Hematopoiesis is the process of making blood cells. It’s complex and happens in different places as we grow. Knowing where it happens is key to treating blood diseases. At Liv Hospital, we focus on top-notch care for our patients.
In our development, hematopoiesis happens in the yolk sac, fetal liver, and bone marrow. The bone marrow is where it mainly happens in adults. We use the latest research to help our patients.
Key Takeaways
- Hematopoiesis occurs in different sites during human development.
- The yolk sac, fetal liver, and bone marrow are the primary locations.
- Bone marrow is the main site of hematopoiesis in adults.
- Understanding hematopoiesis is key to treating blood disorders.
- Liv Hospital provides advanced care for patients with blood disorders.
The Fundamentals of Hematopoiesis
Hematopoiesis is the process of making blood cells. It’s vital for our health. It creates red blood cells, white blood cells, and platelets. These cells carry oxygen, fight infections, and help blood clot.
Understanding hematopoiesis helps us see how our bodies keep blood cells in balance. We’ll look at what blood cell formation is, the role of hematopoietic stem cells, and the different types of blood cells.
Definition and Importance of Blood Cell Formation
Blood cell formation, or hematopoiesis, turns hematopoietic stem cells into different blood cells. It’s key for replacing old or damaged cells and meeting the body’s needs. For example, it boosts white blood cells to fight infections.
This process is very important. Problems with it can cause anemia, leukemia, and lymphoma. Knowing how it works helps us find treatments for these diseases.
Overview of Hematopoietic Stem Cells
Hematopoietic stem cells (HSCs) are the starting point for all blood cells. They can make more of themselves and turn into any blood cell type. This makes them essential for making blood cells throughout our lives. They live in the bone marrow, where they get support from a special environment.
Keeping HSCs in balance is key. They need to keep making more of themselves and turn into blood cells. This balance is important to avoid blood disorders.
The Myeloid and Lymphoid Lineages
HSCs split into two main paths: the myeloid and lymphoid lineages. The myeloid lineage makes red blood cells, platelets, and immune cells. These cells carry oxygen, help blood clot, and fight infections.
| Lineage | Cell Types Produced | Functions |
|---|---|---|
| Myeloid | Red blood cells, platelets, monocytes/macrophages, neutrophils, basophils, eosinophils | Oxygen transport, blood clotting, innate immunity |
| Lymphoid | T cells, B cells, natural killer cells | Adaptive immunity |
The lymphoid lineage makes T cells, B cells, and natural killer cells. These cells are vital for our immune system. Both lineages are important for our health and immune response.
Embryonic Origins: Yolk Sac Hematopoiesis
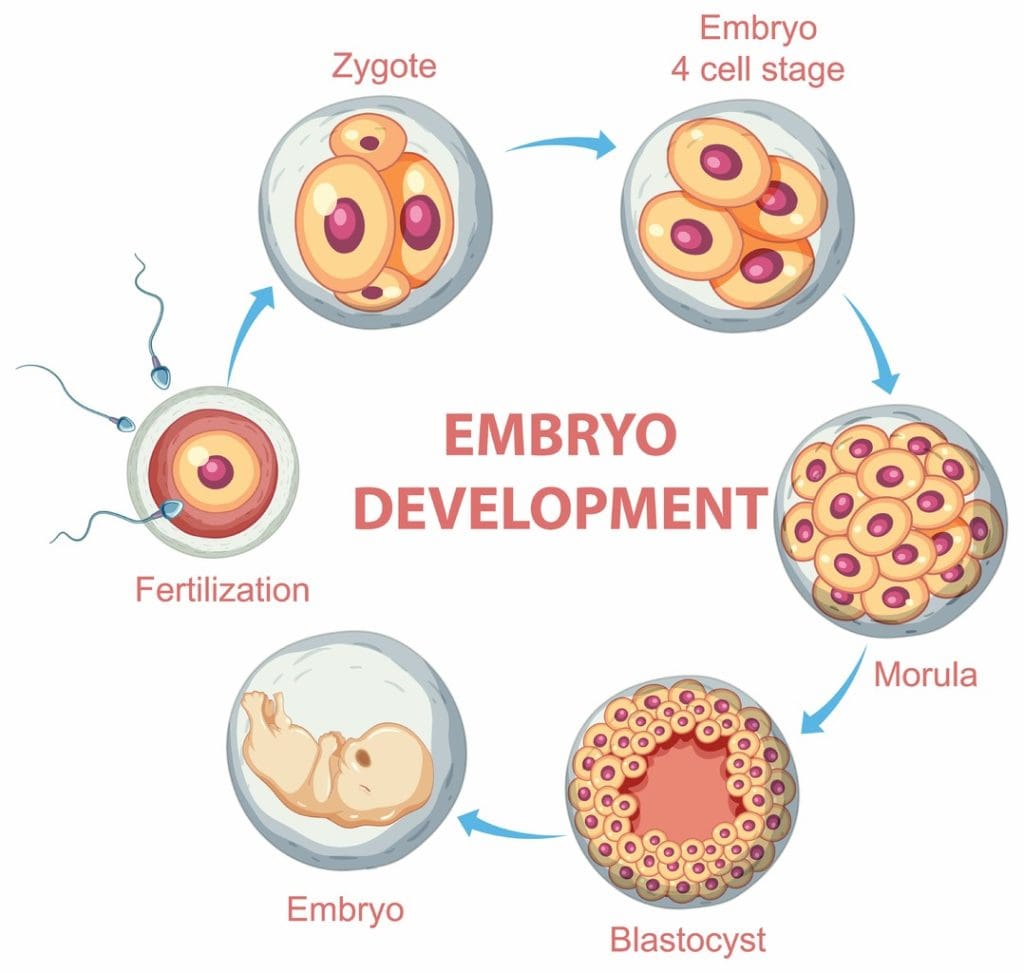
The yolk sac is key in the early stages of blood cell formation in embryos. It’s the first place where blood cells start to form. This sets the stage for all future blood cell development.
Primitive Blood Cell Formation
