Technology
Chimeric antigen receptor (CAR) technology is key to CAR T-cell therapy. It makes T cells recognize and attack cancer cells. This is done by adding a CAR that spots cancer cell antigens.
To make CAR T cells, several steps are taken:
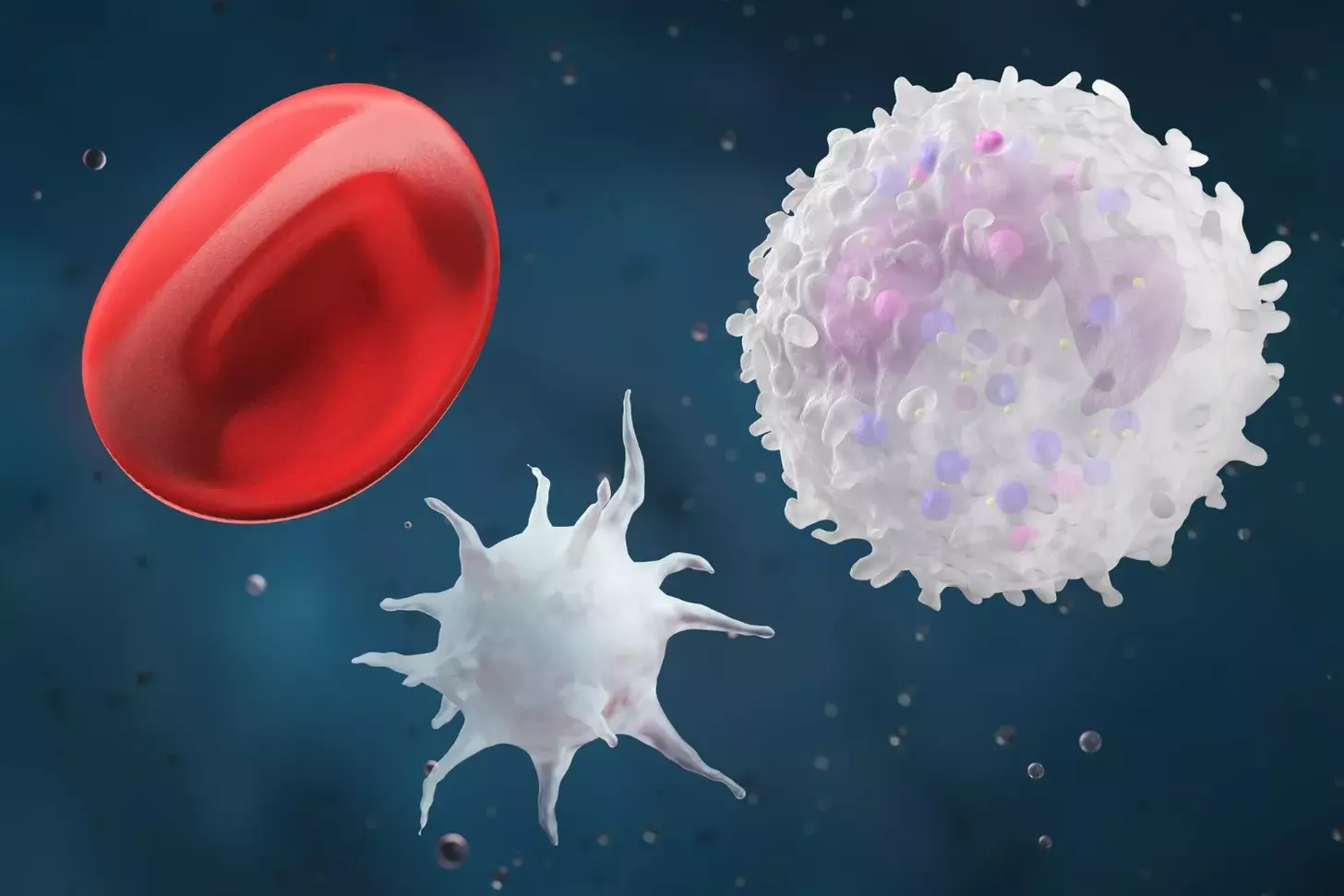
- Collecting T cells from the patient’s blood
- Genetically modifying these T cells to express the CAR
- Expanding the modified T cells
- Infusing the CAR T cells back into the patient
How T Cells Become Powerful Cancer-Fighting Agents
After being infused, CAR T cells fight cancer. They find and destroy cancer cells. This method is precise, harming fewer healthy cells than traditional treatments.
The table below summarizes the key components and functions of CAR T-cell therapy:
| Component | Function |
|---|---|
| CAR T Cells | Genetically modified T cells that recognize and target cancer cells |
| Chimeric Antigen Receptor | Enables T cells to recognize specific antigens on cancer cells |
| T Cell Collection | Initial step where T cells are collected from the patient’s blood |
| Genetic Modification | Process of engineering T cells to express CAR |
Understanding CAR T-cell treatment shows its complexity and promise. As research grows, we’ll see better CAR T-cell tech. This could help more cancers in the future.
