We are seeing a big change in treating lymphoma with CAR T cell therapy. This method uses a patient’s own immune cells to fight cancer. It makes these cells recognize and attack cancer cells.
First, T cells are taken from the patient’s blood. Then, they are changed to find and destroy cancer cells. This personalized treatment has shown great promise in trials. It gives hope to those who didn’t get better with usual treatments.
Key Takeaways
- CAR T cell therapy is a form of immunotherapy that uses a patient’s own T cells to fight cancer.
- The therapy involves genetically modifying T cells to recognize and target cancer cells.
- CAR T cell therapy has shown promising results in treating lymphoma.
- This personalized treatment offers new hope to patients who have not responded to traditional therapies.
- The therapy is made from a patient’s own cells, reducing the risk of rejection.
Understanding CAR T Cell Therapy
CAR T cell therapy is a new way to fight cancer. It changes a patient’s T cells to find and kill cancer cells. This immunotherapy is very promising for some lymphoma types.
Definition and Basic Concept
CAR T cell therapy uses chimeric antigen receptors. These receptors help T cells find specific proteins on cancer cells. First, T cells are taken from the patient’s blood. Then, they are genetically changed to make CARs. After that, these modified cells are put back into the patient.
The chimeric antigen receptor finds a specific antigen on lymphoma cells. This lets the CAR T cells destroy these cells well.
Historical Development of CAR T Cell Therapy
The making of CAR T cell therapy took time. It grew from new ideas in immunology and genetic engineering. The FDA first approved it in 2017, a big step in cancer treatment.
After that, CAR T cell therapy kept getting better. Researchers are working hard to make it more effective and safer. The story of CAR T cell therapy shows how far immunotherapy has come.
The Science Behind CAR T Cell Therapy
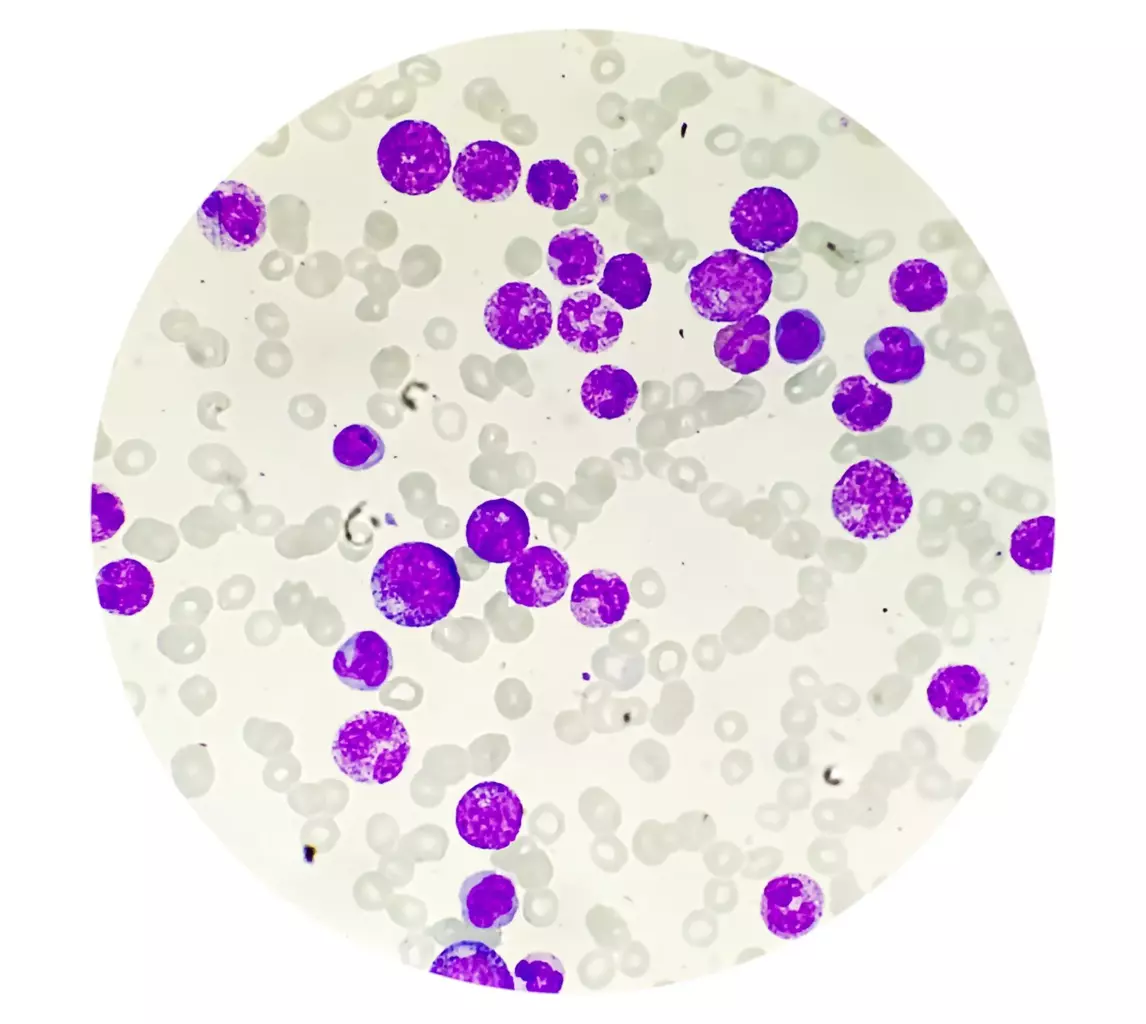
T cells are key to our immune system and are used in CAR T cell therapy to fight cancer. They help protect our body from diseases. Knowing how T cells work is key to understanding CAR T cell therapy.
T Cells and Their Role in Immune Response
T cells are a type of white blood cell that leads the immune response. They can kill infected cells or send signals to other immune cells. In cancer, T cells can find and attack tumor cells. But, cancer cells often hide from the immune system. CAR T cell therapy boosts T cells’ ability to fight cancer.
Chimeric Antigen Receptors: Structure and Function
Chimeric antigen receptors (CARs) are made to find specific cancer cell markers. A CAR has parts that bind to antigens, connect to the cell, and send signals inside. This makes CAR T cells better at finding and killing cancer cells than regular T cells.