Primitive blood cell formation in the yolk sac is vital. This process starts with mesodermal cells turning into blood cells. It marks the start of blood cell development.
The yolk sac’s role in blood cell formation is short but very important. The blood cells it produces help with oxygen and nutrient delivery early on.
Timeline of Yolk Sac Activity
The yolk sac starts making blood cells around the third week of pregnancy. It keeps doing this until about the eighth week. During this time, it’s the main source of blood cells for the embryo.
As the embryo grows, the job of making blood cells shifts. It moves to places like the fetal liver. This change is key for the ongoing production of blood cells and the growth of the blood system.
Types of Blood Cells Produced
The yolk sac makes early blood cells like erythrocytes and macrophages. These cells are essential for oxygen delivery and immune protection in the developing embryo.
Making these cells in the yolk sac is a complex process. It involves many growth factors and transcription factors working together. Understanding this helps us see how important the early stages of blood cell development are.
Hematopoiesis Is Carried Out in the Fetal Liver
As the embryo grows, hematopoiesis moves from the yolk sac to the fetal liver. This change is key for the hematopoietic system’s development. By the 7th week, the fetal liver takes over as the main hematopoiesis site.
Transition from Yolk Sac to Liver
The move from yolk sac to liver hematopoiesis is complex. Hematopoietic stem cells migrate to the liver. They are vital for creating all blood cell types.
This transition is vital for the hematopoietic system’s proper growth. It allows for the creation of various blood cells. The liver’s role in hematopoiesis is temporary but essential for bone marrow development.
Peak Activity During Weeks 7-22
From weeks 7-22, the fetal liver is most active in hematopoiesis. This time sees a big increase in blood cell production. It meets the growing needs of the fetus.
- The liver makes many red blood cells, white blood cells, and platelets.
- Hematopoietic stem cells in the liver turn into different blood cell types.
- The liver’s hematopoietic role is supported by a complex environment.
Cellular Composition and Function
The fetal liver’s cells are diverse during this time. It includes hematopoietic stem cells, progenitor cells, and mature blood cells. The liver’s hematopoietic function is vital for the fetus’s development. It provides the necessary blood cells for oxygen transport, immune defense, and more.
The fetal liver’s hematopoietic activity prepares for bone marrow’s role after birth. Bone marrow will then be the main site for blood cell production.
Other Temporary Fetal Hematopoietic Sites
As the fetus grows, other organs take on hematopoietic roles. The spleen, thymus, and even placenta play big parts in the hematopoietic system’s development.
The Role of the Spleen in Fetal Blood Formation
The spleen is key in fetal blood formation. It makes lymphocytes and other blood cells, adding to the lymphoid lineage. Its role is vital until the bone marrow takes over.