The CAR T-Cell Treatment Process: From Collection to Infusion
Exploring the CAR T-Cell treatment process is key. It involves several stages, from collecting T cells to infusing them. Each step is carefully planned to help our patients get the best results.
T Cell Collection and Isolation Procedures
The first step is collecting T cells from the patient’s blood. This is done through a process called leukapheresis. It takes a few hours and uses a special machine to separate T cells from other blood parts. Then, the T cells are sent to a lab for further work.
In the lab, the T cells are purified and concentrated. This is important for the next steps in genetic modification.
Genetic Engineering and CAR Expression
Next, the T cells are genetically engineered. They are made to express a chimeric antigen receptor (CAR) that can find specific cancer cells. This is done using viral vectors that add the CAR gene to the T cells. The T cells then grow and multiply.
This genetic engineering is very precise. It adds the CAR gene to the T cells’ DNA. This helps the T cells find and attack cancer cells better. The CAR on the T cells is key to the therapy’s success.
Cell Expansion and Patient Preparation
After being genetically modified, the CAR T cells grow in number. This can take days to weeks. During this time, the patient’s health is closely watched, and they are prepared for the CAR T cell infusion.
Preparing the patient is a big part of the treatment. We check if the patient is ready for the infusion and the care that follows. This includes managing side effects and having a plan for any problems.
The CAR T-Cell treatment shows how far cellular immunotherapy has come. Understanding this process helps us see the complexity and innovation of CAR T-Cell therapy.
FDA-Approved CAR-T Therapies and Their Applications
FDA-approved CAR-T therapies are a big step in fighting blood cancers. They have shown great results in clinical trials. This gives new hope to patients with hard-to-treat leukemia and lymphoma.
Tisagenlecleucel (Kymriah) for Leukemia and Lymphoma
Tisagenlecleucel, or Kymriah, was the first CAR-T therapy approved by the FDA. It helps treat certain B-cell cancers and lymphoma. Clinical trials have shown amazing results, with many patients going into complete remission.
Axicabtagene Ciloleucel (Yescarta) and Other Approved Therapies
Axicabtagene ciloleucel, or Yescarta, is another FDA-approved CAR-T therapy. It treats certain lymphomas. Other CAR-T therapies are also helping fight blood cancers, expanding treatment options.
We are proud to offer these FDA-approved CAR-T therapies. They have been tested thoroughly for safety and effectiveness. The FDA’s approval process includes many clinical trials to ensure these therapies improve patient outcomes.
The Rigorous Approval Process and Clinical Requirements
The FDA’s approval process for CAR-T therapies is very strict. It involves several clinical trial phases. These trials check the therapy’s safety, effectiveness, and side effects. The strict standards mean only therapies that greatly benefit patients are approved.
| FDA-Approved CAR-T Therapy | Indication | Notable Clinical Trial Results |
|---|---|---|
| Tisagenlecleucel (Kymriah) | B-cell precursor ALL, DLBCL | Significant complete remission rates |
| Axicabtagene Ciloleucel (Yescarta) | DLBCL, primary mediastinal large B-cell lymphoma | High overall response rates |
As we keep improving CAR-T cell therapy, more FDA-approved treatments become available. These therapies are a big step forward in treating blood cancers. They offer hope and better outcomes for patients and healthcare providers.
Clinical Outcomes and Success Rates of CAR T-Cell Therapy
CAR T-cell therapy is a new way to fight cancer. It has shown great results, improving survival rates and quality of life. This therapy works best for certain blood cancers, giving hope to those who didn’t respond to other treatments.
Remarkable Remission Rates in Blood Cancers
CAR T-cell therapy has been a big success, showing remarkable remission rates in blood cancers. Many patients have seen complete remission, with some staying in remission for a long time. For example, a study on PubMed showed its effectiveness in treating relapsed or refractory leukemia.
The therapy changes T cells to better fight cancer. This targeted method has led to better results, with many patients seeing a big drop in cancer.
Long-term Survival and Quality of Life Improvements
Not only does CAR T-cell therapy achieve high remission rates, but it also leads to long-term survival and better quality of life. Patients often feel better and can do their usual activities again. The therapy’s ability to keep patients in remission for a long time has greatly improved survival rates.
As we keep watching the long-term effects of CAR T-cell therapy, we see great promise. Ongoing research aims to make the therapy even better and use it for more cancers.
Challenges and Side Effects of CAR T-Cell Therapy
Exploring CAR T-cell therapy reveals its challenges and side effects. This treatment has shown great promise against some cancers. Yet, it comes with its own set of hurdles.
