Last Updated on December 4, 2025 by Ugurkan Demir
Learn what is atherosclerosis , how it develops, and how it differs from arteriosclerosis.
Atherosclerosis is a chronic disease that causes atheromatous plaques to build up in arteries. This buildup narrows the arteries and reduces blood flow to important organs. It’s a serious issue because it can quietly get worse over time. This could lead to heart attacks and strokes, which are life-threatening.
At Liv Hospital, we know it’s important to tell the difference between atherosclerosis and arteriosclerosis. These terms are often mixed up. Knowing the difference helps us make better health choices and take care of our hearts.
We focus on patient care and use proven methods to treat atherosclerosis. Our goal is to help patients live better lives by managing this condition well.
Key Takeaways
- Atherosclerosis is a chronic inflammatory condition affecting arterial walls.
- The buildup of atherosclerotic plaques can lead to artery narrowing.
- Distinguishing between atherosclerosis and arteriosclerosis is key to correct diagnosis and treatment.
- Liv Hospital is dedicated to patient-centered care and evidence-based practices.
- Early recognition and management of atherosclerosis can greatly improve patient outcomes.
Understanding Cardiovascular Disease: The Basics
Cardiovascular disease is a big killer worldwide, affecting health globally. It includes many heart and blood vessel problems, with atherosclerosis being a key issue.
Atherosclerosis is a big reason for heart disease deaths in rich countries. The World Health Organization (WHO) says heart diseases kill about 17.9 million people every year. This makes them the top cause of death worldwide.
The Global Impact of Cardiovascular Conditions
Cardiovascular disease hits some places and people harder than others. This is because of lifestyle, genes, and healthcare access.
| Region | Cardiovascular Disease Mortality Rate |
| Global | 17.9 million deaths annually |
| High-income countries | 3.6 million deaths annually |
| Low- and middle-income countries | 14.3 million deaths annually |
The Role of Arterial Health in Overall Wellness
Keeping our arteries healthy is key to staying well. Our arterial condition affects our heart health. We need to make healthy choices and sometimes get medical help to keep our arteries in good shape.
“The health of our arteries is fundamental to our overall cardiovascular well-being. Atherosclerosis, a condition characterized by the buildup of plaque in the arteries, is a major risk factor for cardiovascular disease.”
Learning about cardiovascular disease and the role of arteries helps us fight it. We can work to lessen its effects and make the world a healthier place.
What Is Atherosclerosis? Definition and Overview

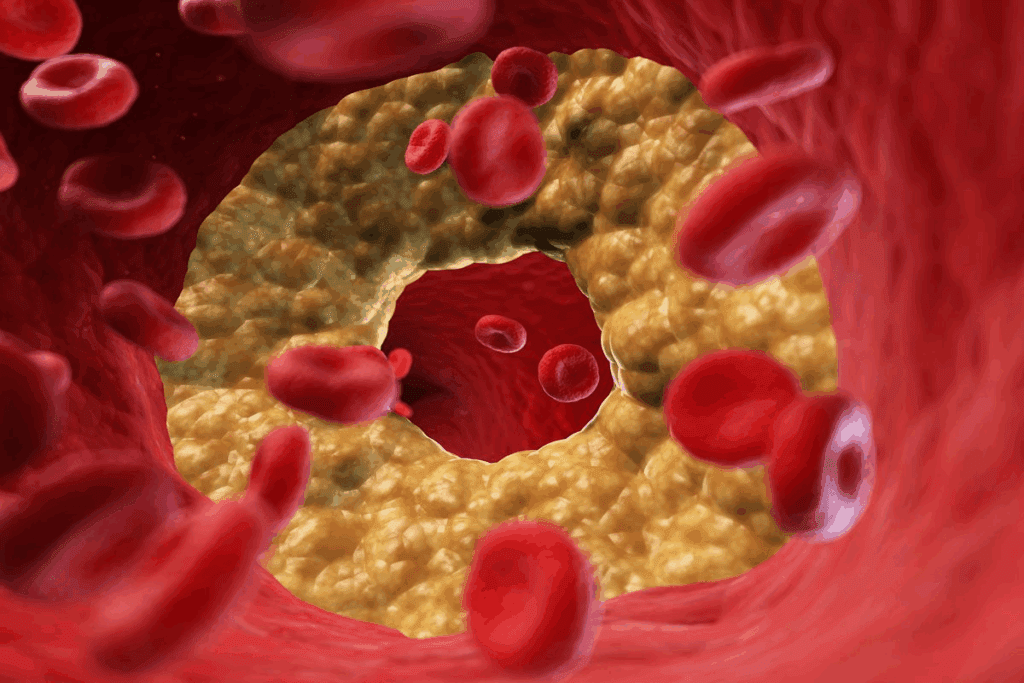
Atherosclerosis is a condition where plaques build up in the arteries. These plaques are made of fat, cholesterol, calcium, and more. This buildup causes the arteries to harden and narrow, affecting heart health.