Thymus and Lymphoid Development
The thymus is vital for the immune system, helping T lymphocytes mature. It’s a key site for lymphoid development, supporting the hematopoietic process. This ensures immune cells work right.
Placental Contribution to Hematopoiesis
Studies show the placenta also helps with hematopoiesis. It supports hematopoietic stem cells and may regulate the hematopoietic system. The placenta’s role shows the complexity and redundancy of hematopoietic sites in fetal development.
Transition to Bone Marrow Hematopoiesis
Bone marrow becomes the main place for making blood cells later in human life. This change is key for a lifelong supply of blood-making stem cells.
Developmental Timeline
The switch to bone marrow for blood cell making happens late in fetal life. By birth, bone marrow takes over this role. This is vital for a stable blood-making system.
Research shows bone marrow starts its role in the last three months of pregnancy. As the fetus grows, bone marrow takes over blood cell production. This was done by the yolk sac and liver before.
Mechanisms of Hematopoietic Stem Cell Migration
The move of blood-making stem cells to bone marrow is complex. They are guided by signals to the bone marrow niche.
Chemokines and adhesion molecules are thought to play a big part in this journey. Learning about these can help us understand blood cell making better.
Establishment of the Bone Marrow Niche
The bone marrow niche is a special area for blood-making stem cells. It’s key for keeping blood cell making going.
This niche has different cells like osteoblasts and endothelial cells. They work together to help stem cells. This balance is important for their growth and function.
| Developmental Stage | Primary Site of Hematopoiesis | Key Features |
|---|---|---|
| Early Embryonic Development | Yolk Sac | Primitive blood cell formation |
| Fetal Development (Weeks 7-22) | Liver | Definitive hematopoiesis, peak activity |
| Late Fetal Development to Birth | Bone Marrow | Establishment of lifelong hematopoiesis |
Structure and Function of Bone Marrow
Bone marrow is a complex tissue that plays a key role in the hematopoietic system. It produces blood cells, which are vital for oxygen delivery, fighting infections, and preventing bleeding.
We will dive into the details of bone marrow, starting with its anatomy. Bone marrow is found in the cavities of bones, mainly in spongy bone tissue. It’s a soft, spongy tissue where blood cells are made.
Anatomy of Bone Marrow
The anatomy of bone marrow includes a network of blood vessels and various cell types. The bone marrow cavity is surrounded by bone. Inside, there’s a rich network of sinusoids and a diverse cell population.
Bone marrow is very vascular, meaning it has a lot of blood vessels. This is key for bringing oxygen and nutrients to cells and removing waste.
Cellular Components and Microenvironment
Bone marrow contains hematopoietic stem cells, which create all blood cell types. The microenvironment of the bone marrow supports these stem cells. It includes different cell types and the extracellular matrix.
The microenvironment is vital for regulating blood cell production. It gives the necessary signals and support for stem cells to grow and mature into blood cells.
Red vs. Yellow Marrow Distribution
Bone marrow is divided into red and yellow types based on its composition and function. Red marrow is actively involved in blood cell production, making red blood cells, white blood cells, and platelets. Yellow marrow, mostly fat cells, doesn’t produce blood cells.
In adults, red marrow is mainly in the pelvis, vertebrae, sternum, and cranium. Yellow marrow is in the long bones of the limbs. The mix of red and yellow marrow changes with age, with more red marrow in children.
Bone Marrow as the Primary Site in Infancy and Childhood
The bone marrow is key for making blood cells in babies and young children. It changes a lot as they grow. This shows how important it is for their health.
Distribution of Active Bone Marrow in Infants
In babies, bone marrow is all over their bones. This includes long bones, the pelvis, and vertebrae. It’s needed because babies grow fast and need lots of blood cells.
At birth, almost all bone marrow is ready to make blood cells. As they get older, some of this marrow turns into fat cells. This change is because they grow and don’t need as many blood cells.
Cellular Composition of Infant Bone Marrow
Baby bone marrow has lots of cells that make blood. These cells are very important. They help make red blood cells, white blood cells, and platelets.
Research shows baby bone marrow has more cells that make blood than adult bone marrow. This means babies have a strong ability to make blood cells.
“The presence of a high number of hematopoietic stem cells in infant bone marrow showcases its vital role in supporting the rapid growth and development during this period.”