Causes and Symptoms of Cytokine Release Syndrome
Cytokine release syndrome (CRS) is a major side effect of CAR T-cell therapy. It happens when T cells release a lot of cytokines into the blood. This can cause a range of symptoms, from mild to severe.
The symptoms of CRS include fever, fatigue, and nausea. In severe cases, it can lead to hypotension and organ dysfunction. Understanding CRS is key to managing it effectively.
| CRS Grade | Symptoms | Management |
|---|---|---|
| 1 | Mild symptoms, fever | Supportive care, monitoring |
| 2-3 | Moderate to severe symptoms, hypotension | Tocilizumab, corticosteroids |
| 4-5 | Life-threatening symptoms, organ dysfunction | Intensive care, tocilizumab, corticosteroids |
Neurotoxicity and Other Common Side Effects
Neurotoxicity is another major side effect of CAR T-cell therapy. It can cause confusion, agitation, and even seizures. The exact cause is not fully understood but is thought to be related to cytokine release and disruption of the blood-brain barrier.
Other common side effects include:
- B cell aplasia
- Infections
- Hemophagocytic lymphohistiocytosis (HLH)
These side effects need careful monitoring and management to ensure the best outcomes for patients.
Management Strategies for CAR T-Cell Therapy Complications
Managing CAR T-cell therapy complications is vital for patient safety. We use several strategies, including:
- Early detection and grading of CRS and neurotoxicity
- Use of tocilizumab and corticosteroids for CRS management
- Supportive care for managing symptoms and preventing infections
- Intensive care for severe cases
By understanding side effects and having effective management strategies, we can improve patient outcomes with CAR T-cell therapy.
“The key to successful CAR T-cell therapy lies not only in its efficacy but also in our ability to manage its side effects effectively.”
Innovations in CAR T-Cell Research and Development
CAR T-cell therapy is getting better with new research and development. We aim to lead in these advancements for our patients. New ideas focus on making CAR T-cell therapy more precise, safe, and effective.
Enhancing Specificity with Dual-Antigen Receptors
A big step in CAR T-cell research is the creation of dual-antigen receptors. These receptors can spot two specific cancer cell markers. This makes the therapy more precise and lowers the chance of cancer cells evading treatment. Dual-antigen receptors aim to solve the problem of single-antigen targeting.
Molecular Switches for Better Control
Molecular switches are another innovation. They let us control CAR T-cells better. These switches can turn CAR T-cells on or off, helping to manage side effects. This is key in reducing cytokine release syndrome (CRS) and other harmful effects of CAR T-cell therapy.
Advancements in Next-Generation CAR Designs
New CAR designs are being worked on to boost CAR T-cell therapy’s benefits. These include adding co-stimulatory domains and using different antigen recognition domains. For example, some new CARs can release cytokines to fight tumors better. For more on other treatments like stem cell transplants, check out Liv Hospital’s page on autologous vs. allogeneic.
Expanding Applications: Beyond Blood Cancers to Solid Tumors
We’re leading the way in using CAR T-cell therapy for solid tumors. This area is tough but full of hope. CAR T-cell therapy has changed the game for some blood cancers. Now, we’re working hard to see if it can help with solid tumors too.
It’s not easy to use CAR T-cell therapy for solid tumors. We face big challenges. Finding the right targets on tumor cells is key. This helps avoid harming healthy cells and reduces side effects.
Current Challenges in Treating Solid Tumors with CAR T-Cells
There are many hurdles when treating solid tumors with CAR T-cells:
- The tumor environment can block CAR T-cells from working well.
- It’s hard to target all cancer cells because tumors have different antigens.
- The tumor’s stroma can stop CAR T-cells from getting inside.
But, researchers are making great strides. For example, tweaking CAR T-cells to fight through the tumor’s defenses is showing promise. Combination therapies with checkpoint inhibitors are also being tested to boost results.
Promising Approaches and Ongoing Clinical Trials
New ideas are being explored to tackle these challenges. These include:
- Creating CAR T-cells that can target multiple antigens to improve accuracy.
- Designing CAR T-cells that last longer and grow more.
- Using CAR T-cell therapy with other treatments to make it more effective.
Studies are underway to test these new methods. For instance, a study showed that armored CAR T-cells could fight solid tumors better by releasing cytokines.
“The future of CAR T-cell therapy lies in its ability to be adapted and optimized for a wide range of cancers, including solid tumors. Ongoing research and clinical trials are critical in achieving this goal.”
We’re dedicated to pushing the limits of CAR T-cell therapy. By tackling the challenges and exploring new ideas, we hope to offer hope to many more patients. This includes those with solid tumors.
The Economic Landscape of CAR T-Cell Treatment
The cost of CAR T-cell treatment is high, and insurance coverage varies. This therapy is changing cancer care. It’s important for patients, doctors, and insurance companies to understand its costs.
