Last Updated on October 27, 2025 by

Hematopoietic stem cell transplantation (HSCT) is a new way to treat Multiple Sclerosis (MS). It works by getting rid of the immune system’s bad parts with drugs. Then, it uses autologous hematopoietic stem cells to make a new immune system.
Studies have found that HSCT can really help MS patients. It can make the disease less active and slow it down. A study with 2,002 patients showed that HSCT lowered disease activity and relapses. For more info, check out PubMed Central.
It’s important to know the difference between autologous and allogeneic stem cell transplants. Autologous transplants use the patient’s own stem cells. Allogeneic transplants use stem cells from another person. This choice is key in finding the right treatment for MS patients.
Key Takeaways
- Hematopoietic stem cell transplantation (HSCT) is a treatment approach for Multiple Sclerosis (MS).
- HSCT involves eradicating the immune system and rebuilding it with autologous hematopoietic stem cells.
- Research has shown that HSCT can mitigate disease activity and progression in MS patients.
- The difference between autologous and allogeneic stem cell transplants is vital in determining the best treatment approach.
- HSCT has shown promise in reducing relapse rates and suppressing inflammatory activity in MS patients.
What Is HSCT? Understanding the Basics
HSCT, or Hematopoietic Stem Cell Transplantation, has grown from treating blood cancers to helping with autoimmune diseases like MS. This change shows how far medical science has come.
HSCT uses special cells called stem cells. These cells can turn into many types of body cells. The process is complex. It includes collecting stem cells, preparing the patient with chemotherapy, and infusing the stem cells back into the patient.
The Science Behind Hematopoietic Stem Cell Transplantation
HSCT works by rebooting the immune system. In diseases like MS, the immune system attacks the body’s own tissues. By using chemotherapy to weaken the immune system and then adding healthy stem cells, HSCT aims to get rid of the bad immune cells.
This method not only reduces disease activity but might also stop MS from getting worse. The idea is that by fixing the immune response, we can see big improvements in patients.
Historical Development of HSCT for Autoimmune Diseases
For over 40 years, HSCT has been a key treatment for blood and bone marrow cancers. Its use for autoimmune diseases like MS is a newer development. This shift came from better understanding how the immune system works in these conditions.
The journey of using HSCT for autoimmune diseases has seen major breakthroughs. The first successful transplants happened in the 1990s. Ever after, many studies have looked into HSCT’s safety and effectiveness for MS and other autoimmune diseases.
| Year | Milestone | Description |
|---|---|---|
| 1990s | First HSCT for Autoimmune Diseases | The first successful HSCT procedures were performed on patients with autoimmune diseases, marking the beginning of a new era in treatment. |
| 2000s | Advancements in HSCT Techniques | Significant advancements were made in HSCT techniques, including improved stem cell collection methods and conditioning regimens. |
| 2010s | Increased Use of HSCT for MS | HSCT became increasingly used for treating MS, with numerous clinical trials and studies demonstrating its promise. |
The growth of HSCT for MS shows a shift in medicine towards more tailored treatments. As research keeps advancing, HSCT is set to become even more vital in treating autoimmune diseases.
Multiple Sclerosis: Disease Mechanisms and Conventional Treatments
Multiple sclerosis (MS) is a complex disease with unpredictable symptoms. It’s important to understand its causes and treatment options. The disease occurs when the immune system attacks the central nervous system, causing damage and loss of nerve function.
The pathophysiology of MS involves a complex interplay between immune cells, cytokines, and the CNS. Autoreactive T cells and B cells play a key role in attacking myelin, the protective sheath around nerve fibers. This attack leads to inflammation, damage to the nerve sheath, and disruption of nerve signals.
Pathophysiology of MS and Immune System Involvement
The immune system plays a complex role in MS. CD4+ T cells, with Th1 or Th17 phenotypes, are key players in the autoimmune response. CD8+ T cells and B cells also contribute to the disease’s progression.
