Last Updated on December 2, 2025 by Bilal Hasdemir
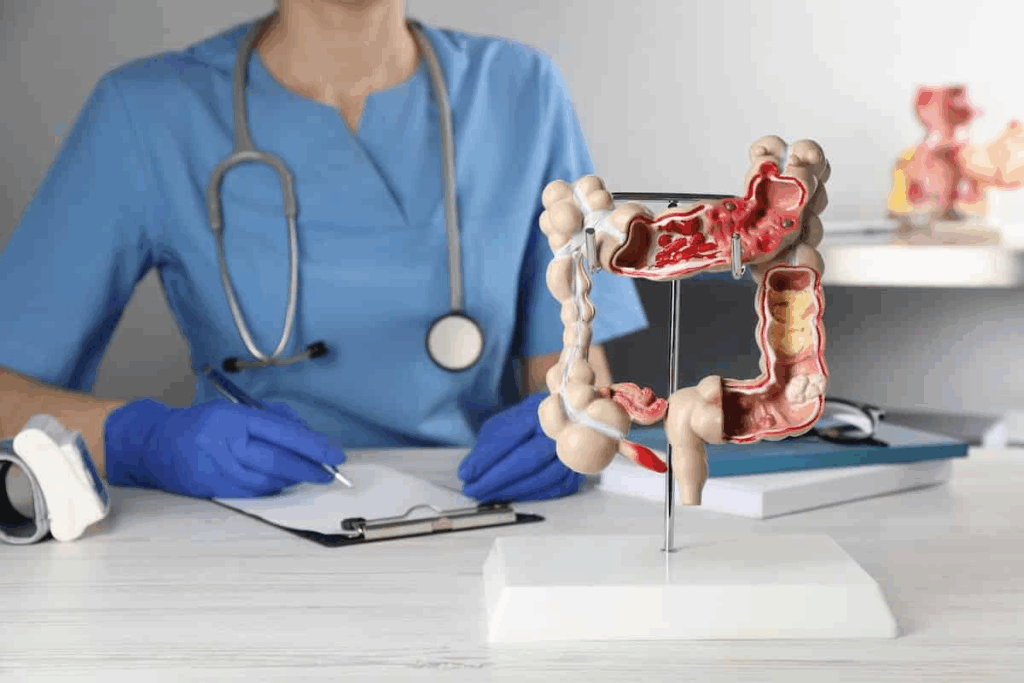
Nearly 150,000 Americans are diagnosed with colorectal cancer each year. Many need surgery to treat it. Knowing what to expect before, during, and after colorectal surgery is key. It helps patients make smart choices about their health.
The colorectal surgery success rate is a big worry for patients. But, thanks to new tech and better surgery methods, results and survival rates have gotten much better.
Key Takeaways
- Colorectal surgery is a big deal that needs careful thought and prep.
- Knowing about the surgery’s results and survival chances helps patients make good choices.
- New medical tech and surgery methods have made care better.
- Patients should talk to their doctors about their specific needs and worries.
- A good recovery plan is key for the best results.
Understanding Colorectal Surgery
It’s important for patients to understand colorectal surgery. This is true when they face conditions needing surgery.
Common Conditions Requiring Colorectal Surgery
Colorectal surgery treats many issues. These include inflammatory bowel disease (IBD), colon cancer, and other disorders.
- Inflammatory Bowel Disease (IBD)
- Colon Cancer
- Diverticulitis
- Colorectal Polyps
These problems can really affect a person’s life. Surgery is often the next step when other treatments don’t work.
When Surgery Becomes Necessary
Surgery is needed when conditions are severe. Or when other treatments have not helped.
Condition | When Surgery is Considered |
Colon Cancer | When diagnosed, specially if advanced |
IBD | When medication fails to control symptoms |
Diverticulitis | Recurrent or severe cases |
Choosing surgery is a big decision. It involves weighing the benefits and risks. And talking it over with a healthcare provider.
Types of Colorectal Surgical Procedures
Colorectal surgery uses different techniques, from open surgery to minimally invasive methods. These methods treat various conditions in the colon and rectum. The right procedure depends on the patient’s diagnosis, health, and other factors.