Cost Considerations and Insurance Coverage Challenges
CAR T-cell therapy costs between $300,000 and $475,000 per patient. The high price comes from making and giving the treatment. It also includes caring for patients and managing side effects.
Insurance for CAR T-cell therapy differs by provider and policy. Many plans cover some or all costs. But, patients often have to pay a lot out of pocket, like deductibles and copays.
Key cost considerations include:
- The cost of T-cell collection and genetic modification
- Expenses related to cell manufacturing and quality control
- Costs associated with patient care and management of side effects
- Potential costs for additional treatments or hospitalizations
Industry Efforts to Improve Accessibility and Affordability
We know the high cost of CAR T-cell therapy is a big problem. We’re working with patients, insurers, and partners to make it more affordable and accessible.
Some strategies we’re exploring are:
- Developing more efficient manufacturing processes to reduce costs
- Improving patient selection and treatment protocols to enhance outcomes
- Implementing innovative pricing models and payment structures
- Enhancing patient support programs and financial assistance initiatives
We aim to make this life-saving treatment available to those who need it most. We want to ensure CAR T-cell therapy is sustainable for the long term.
As CAR T-cell therapy evolves, we’re committed to top-notch healthcare and support for international patients. We’re working hard to make this treatment more accessible and affordable. Our goal is to help patients worldwide.
Specialized Centers Offer CAR T-Cell Immunotherapy
Delivering CAR T-cell immunotherapy needs a team effort, found in specialized cancer centers. Liv Hospital is proud to offer this therapy with a team of experts and top-notch facilities.
Requirements for Hospitals Administering CAR T-Cell Therapy
Centers for CAR T-cell therapy must be highly specialized. They need experienced staff, advanced facilities, and the skill to handle side effects.
The main needs for these hospitals are:
- Teams with a lot of experience
- Advanced setup for cell work and storage
- Ability to deal with side effects like cytokine release syndrome
- Full support for patients
Liv Hospital’s Implementation of Advanced CAR T-Cell Protocols
At Liv Hospital, we aim for top healthcare with advanced CAR T-cell protocols. Our team works closely with patients for personalized care.
Our advanced protocols include:
| Protocol | Description | Benefits |
|---|---|---|
| Personalized Cell Therapy | Tailored CAR T-cell therapy for each patient | Better results and safety |
| Advanced Cell Processing | Top technology for cell work and storage | Better cell health and function |
| Comprehensive Support Services | Full support from a team for patients during treatment | Better patient experience and results |
We meet the tough standards for CAR T-cell therapy. We’re committed to supporting our patients fully during their treatment.
Conclusion: The Future of CAR T-Cell Therapy in Cancer Care
CAR T-cell therapy has changed cancer care forever. It has shown great success in treating some blood cancers. This has given hope to many patients around the world.
Now, researchers are working hard to use CAR T-cell therapy for other cancers too. They aim to make it work for solid tumors. We’re all about making CAR T-cell therapy better, helping more people, and improving treatment results.
The outlook for CAR T-cell therapy is bright. New studies are leading to better ways to treat patients. We’re excited to keep improving care and support for everyone.
What is CAR T-cell therapy?
CAR T-cell therapy is a new way to fight cancer. It changes a patient’s T cells to find and kill cancer cells. It’s been very effective against some blood cancers like leukemia and lymphoma.
How does CAR T-cell therapy work?
First, we take T cells from the patient’s blood. Then, we make these cells recognize cancer cells. After that, we put the changed cells back into the patient.
What are the benefits of CAR T-cell therapy?
This therapy has been very successful in treating blood cancers. It has high remission rates. It’s a targeted treatment that improves survival and quality of life for many patients.
What are the side effects of CAR T-cell therapy?
Side effects include cytokine release syndrome (CRS) and neurotoxicity. CRS can cause mild to severe symptoms. Neurotoxicity can lead to confusion and other brain problems. We work hard to manage these side effects.
Are there any FDA-approved CAR T-cell therapies?
Yes, the FDA has approved therapies like tisagenlecleucel (Kymriah) and axicabtagene ciloleucel (Yescarta) for blood cancers. They have been tested thoroughly and show great results.
Can CAR T-cell therapy be used to treat solid tumors?
CAR T-cell therapy works well for blood cancers but is being studied for solid tumors too. Early trials look promising.
How much does CAR T-cell therapy cost?
CAR T-cell therapy is expensive, which can be a problem for some patients. We’re working to make it more affordable and accessible.
What is the role of chimeric antigen receptor technology in CAR T-cell therapy?
This technology helps T cells target cancer cells better. It’s key to CAR T-cell therapy, making treatment more precise and effective.
How is CAR T-cell therapy administered?
The process includes collecting T cells, engineering them, expanding the cells, and infusing them back into the patient. Our team ensures the best care for our patients.