The part of the CAR that finds tumor markers comes from antibodies. When it finds a marker, the CAR T cell gets activated. This leads to the cancer cell’s death.
How Genetic Modification Creates CAR T Cells
To make CAR T cells, several steps are taken. First, T cells are taken from the patient’s blood or through leukapheresis. Then, these T cells are changed genetically to add the CAR gene. The modified T cells are grown and activated before being given back to the patient.
This genetic change lets T cells find and attack cancer cells better.
| Step | Description |
|---|---|
| T Cell Isolation | T cells are isolated from the patient’s blood. |
| Genetic Modification | T cells are genetically modified to express CAR. |
| CAR T Cell Expansion | Modified T cells are expanded and activated. |
| Infusion | CAR T cells are infused back into the patient. |
Understanding CAR T cell therapy shows the complexity and innovation in cancer treatment. It combines T cell biology, genetic engineering, and immunotherapy. This makes CAR T cell therapy a strong tool against cancer.
CAR T Cell Therapy for Lymphoma: Mechanism of Action
CAR T cell therapy is a new hope for lymphoma patients. It changes a patient’s T cells to fight cancer cells. This method is a game-changer for those with hard-to-treat lymphoma.
How CAR T Cells Target Lymphoma Cells
CAR T cells are made to find and destroy lymphoma cells. They focus on the CD19 antigen, common in B-cell lymphomas. This way, they can kill cancer cells without harming healthy tissues.
To make CAR T cells, T cells are first taken from the patient. Then, they are genetically modified and grown. After that, they are given back to the patient. These cells then keep finding and killing lymphoma cells.
Advantages Over Traditional T-Cell Receptors
CAR T cell therapy has big advantages over traditional TCR therapy. CAR T cells can find and attack cancer cells directly, without needing MHC molecules. This makes them more effective against tumors that hide from the immune system.
| Feature | CAR T Cell Therapy | Traditional TCR Therapy |
|---|---|---|
| Antigen Recognition | Direct recognition without MHC | MHC-dependent recognition |
| Tumor Escape Mechanisms | Less susceptible to MHC downregulation | Susceptible to MHC downregulation |
| Versatility | Can target a wide range of antigens | Limited by MHC restriction |
CAR T cell therapy is a promising treatment for lymphoma. Its targeted approach and flexibility make it a strong option. As research grows, we’ll see even better versions of this therapy.
Types of Lymphoma Treatable with CAR T Cell Therapy
CAR T cell therapy is a new hope for patients with certain lymphomas. It has shown great promise in treating many lymphoma types. This therapy offers a chance for those who have not seen results from traditional treatments.