Open Surgery vs. Minimally Invasive Approaches
There are two main ways to do colorectal surgery: open surgery and minimally invasive methods. Open surgery uses a big cut to directly reach the problem area. On the other hand, minimally invasive surgery uses small cuts and tools like laparoscopes for a less invasive approach. This method causes less damage, less pain, and faster recovery.
Here’s a comparison of open and minimally invasive surgery:
Characteristics | Open Surgery | Minimally Invasive Surgery |
Incision Size | Larger incision | Smaller incisions |
Recovery Time | Generally longer | Typically shorter |
Pain Level | More post-operative pain | Less post-operative pain |
Resection Procedures
Resection procedures remove the sick part of the colon or rectum. They can be done with open or minimally invasive surgery. The success of colorectal resection depends on the condition and the patient’s health.
Ostomy Procedures
Some patients need an ostomy, which creates an opening in the abdomen for waste. This can be temporary or permanent. Ostomy procedures need ongoing care for the best results.
Choosing Your Colorectal Surgeon and Facility
Choosing the right colorectal surgeon and facility is key to a good outcome. It’s important to pick wisely.
Qualifications to Look For
A good colorectal surgeon has the right qualifications. Look for someone who is:
- Board-certified by the American Board of Surgery or the American Osteopathic Board of Surgery
- Fellowship-trained in colorectal surgery
- Experienced in the procedure you need
Certification shows they meet high standards. Fellowship training means they’ve had extra training in colorectal surgery.
Questions to Ask Your Surgeon
It’s important to talk to your surgeon before deciding. Ask them:
- How many times have they done this surgery?
- What risks and complications might there be?
- How they plan to manage your pain?
- How they’ll help you recover?
These questions help you understand their experience and approach to your care.
Hospital Volume and Specialization
The hospital’s volume and specialization matter. High-volume hospitals often have better results. Hospitals focused on GI care have a team ready for your needs.
When looking at hospitals, check their:
- Accreditation status
- Quality metrics, like infection rates and patient satisfaction
- Use of the latest surgical technologies
By looking at these factors, you can choose a facility that improves your surgery’s success.
Pre-Surgical Evaluation and Testing
A thorough pre-surgical check is key to spotting risks and improving surgery results. It includes many tests to see if the patient is ready for surgery.
Medical Assessment
The medical check is very important. It looks at the patient’s health history, current health, and anything that might affect surgery or recovery. This includes past surgeries, medical conditions, and medicines.
Key aspects of the medical assessment include:
- Review of medical history
- Assessment of current health status
- Evaluation of medications and supplements
Imaging and Laboratory Tests
Imaging and lab tests give vital info about the patient’s health. They help plan the surgery. Common tests are:
- Imaging studies (e.g., CT scans, MRI)
- Blood tests to check overall health and find problems
- Other tests as needed based on the patient’s health
Test Type | Purpose | Examples |
Imaging Studies | To see the surgery area and disease extent | CT scans, MRI, X-rays |
Blood Tests | To check overall health and find issues | Complete Blood Count (CBC), Blood Chemistry Tests |
Other Diagnostic Tests | To check specific conditions or risks | Electrocardiogram (ECG), Pulmonary Function Tests |
Bowel Preparation
Bowel prep is vital for colorectal surgery. It lowers infection risk and makes the surgery area clean. It includes diet changes, bowel cleansing, and sometimes antibiotics.
Key elements of bowel preparation include:
- Dietary changes to reduce bowel content
- Bowel cleansing with laxatives or enemas
- Antibiotic use as the surgeon directs
Preparing for Your Colorectal Surgery
To have a successful colorectal surgery, it’s key to prepare both physically and mentally. Good preparation can greatly affect your recovery and experience.
Lifestyle Adjustments Before Surgery
Before surgery, making some lifestyle changes can help. These changes include:
- Dietary Changes: Eating a balanced diet rich in nutrients can help your body prepare for surgery.
- Exercise: Regular physical activity, as advised by your doctor, can improve your physical condition.
- Smoking Cessation: Quitting smoking several weeks before surgery can significantly reduce complications.