The table below summarizes the key immune cells involved in MS pathophysiology:
| Immune Cell Type | Role in MS Pathophysiology |
|---|---|
| CD4+ T cells (Th1/Th17) | Drive autoimmune response against myelin |
| CD8+ T cells | Contribute to axonal damage and disease progression |
| B cells | Produce autoantibodies against myelin and contribute to inflammation |
Limitations of Traditional MS Therapies
Traditional MS treatments aim to manage symptoms and slow disease progression. But, they have limitations. Disease-modifying therapies (DMTs) like interferons and glatiramer acetate can reduce relapse rates. Yet, they may not stop the disease from progressing completely. Their effectiveness varies among patients.
Traditional therapies also have significant side effects, affecting patients’ quality of life. This has led to the search for alternative treatments, such as hematopoietic stem cell transplantation (HSCT).
How HSCT Works for Multiple Sclerosis
HSCT treats Multiple Sclerosis by resetting the immune system. This could stop the disease from getting worse. It aims to fix the immune system’s problem that causes MS.
Targeting the Root Cause: Autoimmune Dysfunction
MS makes the immune system attack the nerve fibers’ protective covering. This disrupts communication between the brain and the body. HSCT fixes this by eradicating the existing immune cells with chemotherapy.
A study on PubMed Central shows HSCT’s promise in treating autoimmune diseases like MS. It reboots the immune system.
The Immune System “Reboot” Process
The HSCT process for MS includes several steps:
- Stem cell mobilization and collection
- Chemotherapy to eliminate existing immune cells
- Reinfusion of hematopoietic stem cells to rebuild a new immune system
This “reboot” process lets the body start over. It might reduce or stop autoimmune attacks on the central nervous system. The aim is to restore immune tolerance and protect the myelin sheath.
HSCT’s success in treating MS comes from its focus on the disease’s root cause. Knowing how HSCT works helps patients and doctors make better choices about this treatment.
Types of HSCT for MS Treatment
There are two main types of HSCT for treating Multiple Sclerosis (MS): autologous and allogeneic transplantation. Knowing the differences between these is key to finding the right treatment for patients.
Autologous HSCT (AutoSCT): Using Your Own Stem Cells
AutoSCT uses the patient’s own stem cells. It starts with collecting stem cells from the bone marrow or blood. These cells are then stored while the patient gets chemotherapy to kill off bad immune cells.
After the chemotherapy, the patient’s stem cells are put back in. This aims to create a new immune system that won’t harm the nervous system.
Advantages of AutoSCT:
- Lower risk of graft-versus-host disease (GVHD)
- Reduced need for immunosuppressive drugs post-transplant
- Potential for quicker immune reconstitution
Allogeneic HSCT (AlloSCT): Donor Stem Cell Transplantation
AlloSCT uses stem cells from a donor. This method needs a compatible donor, often a sibling or someone found through a registry. The process is similar to AutoSCT but aims to introduce a new immune system.
This new immune system might offer a stronger response against MS.
Considerations for AlloSCT:
- Higher risk of GVHD compared to AutoSCT
- Need for immunosuppressive drugs to prevent GVHD
- Potential for a graft-versus-autoimmune effect

Comparing AutoSCT vs AlloSCT Outcomes in MS
Both AutoSCT and AlloSCT show promise in treating MS. AutoSCT is safer, with less risk of GVHD. But AlloSCT might offer a more lasting solution by introducing a new immune system.
Key differences in outcomes:
- Relapse Rates: Studies show different relapse rates. AlloSCT might reduce long-term disease activity.
- Complication Rates: AutoSCT has fewer complications, like GVHD.
- Immune Reconstitution: The way immune systems recover differs. This affects the risk of infections and other issues.
Choosing between AutoSCT and AlloSCT depends on many factors. These include the patient’s health, disease severity, and donor availability. Each case is unique, and a healthcare provider should guide the decision.
The Role of Chemotherapy in HSCT for MS
Chemotherapy is used in HSCT to reset the immune system for patients with Multiple Sclerosis. It erases the current immune system. Then, new stem cells replace it. This helps get rid of immune cells that attack the body.