Non-Hodgkin Lymphoma
Non-Hodgkin lymphoma (NHL) includes many types of lymphomas. CAR T cell therapy works well for some NHL subtypes, like diffuse large B-cell lymphoma (DLBCL) and follicular lymphoma. These lymphomas are aggressive and hard to treat, making CAR T cell therapy very important.
Studies show that CAR T cell therapy can help patients with relapsed or refractory DLBCL. The process involves taking T cells from the patient, changing them to attack cancer cells, and then putting them back in the patient.
Other Lymphoma Types
CAR T cell therapy is also being tested for other lymphomas. Researchers are looking into its use for mantle cell lymphoma and other rare types. CAR T cell therapy can be made to target specific cancer cells, making it a hopeful treatment for many lymphomas.
As research keeps improving, we will likely see more lymphomas treatable with CAR T cell therapy. This progress is exciting for better patient outcomes and more tailored treatments.
The CAR T Cell Therapy Process
The journey through CAR T cell therapy involves several key stages. Each stage is important for the treatment’s success. We will explain the main steps in this innovative treatment.
Collection of T Cells (Leukapheresis)
The first step is collecting T cells from the patient’s blood. This is done through a procedure called leukapheresis. The blood is drawn, and the T cells are separated from other components. The rest of the blood is then returned to the patient.
This process can take several hours. It is usually done on an outpatient basis.
Engineering the CAR T Cells
After collecting the T cells, they are sent to a lab for genetic modification. They are made to express chimeric antigen receptors (CARs). These CARs target specific proteins on lymphoma cells.
The T cells are genetically modified using a viral vector. They are then expanded and prepared for infusion back into the patient.
Lymphodepletion Chemotherapy
Before the CAR T cell infusion, patients undergo lymphodepletion chemotherapy. This treatment depletes the patient’s existing lymphocytes. It makes space for the infused CAR T cells to expand and function better.
It also reduces the patient’s immune response against the CAR T cells. This improves their persistence and efficacy.
Infusion of CAR T Cells
The final step is infusing the engineered CAR T cells back into the patient. This is similar to a blood transfusion. It is done in a clinical setting where the patient can be monitored for any immediate reactions.
After infusion, the CAR T cells target and destroy lymphoma cells. This can lead to a significant reduction in tumor burden.
The entire CAR T cell therapy process takes several weeks to a few months. The exact timeline varies based on individual patient factors and the specific treatment protocol.
| Step | Description | Timeline |
|---|---|---|
| Leukapheresis | Collection of T cells from patient’s blood | 1-2 days |
| CAR T Cell Engineering | Genetic modification of T cells to target lymphoma cells | 2-4 weeks |
| Lymphodepletion Chemotherapy | Chemotherapy to prepare patient’s body for CAR T cells | 3-7 days |
| CAR T Cell Infusion | Infusion of engineered CAR T cells back into patient | 1 day |
FDA-Approved CAR T Cell Therapies for Lymphoma
The FDA has approved several CAR T cell therapies for lymphoma. This gives new hope to patients. These therapies have changed how we treat lymphoma, making treatment more targeted and effective.
Axicabtagene Ciloleucel (Yescarta)
Axicabtagene ciloleucel, known as Yescarta, is a leading CAR T cell therapy for lymphoma. It is approved for adult patients with relapsed or refractory large B-cell lymphoma after two or more treatments. The FDA approved Yescarta based on its success in clinical trials, showing it can help patients with few treatment options.
The ZUMA-1 trial tested Yescarta in patients with refractory diffuse large B-cell lymphoma. The trial found a 72% overall response rate, with 54% achieving complete response. These results led to Yescarta’s FDA approval, a major breakthrough in lymphoma treatment.
Tisagenlecleucel (Kymriah) and Other Approved Therapies
Tisagenlecleucel, or Kymriah, is another FDA-approved CAR T cell therapy for lymphoma. It’s for adult patients with relapsed or refractory diffuse large B-cell lymphoma after two or more treatments. Kymriah has shown promising results in trials, with a high response rate and long-lasting effects.