- Limiting Alcohol: Reducing or eliminating alcohol consumption can also contribute to a smoother surgery and recovery.
Medication Management
Proper management of your medications before surgery is vital. This includes:
- Reviewing Medications: Inform your surgeon about all medications you’re currently taking.
- Adjusting Medications: Some medications may need to be paused or adjusted before surgery.
- Blood Thinners: Medications that thin your blood may need to be stopped temporarily to reduce the risk of bleeding.
Mental Preparation
Mental preparation is just as important as physical preparation. Strategies include:
- Stress Reduction Techniques: Practices such as meditation or deep breathing can help manage stress.
- Support System: Having a strong support system of family and friends can provide emotional comfort.
- Understanding the Procedure: Educating yourself about what to expect during and after surgery can reduce anxiety.
By focusing on these areas, you can ensure you’re well-prepared for your colorectal surgery. This leads to a more successful outcome and smoother recovery.
The Day of Surgery: What to Expect
Knowing what to expect on the day of your colorectal surgery can help you feel more prepared and in control.
Arrival and Pre-Op Procedures
On the day of your surgery, you will arrive at the hospital a few hours before. You’ll go to the pre-operative area to get ready for surgery.
The pre-operative process includes several steps:
- Completing any remaining paperwork and reviewing your medical history.
- Changing into a surgical gown.
- Receiving an IV line for administering medications and fluids.
- Meeting with your surgical team and anesthesiologist to review the plan.
Anesthesia Process
Anesthesia is key to your comfort during surgery. Your anesthesiologist will explain the type of anesthesia and the process.
The anesthesia process involves:
- Administering anesthesia through your IV line.
- Monitoring your vital signs closely throughout the procedure.
- Adjusting the anesthesia as needed to maintain your comfort.
Duration and Surgical Team
The surgery’s length depends on the procedure’s complexity and your condition.
Your surgical team includes:
Team Member | Role |
Surgeon | Performs the surgery. |
Anesthesiologist | Administers and monitors anesthesia. |
Nurses and Surgical Technologists | Assist the surgeon and care for you during the procedure. |
Knowing your surgical team’s roles can make you feel more at ease on surgery day.
Colorectal Surgery Success Rate: Understanding the Statistics
Colorectal surgery has seen a big improvement in success rates over time. Success in colorectal surgery depends on many factors and metrics. These help determine how well a patient does after surgery.
Overall Success Metrics
Success in colorectal surgery is measured in several ways. These include how many procedures are successful, complication rates, and survival rates for cancer patients. Most patients see a big improvement in their quality of life after surgery.
Success rates can change based on the surgery type and the patient. For example, surgeries for non-cancerous conditions usually have better success rates than those for cancer.
Factors Influencing Success Rates
Many things can affect how well colorectal surgery works. These include:
- The skill and experience of the surgical team
- The patient’s overall health
- The cancer stage at diagnosis (for cancer patients)
- The type of surgery done
Knowing these factors is important for both patients and doctors when deciding on surgery.
Stage-Based Survival Rates for Cancer Patients
For cancer patients, survival rates by cancer stage are very important. These rates help show how well colorectal surgery works. Survival rates are based on the cancer stage at diagnosis.
Cancer Stage | 5-Year Survival Rate |
Stage I | 90% |
Stage II | 70-80% |
Stage III | 40-60% |
Early-stage cancer patients have much higher survival rates after surgery. Early detection and treatment are very important for better survival chances.
Immediate Post-Operative Recovery
The time right after colorectal surgery is very important. Knowing what to expect can make recovery easier. This includes the hospital stay, managing pain, and getting back to moving and eating.
Hospital Stay Duration
The time you spend in the hospital can change based on your surgery and health. People who have less invasive surgeries might stay less than those with open surgery.
Surgery Type | Average Hospital Stay |
Minimally Invasive Surgery | 2-4 days |
Open Surgery | 5-7 days |
Pain Management
Managing pain right after surgery is key. Doctors give pain meds to help with discomfort. They adjust the type and amount based on how you’re doing.