Conditioning Regimens: Myeloablative vs. Non-myeloablative
The conditioning regimen is key in HSCT. It prepares the body for the transplant. There are two main types: myeloablative and non-myeloablative conditioning.
Myeloablative conditioning uses strong chemotherapy. It wipes out the bone marrow’s ability to make blood cells. After, stem cells are needed to start making blood again.
Non-myeloablative conditioning uses lower doses of chemotherapy. It aims to weaken the immune system but not destroy it. This method is safer than myeloablative conditioning.
Common Chemotherapy Agents Used
Several chemotherapy agents are used in HSCT for MS. These include:
- Cyclophosphamide
- Busulfan
- Fludarabine
- Antithymocyte globulin (ATG)
These agents are picked for their ability to weaken the immune system and destroy bone marrow. This is important for the success of the HSCT.
Managing Chemotherapy Side Effects
It’s important to manage chemotherapy side effects. This ensures patients are safe and comfortable during HSCT. Common side effects include:
- Nausea and vomiting
- Hair loss
- Increased risk of infections
- Mucositis
Supportive care, like antiemetics and antibiotics, helps manage these side effects. Close monitoring and quick action are key to avoiding problems.
The Complete HSCT Procedure: From Evaluation to Infusion
Understanding the HSCT procedure is key for those with multiple sclerosis. It involves several stages, from evaluation to infusion. Each stage is vital for the treatment’s success.
Pre-Transplant Screening and Preparation
The first step is a detailed screening and preparation. This ensures patients are good candidates and reduces risks.
- Comprehensive medical evaluation to assess overall health and disease status
- Review of medical history to identify any previous treatments or conditions that may impact the HSCT procedure
- Cardiac and pulmonary function tests to evaluate organ health
- Infectious disease screening to prevent possible complications
Patients also learn about the HSCT, including risks and benefits. This is to ensure they give informed consent.
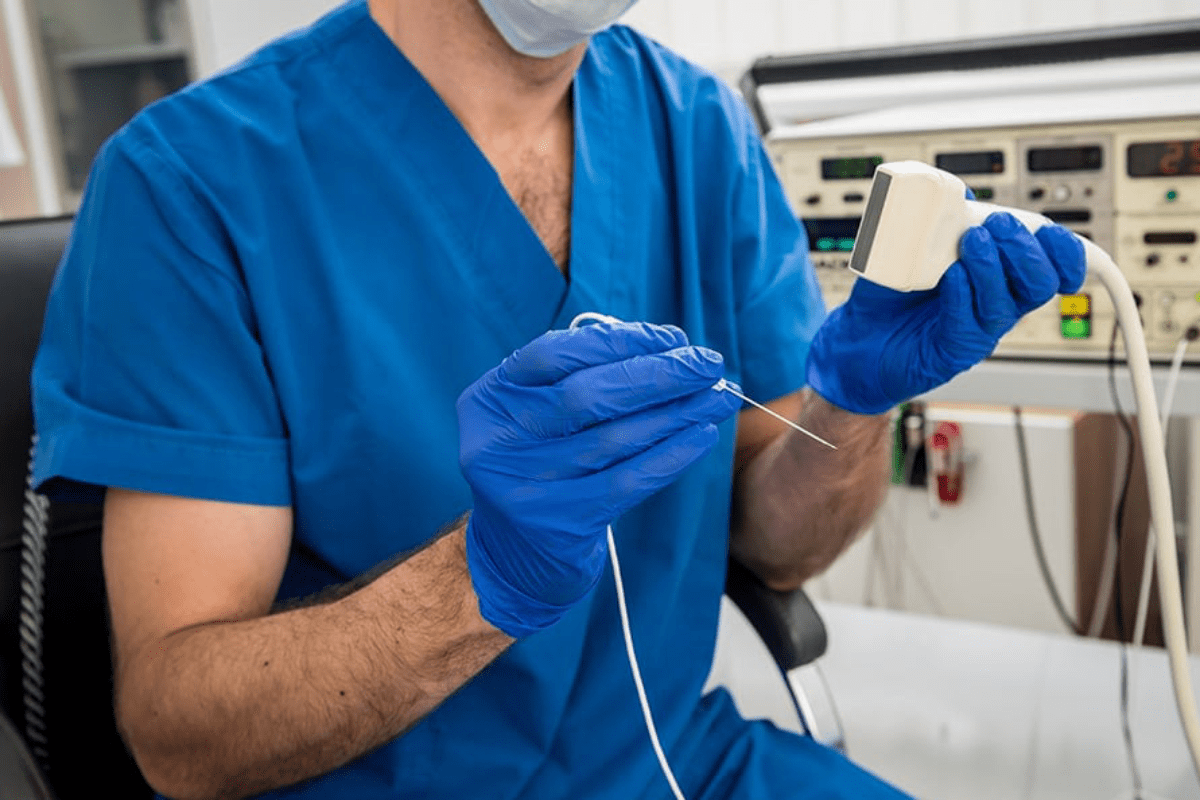
Stem Cell Mobilization and Collection
After clearance, the next step is mobilizing and collecting stem cells. This involves getting the bone marrow to release stem cells into the blood.
Stem cell mobilization uses medications to stimulate the bone marrow. The stem cells are then collected through apheresis, filtering the blood to separate the stem cells.
Conditioning Phase (Chemotherapy)
Before reinfusing the stem cells, patients undergo chemotherapy. This phase aims to:
- Suppress the immune system to prevent rejection of the transplanted stem cells
- Eradicate diseased immune cells that contribute to multiple sclerosis