Other CAR T cell therapies are also being studied for lymphoma treatment. Ongoing research and trials are helping us understand CAR T cell therapy’s role in treating lymphoma better.
| Therapy | Indication | Response Rate |
|---|---|---|
| Axicabtagene Ciloleucel (Yescarta) | Relapsed/Refractory Large B-Cell Lymphoma | 72% |
| Tisagenlecleucel (Kymriah) | Relapsed/Refractory Diffuse Large B-Cell Lymphoma | 52% |
These FDA-approved CAR T cell therapies are a big step forward in lymphoma treatment. They offer new hope to patients who have tried other treatments. As research goes on, we expect even more progress in this field, leading to better treatments for patients.
Clinical Efficacy of CAR T Cell Lymphoma Treatment
CAR T cell therapy is a new hope for lymphoma patients. It works well when other treatments fail. This method has shown great results in treating lymphoma.
Response Rates in Refractory Cases
Studies show CAR T cell therapy can help patients with hard-to-treat lymphoma. It works for 50% to over 80% of patients. For example, Yescarta helped 82% of patients with refractory large B-cell lymphoma.
This therapy targets and kills cancer cells better than old treatments. It’s a big help for those who didn’t respond to other treatments.
Durability of Remission
Not only does CAR T cell therapy work well, but it also keeps patients in remission for a long time. Many patients stay disease-free for years.
A study on Kymriah showed 80% of patients with diffuse large B-cell lymphoma stayed in remission at 12 months. This long-lasting effect is key to CAR T cell therapy’s success.
| Therapy | Overall Response Rate | Complete Remission Rate | Durability of Remission |
|---|---|---|---|
| Axicabtagene Ciloleucel (Yescarta) | 82% | 58% | Up to 2 years |
| Tisagenlecleucel (Kymriah) | 52% | 40% | Up to 1.5 years |
CAR T cell therapy is a big step forward in fighting lymphoma. It offers hope to patients with hard-to-treat lymphoma. Its ability to achieve high response rates and long-lasting remissions is groundbreaking.
Side Effects and Management
CAR T cell therapy brings hope to lymphoma patients but comes with significant side effects. It’s important to know the risks and how to manage them.
Cytokine Release Syndrome
Cytokine release syndrome (CRS) is a common and serious side effect. It happens when CAR T cells release cytokines, causing inflammation. Symptoms can range from mild to life-threatening and include fever, fatigue, nausea, and in severe cases, hypotension and organ dysfunction.
Early treatment of CRS is key. We use a grading system to guide our treatment. For mild cases, we use hydration and antipyretics. But severe CRS needs quick action with tocilizumab and sometimes corticosteroids.
Neurological Toxicities
Neurological toxicity, or ICANS, is another side effect. Symptoms include confusion, tremors, dysphasia, and in severe cases, seizures or cerebral edema. The exact cause is being studied, but it’s linked to cytokine release and inflammation.
Managing ICANS involves supportive care and, in some cases, corticosteroids to reduce inflammation. Watching patients closely for early signs is critical, as quick action can greatly improve outcomes.
Management Strategies
Managing CAR T cell therapy side effects needs a team effort. We focus on patient selection, monitoring, and having a clear plan. Tocilizumab and corticosteroids are key tools for managing CRS and ICANS.
- Early recognition of side effects
- Grading the severity of CRS and ICANS
- Use of tocilizumab for CRS
- Corticosteroids for both CRS and ICANS
- Supportive care, including hydration and symptom management
Understanding CAR T cell therapy’s side effects and having good management strategies helps. As research improves, we expect better safety and effectiveness for lymphoma patients.
Patient Experience and Recovery After CAR T Cell Therapy
The journey through CAR T cell therapy doesn’t end with the infusion. It extends into a critical recovery period. Patients going through this treatment for lymphoma face a recovery phase that’s just as important as the treatment itself. The road to recovery is complex, involving careful monitoring, managing side effects, and a long-term follow-up plan.
Hospital Stay and Monitoring
After CAR T cell therapy, patients usually need to stay in the hospital for close monitoring. This period is key as it lets healthcare professionals manage any immediate side effects and ensure the patient’s safety. During the hospital stay, we watch for signs of cytokine release syndrome (CRS), a serious side effect that can happen after the infusion.
We check patients’ vital signs, run lab tests, and watch their overall condition. We also teach patients and their caregivers what to expect and how to spot any issues early.
Long-term Follow-up and Quality of Life
Long-term follow-up is a big part of CAR T cell therapy. After leaving the hospital, patients need to see their healthcare team regularly. These visits help us see how well the treatment is working and watch for any late side effects.