Pain management strategies may include:
- Opioid analgesics for severe pain
- Non-opioid medications for mild to moderate pain
- Regional anesthesia techniques
Initial Mobility and Nutrition
Moving around early is important to avoid problems like blood clots. It also helps your body heal. You’ll also learn about eating the right foods for recovery.
- Hydration with clear fluids initially
- Gradual introduction to solid foods
- Avoiding heavy or spicy foods
Potential Complications and Risk Factors
It’s important for patients to know about the risks of colorectal surgery. This surgery is often a lifesaver, but it’s good to understand the possible complications.
Common Short-Term Complications
Short-term complications happen during or right after surgery. Some common ones include:
- Infection: Any surgery, like colorectal procedures, can lead to infections at the surgical site.
- Bleeding: Too much bleeding during or after surgery is a possible issue.
- Adverse reactions to anesthesia: Some people may have bad reactions to the anesthesia used during surgery.
Long-Term Complications
Long-term complications can show up weeks, months, or even years later. These might include:
- Stoma complications: Patients with ostomy procedures might face issues with their stoma.
- Adhesions: Scar tissue in the abdomen can cause bowel obstruction.
- Changes in bowel habits: Some people might experience diarrhea or constipation after surgery.
Risk Reduction Strategies
While some risks are part of colorectal surgery, there are ways to lower them. These include:
- Preoperative optimization: Being as healthy as possible before surgery can help.
- Following post-operative instructions: It’s key to follow the surgeon’s advice after surgery for a smooth recovery.
- Maintaining a healthy lifestyle: Eating well, exercising regularly, and not smoking can lead to better results.
Long-Term Recovery and Follow-Up Care
After colorectal surgery, the road to full recovery is long. It requires careful follow-up care and a focus on long-term health. This stage is key to making sure the surgery works well and to catch any problems early.
Follow-Up Appointment Schedule
Regular visits with your surgeon or healthcare provider are vital. These meetings help your doctor check on your healing, solve any issues, and tweak your treatment plan if needed. Usually, the first check-up is a few weeks after surgery, with more visits spaced out over months.
Surveillance Testing
Surveillance testing is a big part of follow-up care, mainly for those who had surgery for colorectal cancer. This might include colonoscopies, CT scans, and blood tests to watch for tumor markers. How often and what kind of tests you need depends on your risk factors and surgery details.
When to Contact Your Doctor
Knowing when to reach out to your doctor is important during recovery. Call your doctor if you have severe belly pain, fever, vomiting, or signs of infection at the surgery site. Also, talk to your healthcare provider about any recovery worries or questions you have.
Following your follow-up schedule and staying alert to your health can help you recover well after colorectal surgery.
Quality of Life After Colorectal Surgery
The journey after colorectal surgery touches on many areas. These include physical recovery, changes in diet, and mental health. Knowing about these can greatly affect a person’s quality of life.
Physical Function and Limitations
After surgery, patients might notice changes in how they feel physically. Some common issues include:
- Reduced stamina and fatigue
- Temporary or permanent changes in bowel habits
- Potential for ostomy or changes in urinary function
Talking to a healthcare provider about these changes is key. It helps manage expectations and find ways to lessen their impact.
Dietary Considerations
Diet is very important for recovery and long-term health after surgery. Patients are often told to:
- Follow a specific post-operative diet to manage bowel movements and minimize discomfort
- Stay hydrated to prevent constipation and maintain overall health
- Gradually reintroduce foods to identify any that may cause intolerance or discomfort
Eating a balanced diet helps regain strength and aids in healing.
Psychological and Social Adjustment
The emotional side of colorectal surgery is significant. Patients may feel a mix of emotions, from anxiety and depression to relief and gratitude. Support from loved ones and healthcare teams is essential in dealing with these feelings.
Strategies for emotional and social adjustment include:
- Seeking support groups for shared experiences and advice
- Engaging in counseling or therapy to address emotional challenges
- Gradually resuming social activities to rebuild connections and confidence
By understanding and tackling these areas, patients can improve their recovery journey and enhance their quality of life after surgery.