The Inflammatory Nature of Atherosclerosis
Atherosclerosis is an inflammatory disease. The inflammation in the arteries is key to forming and growing plaques. The inflammatory response is caused by high LDL cholesterol, high blood pressure, and smoking.
The role of inflammation in atherosclerosis is complex. It involves many cells and substances that help plaques form and grow. Knowing this helps us find better treatments.
Atheromatous Plaque Composition
Atheromatous plaques are made of lipids, inflammatory cells, smooth muscle cells, and calcium. The mix of these elements can change, affecting how stable the plaque is.
| Component | Description | Impact on Plaque Stability |
| Lipids | Mainly cholesterol and cholesterol esters | Increases risk of rupture |
| Inflammatory Cells | Macrophages and T lymphocytes | Contributes to inflammation and instability |
| Calcium Deposits | Calcification within the plaque | Can stabilize or destabilize the plaque |
The makeup of atheromatous plaques is key to understanding their risk. By looking at the components and their effects, doctors can improve treatment for atherosclerosis.
What Is Arteriosclerosis? Definition and Overview
Arteriosclerosis is a disease that makes arteries thick and hard. This can block blood flow and cause heart problems. We’ll look at what arteriosclerosis is, its types, and how arteries harden.
Types of Arteriosclerosis
There are several types of arteriosclerosis, each with its own features. The main ones are:
- Atherosclerosis: This is the most common, where plaques build up in the arteries.
- Arteriolosclerosis: It’s when the small arteries harden, affecting blood pressure.
- Monckeberg’s Sclerosis: A rare condition where the arteries calcify.
General Arterial Hardening Processes
The hardening of arteries in arteriosclerosis involves several steps. These include inflammation, calcification, and the buildup of lipids and other substances. The table below shows the main differences between the types of arteriosclerosis:
| Type | Characteristics | Primary Effects |
| Atherosclerosis | Plaque buildup in arterial walls | Reduced blood flow, increased risk of thrombosis |
| Arteriolosclerosis | Hardening of small arteries | Hypertension, renal impairment |
| Monckeberg’s Sclerosis | Calcification of arterial media | Arterial stiffness, possible ischemia |
Knowing these processes helps doctors diagnose and treat arteriosclerosis better.
Atherosclerosis vs. Arteriosclerosis: Key Differences
Atherosclerosis and arteriosclerosis both affect the arteries but in different ways. Knowing these differences is ketoor correct diagnosis and treatment.
Comparing Pathological Processes
Atherosclerosis is when fatty plaques build up in the arteries, causing inflammation. This can lead to serious problems like plaque rupture. Arteriosclerosis, on the other hand, is about the arteries becoming hard and thick. This can happen due to aging, high blood pressure, or diabetes.
Key differences in pathological processes include:
- Atherosclerosis involves lipid accumulation and inflammation.
- Arteriosclerosis encompasses a broader range of arterial hardening processes.
Diagnostic Distinctions
Diagnosing these conditions requires different methods. Atherosclerosis is often spotted through imaging like angiography or ultrasound. These methods show plaque buildup. Arteriosclerosis, though, is diagnosed based on symptoms and how stiff the arteries are.
| Condition | Pathological Process | Diagnostic Approach |
| Atherosclerosis | Lipid-rich plaque buildup, inflammation | Imaging (angiography, ultrasound) |
| Arteriosclerosis | Arterial hardening, thickening | Clinical assessment, arterial stiffness measurement |
By knowing the difference between atherosclerosis and arteriosclerosis, doctors can give better treatment. This helps improve patient results.