We also check how CAR T cell therapy affects patients’ daily lives. We look at their ability to do everyday tasks, manage fatigue, and deal with any ongoing side effects. Our goal is to help patients live the best life possible after treatment.
| Aspect of Care | Description | Importance |
|---|---|---|
| Hospital Stay | Close monitoring after CAR T cell infusion | High |
| Monitoring | Regular checks for side effects and response | High |
| Long-term Follow-up | Ongoing assessment of response and side effects | High |
| Quality of Life Assessment | Evaluation of daily life impact post-treatment | High |
Understanding the patient experience and recovery after CAR T cell therapy helps us support those undergoing this treatment better. Our care approach, from the start of hospitalization to long-term follow-up, aims to improve patient outcomes and quality of life.
Challenges and Future Directions in CAR T Cell Therapy
Exploring CAR T cell therapy, we see both bright spots and hurdles. It’s a game-changer for lymphoma treatment but has its own set of issues.
Current Limitations
Current Limitations
CAR T cell therapy has its own set of challenges. One big issue is antigen escape, where cancer cells hide from the therapy. Also, tumor heterogeneity makes it hard for CAR T cells to target all cancer cells effectively.
Side effects like cytokine release syndrome (CRS) and neurological issues are common. While treatable, they highlight the need for better treatment methods.
Next-Generation CAR T Designs
Researchers are working on new CAR T cell therapies. They aim to make them more effective and safer. One idea is dual-targeting CAR T cells, which can attack cancer cells from two angles, reducing the chance of cancer cells evading the therapy.
Another innovation is CAR T cells with built-in safety switches. These switches can turn off the therapy if severe side effects happen. Genetic engineering is also improving CAR T cells, making them last longer and work better against cancer.
“The development of next-generation CAR T cell therapies represents a critical step forward in our fight against lymphoma, opening new doors for patients with hard-to-treat disease.”
As research keeps moving forward, we expect these new CAR T cell designs to overcome many current challenges. This will lead to more effective and safer treatments for cancer patients.
Conclusion
CAR T cell therapy has changed how we treat lymphoma, giving patients new hope. This immunotherapy uses the immune system to fight cancer. It has shown great promise in trials, with some patients getting completely better.
This therapy has made a big difference in treating lymphoma. It offers a new choice for those who have tried other treatments without success. CAR T cell therapy is a big step forward in fighting cancer.
As research keeps going, we’ll see even more progress in CAR T cell therapy. It might help more types of lymphoma in the future. The outlook for lymphoma treatment is bright, with CAR T cell therapy leading the way.
What is CAR T cell therapy?
CAR T cell therapy is a way to fight cancer. It changes a patient’s T cells to find and kill cancer cells. It’s mainly used for lymphoma.
How does CAR T cell therapy work?
First, T cells are taken from the patient. Then, they are changed to find and attack cancer cells. After that, these T cells are put back into the patient to fight the cancer.
What types of lymphoma can be treated with CAR T cell therapy?
CAR T cell therapy helps with certain types of Non-Hodgkin lymphoma (NHL). This includes diffuse large B-cell lymphoma (DLBCL) and other aggressive types that don’t respond to other treatments.
What are the FDA-approved CAR T cell therapies for lymphoma?
The FDA has approved two CAR T cell therapies for lymphoma. These are axicabtagene ciloleucel (Yescarta) and tisagenlecleucel (Kymriah). They are for relapsed or refractory NHL.
What are the possible side effects of CAR T cell therapy?
Side effects can include cytokine release syndrome (CRS) and neurological issues. These can be managed with medical care and monitoring.
How is cytokine release syndrome managed?
CRS is treated with tocilizumab and corticosteroids. Supportive care is also used to lessen symptoms and prevent serious problems.
What is the patient experience like after CAR T cell therapy?
After treatment, patients need close monitoring in the hospital. They may also need long-term follow-up to check how well the treatment worked and manage any late effects.
What are the current limitations of CAR T cell therapy?
Current challenges include severe side effects, the need for chemotherapy, and high treatment costs. These are areas for improvement.
What are next-generation CAR T designs?
Next-generation CAR T cells aim to improve treatment. They might have better antigen recognition or last longer in the body. This could make the therapy safer and more effective.
How does CAR T cell therapy impact quality of life?
CAR T cell therapy can greatly improve life for lymphoma patients. It can lead to long-lasting remissions and better survival rates. But, the treatment and possible side effects can also affect quality of life.