Advancements in Colorectal Surgical Techniques
The field of colorectal surgery has seen big changes in recent years. These changes have made surgeries more precise and safer. They have also made care for patients better.
Robotic-Assisted Surgery
Robotic-assisted surgery is a big step forward. It gives surgeons better control and vision. This makes surgeries more precise and safer.
Robotic surgery has many benefits:
- It makes surgeries more precise
- It reduces blood loss and complications
- It uses smaller cuts, leaving less scarring
- Patients recover faster
Enhanced Recovery After Surgery (ERAS) Protocols
Enhanced Recovery After Surgery (ERAS) protocols are another big step. They help make care better and faster. ERAS includes things like better nutrition and pain control.
ERAS has key parts:
- It includes pre-surgery education
- It focuses on nutrition and fluids
- It uses standard pain control
- It encourages early movement
Future Innovations
The future of colorectal surgery looks bright. New technologies like artificial intelligence and machine learning will help a lot. They will improve planning and care after surgery.
New materials and ways to fix tissues are also coming. These will help with complex problems. Patients will see better results and faster recovery times.
Conclusion
Understanding colorectal surgery is key for patients going through it. The success rate depends on several things. These include the surgery type, the condition, and the patient’s health.
Thanks to new techniques, like robotic surgery and ERAS protocols, results have gotten better. These advancements help patients recover faster and face fewer complications. This leads to better outcomes for patients.
By learning from this article, patients can make better choices. They can understand what to expect from their surgery. This knowledge helps them recover better and improves their life after surgery.
FAQ
What is the overall success rate of colorectal surgery?
The success rate of colorectal surgery depends on several factors. These include the condition being treated, the cancer stage, and the patient’s health. Studies show a 5-year survival rate of up to 90% for early-stage colorectal cancer.
What are the most common conditions that require colorectal surgery?
Common reasons for colorectal surgery include colorectal cancer, diverticulitis, and inflammatory bowel disease. It’s also needed for certain benign polyps and to repair rectal prolapse.
How do I choose the right colorectal surgeon?
Look for a surgeon who is board-certified and experienced in colorectal surgery. Check their hospital privileges and ask about their approach to your condition. It’s also important to know their complication rates.
What can I expect during the pre-surgical evaluation and testing process?
You’ll have a detailed medical check-up before surgery. This includes imaging and lab tests to assess your health and condition. You might also need to prepare your colon.
How can I prepare for colorectal surgery?
Follow your surgeon’s advice on lifestyle changes and medication management. Quit smoking and follow a specific diet as recommended.
What happens on the day of surgery?
On surgery day, you’ll arrive at the hospital for pre-op procedures. You’ll receive anesthesia and be treated by a skilled team. The surgery’s length depends on its complexity.
What are the possible complications of colorectal surgery?
Risks include short-term issues like infection and bleeding, and long-term problems like ostomy complications. Your surgeon will discuss these risks and how to minimize them.
How long does it take to recover from colorectal surgery?
Recovery time varies based on the surgery type, your health, and any complications. You’ll likely spend several days in the hospital and weeks to months at home recovering.
What is the quality of life like after colorectal surgery?
Recovery can bring changes in physical function and dietary needs. You may also face psychological and social adjustments. With proper care, many patients return to normal activities and enjoy a good life quality.
Are there any advancements in colorectal surgical techniques that I should know about?
Yes, there are advancements like robotic-assisted surgery and Enhanced Recovery After Surgery (ERAS) protocols. These aim to improve outcomes, reduce complications, and enhance recovery.
How successful is colorectal surgery in treating cancer?
Surgery’s success in treating cancer depends on the cancer stage. For early-stage cancer, surgery can be very effective, with high cure rates. For advanced cancer, surgery is often combined with other treatments like chemotherapy and radiation.
What is the mortality rate associated with colorectal surgery?
The mortality rate varies based on your health, the surgery complexity, and the surgeon’s experience. It’s generally low, ranging from 1-5% in most studies.
How often are follow-up appointments needed after colorectal surgery?
You’ll need regular follow-up appointments to monitor your recovery and check for complications. The appointment frequency depends on your condition and the surgeon’s advice.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/30595870/