Changes Throughout Childhood Development
As kids get older, their bone marrow changes too. By 4-5 years old, more of it turns into fat cells. This is because they grow slower and need fewer blood cells.
| Age Group | Red Marrow Distribution | Hematopoietic Activity |
|---|---|---|
| Infancy (0-1 year) | Widespread, including long bones | High |
| Early Childhood (1-5 years) | Stil widespread, starting to convert | High, but decreasing |
| Late Childhood (5+ years) | Mainly in pelvis, vertebrae, and sternum | Moderate |
Knowing these changes helps us understand how bone marrow works in kids. It shows how it supports their growth and health.
Adult Hematopoiesis: The Axial Skeleton
In adults, the process of making blood cells happens mainly in the axial skeleton. This is key for keeping the right amount of blood cells in the body. The bones in the axial skeleton create the perfect place for blood cell production.
Primary Sites: Pelvis, Sternum, Vertebrae, and Cranium
The pelvis, sternum, vertebrae, and cranium are where blood cell production happens in adults. These bones have bone marrow, a spongy tissue that makes blood cells.
- The pelvis is a major site for hematopoiesis, containing a significant amount of bone marrow.
- The sternum, or breastbone, is another key location.
- The vertebrae, which form the spine, also play a critical role.
- The cranium, or skull, is involved in hematopoiesis as well.
Cellular Composition of Adult Bone Marrow
Adult bone marrow is filled with different cells. Hematopoietic stem cells are the main ones. They can turn into any blood cell type. The bone marrow environment helps these cells grow and mature into blood cells.
The cells in bone marrow include:
- Hematopoietic stem cells, which can become any blood cell type.
- Progenitor cells, which are more specific to certain blood cell types.
- Mature blood cells, like red and white blood cells, and platelets.
Regulation of Adult Hematopoiesis
Adult hematopoiesis is controlled by many factors. Growth factors, cytokines, and the bone marrow environment all play a part. They work together to make sure the right amount of blood cells are produced.
Important parts of this regulation include:
- The role of growth factors in helping hematopoietic stem cells grow and change.
- The effect of cytokines on blood cell development and function.
- The role of the bone marrow niche in supporting hematopoietic stem cells.
Extramedullary Hematopoiesis in Pathological Conditions
Pathological conditions can trigger extramedullary hematopoiesis, reviving fetal hematopoietic sites. This reactivation is a complex process. It involves the hematopoietic system adapting to the body’s needs under stress.
Reactivation of Fetal Hematopoietic Sites
In certain disease states, the body may reactivate fetal hematopoietic sites. This is to compensate for the bone marrow’s inability to meet the demand for blood cells. Organs like the liver and spleen, which played roles in hematopoiesis during fetal development, can be involved.
Experts note, “In conditions where the bone marrow is severely compromised, extramedullary hematopoiesis can become a vital compensatory mechanism.” (
This adaptive response highlights the body’s ability to revert to earlier developmental pathways to maintain homeostasis.
)
Common Causes of Extramedullary Hematopoiesis
Several pathological conditions can lead to extramedullary hematopoiesis, including:
- Myelofibrosis, a condition characterized by the scarring of the bone marrow.
- Hemolytic anemia, where red blood cells are destroyed faster than they can be made.
- Cancer metastasis to the bone marrow, disrupting its function.
| Condition | Description | Impact on Hematopoiesis |
|---|---|---|
| Myelofibrosis | Scarring of the bone marrow | Leads to extramedullary hematopoiesis as the body compensates for reduced bone marrow function. |
| Hemolytic Anemia | Rapid destruction of red blood cells | Increases demand for blood cell production, potentially leading to extramedullary hematopoiesis. |
Clinical Significance and Management
Understanding extramedullary hematopoiesis is key for managing patients with hematological disorders. For more information on what triggers hematopoiesis, visit https://int.livhospital.com/what-triggers-hematopoiesis/.
The clinical significance of extramedullary hematopoiesis lies in its implications for patient diagnosis and treatment. Managing underlying conditions and supporting the body’s hematopoietic needs are key strategies.
Modern Approaches to Hematopoietic Disorders
New research on hematopoietic stem cells is changing how we diagnose and treat blood disorders. We’re seeing big changes in managing these conditions. This is thanks to better diagnostic tools and treatment plans.
Diagnostic Techniques
Today’s diagnostic tools are more advanced. They help find blood disorders early and accurately. Next-generation sequencing (NGS) is a key tool for spotting genetic issues. Flow cytometry also helps identify and study blood and bone marrow cells.