- Create space in the bone marrow for the new stem cells to engraft
The chemotherapy regimen varies based on the HSCT protocol and patient condition.
Stem Cell Reinfusion and Engraftment
The final step is reinfusing the stem cells. This is like a blood transfusion, where the stem cells are infused into the bloodstream.
After infusion, the stem cells go to the bone marrow. There, they start to engraft and produce new blood cells. This process takes weeks to months, with close monitoring for complications.
The HSCT procedure is complex and tailored to each patient. Knowing each step helps patients prepare and improves their experience.
HSCT Success Rates and Effectiveness for MS
HSCT is seen as a promising treatment for MS. It’s being studied in clinical trials and through long-term data. This treatment might help patients with aggressive or treatment-resistant MS by inducing long-lasting remissions.
Clinical Trial Results and Long-term Data
Many clinical trials have looked into HSCT’s effectiveness for MS. The results show it can improve disability status and lower relapse rates for some patients.
Long-term studies suggest that some patients stay disease-free for years after the transplant. For example, a study in the Journal of Neurology, Neurosurgery, and Psychiatry found that at 5 years, many patients had not seen their disease progress.
| Study | Number of Patients | Follow-up Period | Progression-Free Survival |
|---|---|---|---|
| Burt et al. (2019) | 281 | 5 years | 62% |
| Mancardi et al. (2018) | 110 | 4 years | 55% |
| Atkins et al. (2020) | 200 | 3 years | 70% |
Factors Influencing Treatment Success
Several factors can affect how well HSCT works for MS. These include the type and severity of MS, the patient’s age, and overall health. Patients with more aggressive MS might have different results than those with less aggressive forms.
- Disease Severity: Patients with higher disease activity or more severe disability may have different outcomes.
- Age and Health Status: Younger patients with fewer comorbidities tend to have better outcomes.
- MS Subtype: The effectiveness of HSCT can vary between relapsing-remitting and progressive forms of MS.
Comparing HSCT to Other Advanced MS Treatments
It’s important to compare HSCT to other advanced MS treatments. HSCT is often considered for patients who haven’t responded well to other treatments.
HSCT works differently than other treatments like monoclonal antibodies or oral disease-modifying therapies. It can offer sustained disease control for some patients who haven’t responded to other treatments.
Potential Risks and Complications of HSCT
HSCT offers hope for some MS patients. But, it’s important to know the risks. This procedure can have serious side effects, both short-term and long-term.