The Pathophysiology of Atherosclerosis
To understand atherosclerosis, we must look at how plaque forms and arteries get inflamed. This condition is complex, involving many factors at the cellular, molecular, and hemodynamic levels.
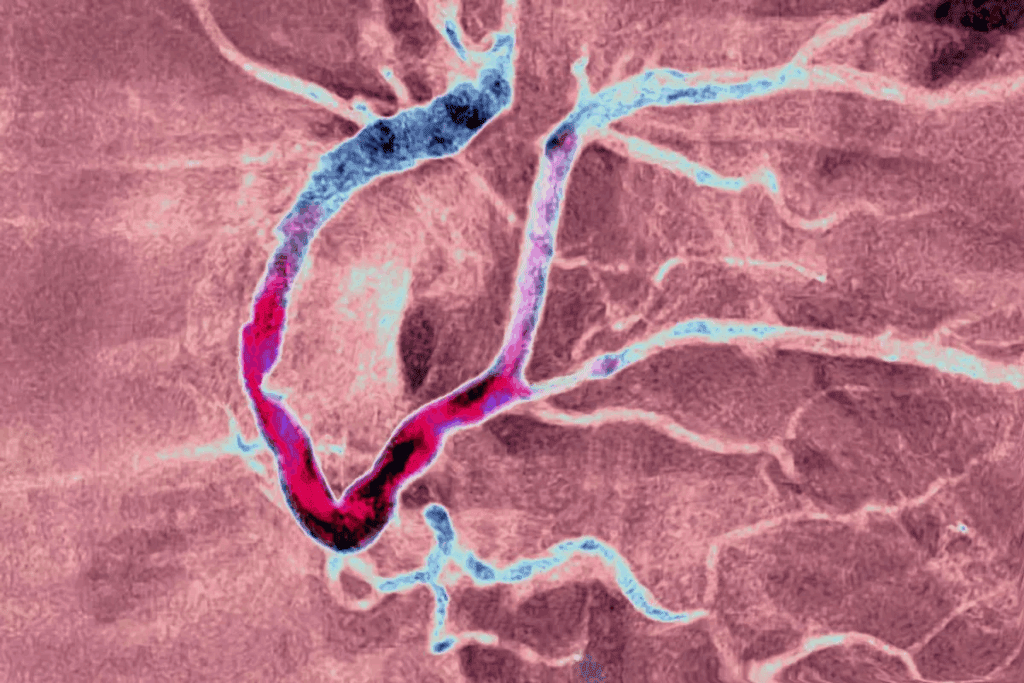
The Inflammatory Response in Arterial Walls
The inflammatory response is key in atherosclerosis. Endothelial dysfunction is an early sign. It makes the endothelium less functional, leading to more permeability and adhesion molecule expression.
This allows leukocytes to enter and lipids to get into the arterial wall. The inflammatory process then gets worse, with macrophages and T lymphocytes playing a part. Cytokines and chemokines help this inflammation grow, making the plaque unstable.
Stages of Plaque Formation and Development
Plaque formation happens in stages. First, lipid accumulation forms fatty streaks in the arterial wall. These then grow into more complex plaques with a fibrous cap, lipid core, and inflammatory cells.
As plaques get older, they can rupture. This can cause sudden heart problems. The stability of the plaque depends on its fibrous cap thickness, lipid core size, and inflammatory cell presence.
Locations and Types of Atherosclerotic Disease
Atherosclerosis can show up in different parts of the arteries. This leads to various symptoms. It’s a complex condition to handle because of its different forms.
Coronary Artery Disease (CAD)
When atherosclerosis hits the coronary arteries, it causes Coronary Artery Disease (CAD). CAD is a big problem worldwide, leading to heart pain or heart attacks. It happens when the coronary arteries get narrowed or blocked by plaque.