These tools help doctors create treatment plans that fit each patient’s needs. Knowing the genetic and cellular details of a condition helps predict how it will progress and how well it will respond to treatment.
Treatment Strategies
Treatment for blood disorders has evolved, focusing more on personalized care. Hematopoietic stem cell transplantation is a mainstay treatment for many conditions. It can even cure some. New transplant techniques and better donor matching have made this treatment more accessible.
New targeted therapies offer hope for patients with specific blood disorders. These therapies aim to attack the disease directly, sparing healthy cells and tissues.
Advances in Hematopoietic Stem Cell Transplantation
Hematopoietic stem cell transplantation has made big strides, leading to better outcomes for patients. Using haploidentical donors has opened up more donor options for patients. This is important for those without a matched donor.
Improvements in post-transplant care have also cut down on complications and boosted survival rates. New immunosuppressive methods and better supportive care are part of this progress.
As we learn more about hematopoiesis and hematopoietic stem cells, we’ll see more breakthroughs in treating blood disorders. These advancements promise better patient outcomes and quality of life.
Conclusion
We’ve looked into how blood cells are made, from the yolk sac in the womb to the bone marrow in adults. This journey shows how important each stage is in making blood cells.
The move from the yolk sac to the liver and then to the bone marrow shows how blood cell creation changes. In adults, the bone marrow is key for making blood cells. The bones in our spine are important for this process.
Knowing how blood cells are made helps us understand blood diseases better. It also shows why bone marrow is vital for healthy blood cells. As we learn more, we can find new ways to treat blood diseases.
What is hematopoiesis, and where is it carried out throughout human development?
Hematopoiesis is the process of making blood cells. It happens in different places in our bodies at different times. These places include the yolk sac, fetal liver, spleen, thymus, bone marrow, and other organs.
What is the role of hematopoietic stem cells in blood cell formation?
Hematopoietic stem cells are key in making all types of blood cells. They do this through a complex process. This process involves many cellular and molecular interactions.
What is the significance of the yolk sac in primitive blood cell formation?
The yolk sac is the first place where blood cells are made in an embryo. It produces essential blood cells. These cells help start the hematopoietic system.
How does hematopoiesis transition from the yolk sac to the fetal liver?
As the embryo grows, blood cell formation moves from the yolk sac to the fetal liver. The fetal liver becomes the main place for making blood cells in the second trimester of pregnancy.
What is the role of the bone marrow in hematopoiesis?
In adults, the bone marrow is where blood cells are made. It does this throughout our lives. The bone marrow has a complex environment that helps hematopoietic stem cells work.
How does the distribution of bone marrow change throughout childhood development?
In babies and young children, where bone marrow is active changes. It moves from being spread out to being more focused in the bones of the trunk and head.
What are the primary sites of hematopoiesis in adults?
In adults, the main places for making blood cells are the pelvis, sternum, vertebrae, and cranium. These areas have active bone marrow that produces blood cells.
What is extramedullary hematopoiesis, and what are its clinical implications?
Extramedullary hematopoiesis is when blood cells are made in places outside the bone marrow. This can happen in response to illness. It has important clinical implications.
What are the latest advances in the diagnosis and treatment of hematopoietic disorders?
New diagnostic tools, like molecular and imaging technologies, have improved finding and treating blood disorders. Treatments, such as hematopoietic stem cell transplantation, have also gotten better.
What is the significance of understanding hematopoiesis in human development?
Knowing about hematopoiesis helps us understand how blood cells are made. It’s key for developing good treatments for blood disorders. It also shows the importance of blood cells in our bodies.
References
- National Center for Biotechnology Information. (n.d.). Hematopoiesis [Book]. In NCBI Bookshelf. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK544245/
- (n.d.). PMC Article PMC3666375. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC3666375/
- Wikipedia contributors. (2025). Haematopoiesis. In Wikipedia. Retrieved October 11, 2025, from https://en.wikipedia.org/wiki/Haematopoiesis
- Kenhub. (n.d.). Histology of hematopoiesis. Retrieved from https://www.kenhub.com/en/library/anatomy/histology-of-hematopoiesis
- HistologyGuide. (n.d.). Hematopoiesis slide box. Retrieved from https://histologyguide.com/slidebox/08-hematopoiesis.html