Short-term Side Effects and Management
Short-term side effects of HSCT can be tough for patients. These include:
- Infections due to immunosuppression
- Nausea and vomiting from chemotherapy
- Fatigue and weakness
- Hair loss
- Mucositis (inflammation of the mucous membranes)
It’s key to manage these side effects. This helps patients feel better and avoid more problems. Ways to do this include:
- Prophylactic antibiotics and antiviral medications
- Anti-nausea medications
- Nutritional support
- Growth factor support to stimulate blood cell production
Long-term Risks and Considerations
HSCT can treat MS, but there are long-term risks. These include:
- Risk of secondary malignancies (new cancers)
- Organ damage (e.g., to the heart, lungs, or liver)
- Infertility or gonadal failure
- Immunosuppression leading to opportunistic infections
- Graft failure or relapse of MS
It’s vital to have long-term follow-up care. This helps monitor for these risks.
Mortality Rates and Risk Factors
HSCT carries a risk of death. This is mainly due to infections, organ failure, or graft-versus-host disease. The risk varies based on several factors, including:
| Risk Factor | Impact on Mortality |
|---|---|
| Age of the patient | Increased age generally increases risk |
| Type of HSCT (autologous vs. allogeneic) | Allogeneic HSCT typically carries higher risk |
| Underlying health conditions | Presence of other health issues can increase risk |
| Conditioning regimen intensity | Myeloablative conditioning is more intense and risky |
Knowing these risk factors is key for choosing patients and getting informed consent.
Patient Selection: Who Should Consider HSCT for MS?
Choosing the right patients for HSCT in MS treatment is complex. It looks at several important factors. These include the type of MS, how active the disease is, the patient’s age, health, and other criteria.
Ideal Candidates Based on MS Type and Disease Activity
Those with aggressive or very active MS who haven’t done well with usual treatments are top candidates. This includes people with relapsing-remitting MS (RRMS) who keep having relapses. Also, those with secondary progressive MS (SPMS) who are showing signs of ongoing inflammation might be considered.
Key characteristics of ideal candidates include:
- High disease activity despite being on disease-modifying therapies
- Presence of gadolinium-enhancing lesions on MRI, indicating active inflammation
- Frequent relapses or significant disability progression
Age, Health Status, and Other Eligibility Factors
Age and health are big factors in deciding if someone can get HSCT. Younger people with fewer health problems usually do better. Doctors do detailed checks to see if the patient’s organs are working well, if they’re at risk for infections, and if they can handle the treatment.
| Eligibility Factor | Description | Importance |
|---|---|---|
| Age | Generally, younger patients have better outcomes | High |
| Health Status | Presence of comorbidities can affect eligibility | High |
| Disease Activity | High disease activity is a key indicator for HSCT consideration | High |
| Previous Treatments | Failure or intolerance to multiple disease-modifying therapies | Medium |
When HSCT May Not Be Recommended
HSCT isn’t right for everyone with MS. Those with very advanced disease, a lot of disability, or health problems might face too many risks. Also, people with primary progressive MS (PPMS) who don’t show much inflammation might not get much benefit from HSCT.
It’s very important for patients to talk to their doctors about their specific situation. This helps figure out if HSCT is a good choice for them.
Recovery and Life After HSCT
The recovery after HSCT for MS is complex. It involves immediate care and long-term follow-up. This ensures the best outcomes. It covers both physical and emotional recovery.
Immediate Post-Transplant Recovery Period
The first recovery phase is key. It focuses on managing side effects and complications. Patients need close monitoring for infections and graft-versus-host disease. Managing these issues well is vital for success.
During this time, patients often stay in the hospital. This makes it easier to get medical care. The team watches blood counts, organ function, and overall health closely.
Long-term Follow-up and Monitoring
After the first recovery, long-term follow-up is vital. It tracks disease activity and late transplant effects. Regular check-ups help catch and manage complications early. Follow-up care is personalized, based on age, health, and MS and HSCT specifics.