Cerebrovascular Atherosclerosis
Atherosclerosis in the brain’s arteries can cause strokes or TIAs. This happens when the blood flow to the brain stops. It can be due to a blockage or a plaque rupture. It’s a big risk for brain problems.
Peripheral Arterial Disease
Peripheral Arterial Disease (PAD) affects the arteries in the legs. It can cause pain when walking, pain even when resting, and in bad cases, gangrene. PAD often means you’re at risk for a heart problem, too.
Knowing about the different types of atherosclerotic disease is key. Each one needs its own treatment plan. This helps doctors manage the disease better.
Risk Factors for Developing Atherosclerosis
The risk of getting atherosclerosis is affected by modifiable and non-modifiable factors. Knowing these factors is key to preventing and managing the disease.
Modifiable Risk Factors
There are several risk factors that can be changed to lower the risk of atherosclerosis. These include:
- High Cholesterol: Too much low-density lipoprotein (LDL) cholesterol can cause plaque buildup.
- Hypertension: High blood pressure can damage artery walls, making them more prone to atherosclerosis.
- Diabetes: Diabetes mellitus speeds up atherosclerosis by affecting blood vessels and lipid metabolism.
- Smoking: Smoking damages blood vessel linings and promotes plaque buildup.
By tackling these modifiable risk factors through lifestyle changes and medical treatments, people can lower their risk of atherosclerosis.
Non-Modifiable Risk Factors
Some risk factors can’t be changed. These include:
- Family History: A family history of atherosclerosis or heart disease raises an individual’s risk.
- Age: The risk of atherosclerosis grows with age as plaque builds up over time.
- Gender: Men are generally at higher risk than women, but women’s risk increases after menopause.
Understanding these non-modifiable risk factors helps in assessing overall risk and planning preventive strategies.
Clinical Manifestations and Complications
Atherosclerotic disease can cause a range of symptoms, from mild to severe. The health impact depends on which arteries are affected and how much.
Symptoms Based on Affected Arteries
The symptoms of atherosclerosis vary by location. For example, coronary artery disease can cause angina or heart attacks. Peripheral artery disease leads to leg pain during exercise.
Carotid artery disease can result in TIAs or strokes. Symptoms include sudden weakness, trouble speaking, or vision changes.
Major Complications
Atherosclerosis can lead to severe complications. Myocardial infarction (heart attack) is a major risk. It happens when the blood flow is blocked, damaging the heart muscle.
Stroke is another serious complication. It occurs when brain blood flow is interrupted, causing brain tissue damage.
| Artery Affected | Potential Symptoms | Major Complications |
| Coronary Arteries | Angina | Myocardial Infarction |
| Peripheral Arteries | Claudication | Peripheral Artery Disease |
| Carotid Arteries | TIAs, Stroke Symptoms | Stroke |
Diagnostic Approaches for Atherosclerosis
Diagnosing atherosclerosis needs a detailed plan. We use many methods to find out what’s going on. This is key to treating it well.
Non-Invasive Diagnostic Methods
First, we try non-invasive tests. These are safe and easy. They include:
- Ultrasound: Helps check the carotid and peripheral arteries.
- Computed Tomography (CT) scans: Show detailed images of arteries and find calcium.
- Magnetic Resonance Imaging (MRI): Gives clear pictures of the artery walls and inside.
Invasive Diagnostic Procedures
If non-invasive tests don’t work, we might need to do more. These are more detailed and include:
| Procedure | Description | Use |
| Angiography | Uses contrast to see inside the arteries. | Finds blockages and narrow spots in arteries. |
| Intravascular Ultrasound (IVUS) | Uses ultrasound with angiography for detailed views. | Looks at plaque and checks stent placement. |
We pick the right tests for each patient. This way, we can manage atherosclerosis effectively.
Treatment Strategies for Atherosclerosis
Atherosclerosis treatment includes many options. We use a mix of medicines and lifestyle changes. Each plan is made just for the patient.
Pharmaceutical Interventions
Medicines are key in treating atherosclerosis. Statins help lower cholesterol. Antiplatelet agents stop blood clots. Medicines for high blood pressure and diabetes are also used.
Surgical and Interventional Procedures
For serious cases, surgery or interventional procedures are needed. Angioplasty and stenting open narrowed arteries. Sometimes, surgery is needed to bypass blocked areas.
Lifestyle Modifications as Treatment
Changing your lifestyle is important. We suggest a healthy diet and physical exercise. Quitting smoking and keeping a healthy weight are also key.
By using these strategies together, we can manage atherosclerosis well. This helps lower the risk of heart problems.
Emerging Research and Future Directions
New research is uncovering the complex nature of atherosclerosis, bringing hope for better treatments. Studies are key to finding new ways to help patients. We’re seeing big steps forward in treatments and early detection.
Novel Therapeutic Approaches
Scientists are looking into new ways to fight atherosclerosis. They’re focusing on anti-inflammatory drugs and PCSK9 inhibitors. Some exciting areas include:
- Immunotherapy to change how our immune system works
- Gene therapy to tackle genetic causes of atherosclerosis
- Nanoparticle treatments for precise drug delivery
Advancements in Early Detection
Spotting atherosclerosis early is vital. New tools and methods are being developed. These include:
- High-tech imaging like MRI and PET scans
- Biomarkers to find at-risk patients and track disease
- AI and machine learning to predict heart problems
These new research areas are full of hope for better atherosclerosis management. As we keep exploring, we’ll likely see big gains in patient care.
Conclusion: Living with and Managing Atherosclerosis
Managing atherosclerosis well needs a mix of lifestyle changes, medicine, and regular check-ups. Knowing about the condition helps people take care of their health.
Living with atherosclerosis means making smart lifestyle choices. This includes eating right, staying active, and not smoking. It also means following your doctor’s advice and going for regular health checks.
Getting help from many healthcare experts is key. They can help create a treatment plan that fits you. This plan includes lifestyle changes and keeping up with new ways to manage atherosclerosis.
By focusing on a complete and personal approach, people can manage atherosclerosis well. This reduces the chance of serious problems and improves their liality.
FAQ
What is atherosclerosis?
Atherosclerosis is a serious condition where plaque builds up in arteries. This makes them hard and narrow. It reduces blood flow to important organs.
What is the difference between atherosclerosis and arteriosclerosis?
Atherosclerosis is a specific type of arteriosclerosis. It involves atheromatous plaques. Arteriosclerosis is the general hardening of arteries. Atherosclerosis is more specific, with lipids, inflammatory cells, and fibrous elements.
What are the risk factors for developing atherosclerosis?
Risk factors include high blood pressure, high cholesterol, and smoking. Diabetes is also a risk. Non-modifiable factors are age, family history, and genetics.
How is atherosclerosis diagnosed?
It’s diagnosed with non-invasive methods like ultrasound and CT scans. MRI and angiography are also used. The choice depends on the disease’s location and severity.
What are the symptoms of atherosclerosis?
Symptoms vary by artery. Coronary artery disease causes chest pain. Cerebrovascular atherosclerosis can lead to stroke. Peripheral arterial disease causes leg pain when walking.
How is atherosclerosis treated?
Treatment includes managing risk factors with medicine. Surgical and interventional procedures restore blood flow. Lifestyle changes like diet and exercise are also key.
Can atherosclerosis be prevented?
While some risk factors can’t be changed, lifestyle changes and medicine can help. This can prevent or slow the disease.
What is the impact of atherosclerosis on cardiovascular health?
Atherosclerosis is a major cause of heart attacks, strokes, and peripheral arterial disease. Managing it is vital for heart health.
What are the emerging research directions in atherosclerosis?
Research focuses on new treatments targeting inflammation and lipid metabolism. Advances in early detection using biomarkers and imaging are also being explored.
How does atherosclerosis affect different parts of the body?
It affects various arteries, including coronary, cerebral, and peripheral arteries. This leads to different symptoms and complications.
References
- O’Rourke, M. F. (2018). Structure and function of systemic arteries: reflections on the vascular wall and blood flow. Vascular Medicine, 23(4), 316-323. https://pubmed.ncbi.nlm.nih.gov/30016416/