Patient Experiences and Quality of Life Improvements
Many patients see big improvements in their quality of life after HSCT. Some see a stop in disease progression. The treatment can reduce symptoms and improve physical function. Sharing experiences and connecting with others can offer great support.
Managing Expectations: Possible Outcomes
It’s important to manage expectations, as outcomes vary. The type of MS, disease severity, and overall health affect success. Understanding outcomes well can help prepare patients and their families.
Conclusion: The Future of HSCT in MS Treatment
Hematopoietic Stem Cell Transplantation (HSCT) is becoming a hopeful treatment for Multiple Sclerosis (MS). It gives new hope to those with this chronic disease. As research grows, HSCT’s role in MS treatment looks very promising.
Studies are working to make HSCT safer, more effective, and easier to get for MS patients. Improvements in stem cell therapy aim to better treatment results. This makes HSCT a possible choice for more people.
HSCT’s role in treating MS is getting bigger. More evidence shows it works well for some patients. As the field keeps growing, HSCT will likely be a big part of MS treatment plans.
With ongoing research and stem cell therapy advancements, HSCT’s future in MS treatment is bright. As we learn more about MS, HSCT will play a key role. It offers new chances for patients and doctors.
FAQ
What is HSCT and how is it used to treat Multiple Sclerosis?
HSCT, or Hematopoietic Stem Cell Transplantation, is a treatment that uses chemotherapy to weaken the immune system. Then, it rebuilds it with stem cells. For Multiple Sclerosis, it aims to “reboot” the immune system, targeting the root cause of the disease.
What are the differences between autologous and allogeneic HSCT?
Autologous HSCT uses a patient’s own stem cells. Allogeneic HSCT uses donor stem cells. Autologous HSCT is more common for MS treatment because it lowers the risk of graft-versus-host disease.
How does chemotherapy work in HSCT for MS?
Chemotherapy weakens the immune system, getting rid of faulty immune cells that cause MS. There are different ways to do this, like myeloablative and non-myeloablative approaches.
What are the possible risks and complications of HSCT for MS?
Risks include short-term side effects like infections and fatigue. Long-term risks include infertility and secondary cancers. There’s also a risk of death from the procedure.
Who is a good candidate for HSCT in MS treatment?
Good candidates usually have aggressive or rapidly progressing MS. They should have tried other treatments without success. Age, health, and disease activity are considered when deciding if someone is eligible.
What is the success rate of HSCT for MS?
Success rates vary, with some studies showing big improvements in disability and quality of life. How well the treatment works depends on the disease’s severity and the patient’s health.
How does HSCT compare to other advanced MS treatments?
HSCT is seen as a potentially effective treatment for MS, mainly for aggressive or treatment-resistant cases. It’s compared to other advanced therapies, like disease-modifying drugs.
What is the recovery process like after HSCT for MS?
Recovery starts with an immediate post-transplant period. It then involves long-term follow-up and monitoring. Patients may see improvements in quality of life, but it’s important to manage expectations.
What is the role of stem cell mobilization and collection in HSCT?
Mobilizing and collecting stem cells are key steps in HSCT. Medications are used to release stem cells, which are then collected for reinfusion.
What are the possible long-term benefits of HSCT for MS?
Long-term benefits include sustained improvements in disability and quality of life. There’s also a chance of halting disease progression.
Is HSCT a cure for Multiple Sclerosis?
HSCT is not a cure for MS. It’s a treatment that can significantly impact disease activity and quality of life.
What is the future of HSCT in MS treatment?
Research and advancements in HSCT techniques and patient selection are ongoing. This could lead to better outcomes and more treatment options for MS patients.
References
- Approximately 68% of patients achieve No Evidence of Disease Activity (NEDA) after AHSCT. PubMed
- The overall survival rate post-transplant is around 94%, with a 4% risk of transplant-related mortality. PubMed
- AHSCT has shown potential in altering the course of progressive MS and may delay or prevent its onset. BioMed Central