Learn about the health risks associated with IVF for the mother (OHSS symptoms) and child (prematurity), and how to manage them.
Send us all your questions or requests, and our expert team will assist you.
Infertility is often a silent struggle. Couples may feel isolated, frustrated, or even guilty, wondering “Why us?” at every negative pregnancy test. At Liv Hospital, we want to shift the narrative. Infertility is not a failure of character; it is a medical condition of the reproductive system. And like any medical condition, it has specific causes that can be identified and treated.
The first step to a successful pregnancy is a precise diagnosis. In about 40% of cases, the cause lies with the female partner; in 40%, it lies with the male partner; and in 20% of cases, it is a combination of both or remains “unexplained.” Our IVF Causes and Evaluation program is designed to investigate both partners simultaneously, ensuring that no time is wasted treating the wrong problem.
The medical definition of infertility is based on time, not just biology. You should schedule a consultation with our fertility specialists if:
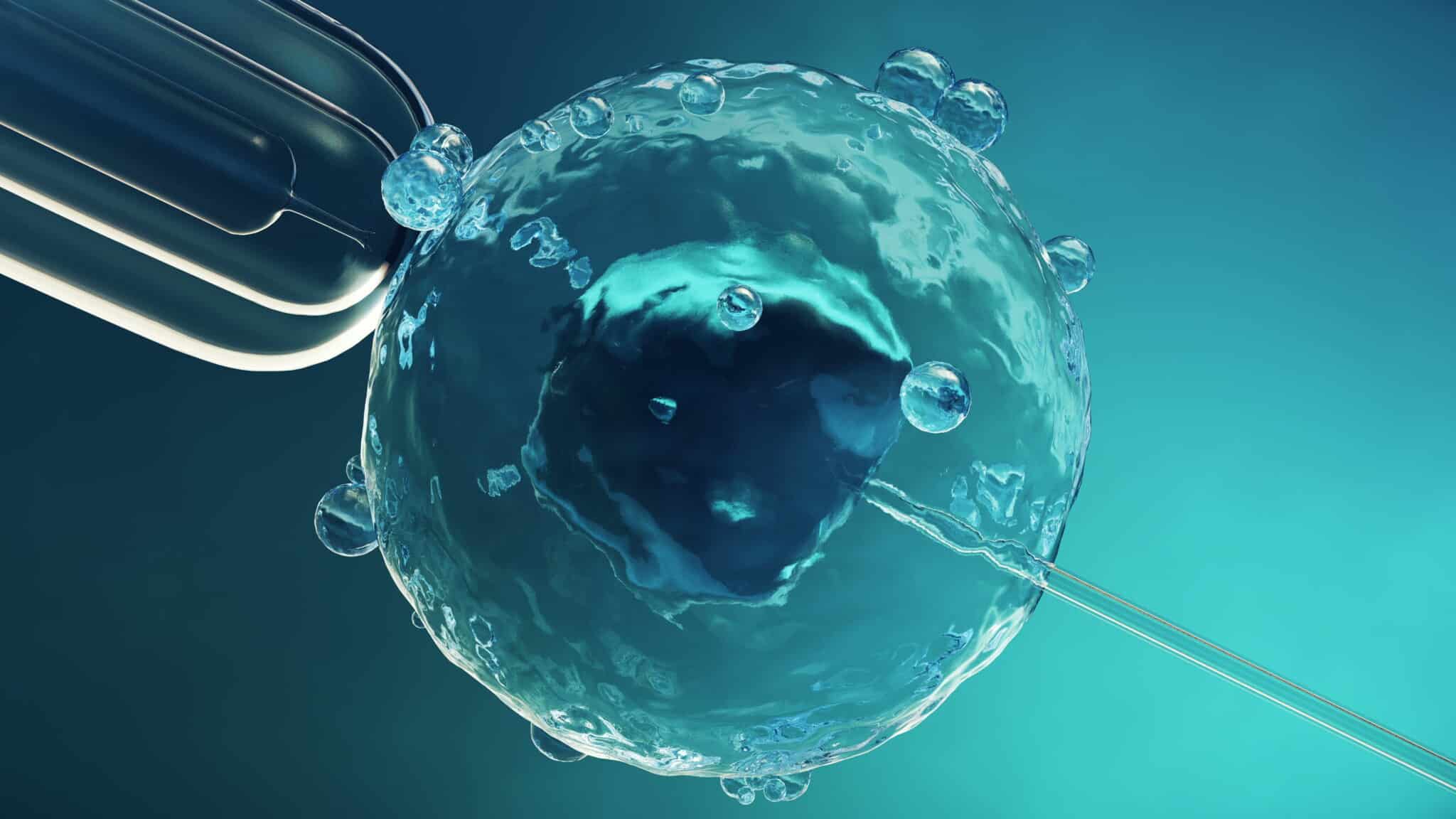
For a woman to conceive, a complex sequence of events must occur perfectly: hormones must trigger an egg to mature, the ovary must release it (ovulation), the fallopian tube must catch it, sperm must fertilize it, and the resulting embryo must implant in the uterus. A disruption at any stage causes infertility.

If you don’t ovulate, there is no egg to fertilize.

The fallopian tubes are the “meeting place” for sperm and egg.
The “soil” must be healthy for the “seed” to grow.
A painful condition where tissue similar to the uterine lining grows outside the uterus (on ovaries, tubes, or bowel).

Send us all your questions or requests, and our expert team will assist you.

Historically, infertility was seen as a “woman’s problem.” We now know that Male Factor Infertility is the sole cause in 20-30% of cases and a contributing factor in another 20-30%.
Sometimes the sperm count looks normal, but the DNA inside the sperm head is damaged (fragmented). High fragmentation is a major cause of Recurrent Miscarriage and “Unexplained Infertility.”

In about 15-20% of couples, all standard tests come back normal. The sperm is good, tubes are open, and ovulation is regular. This is called Unexplained Infertility.
In about 15-20% of couples, all standard tests come back normal. The sperm is good, tubes are open, and ovulation is regular. This is called Unexplained Infertility.
When you arrive at Liv Hospital for your initial evaluation, we perform a “360-degree” assessment. We recommend both partners attend the first visit.
If a couple has had recurrent miscarriages or failed IVF cycles, we perform a Karyotype blood test on both parents.
To make the most of your consultation at Liv Hospital, please bring:

Most women experience moderate cramping, similar to menstrual cramps, when the dye is injected. This lasts for only a few minutes. We recommend taking a mild painkiller (like Ibuprofen) 1 hour before the procedure.
Sometimes. If the cause is a hormonal imbalance, medication (like Clomid) can boost sperm count. If it is a varicocele, surgery might help. However, for severe counts, IVF with ICSI is the fastest and most effective route to pregnancy.
Stress doesn’t block tubes or kill sperm directly, but extreme stress can disrupt the brain signals (GnRH) that trigger ovulation or sperm production. It can also lower libido. We treat stress as a contributing factor, not a primary cause.
This refers to the 3rd day of your menstrual period (Day 1 is the first day of full flow). This is the baseline when your hormones are “quiet,” giving us the most accurate reading of your ovarian function (FSH/E2).
You can do the ultrasound and AMH test while on the pill, but you cannot do the Day 3 hormone panel (FSH/LH) because the pill suppresses these hormones. You will need to stop the pill for one cycle to get accurate baseline blood work.


Guide to the ideal location where in the uterus does the embryo implant (upper posterior wall). Knowing embryo implantation location is key for a healthy
Explaining the best location where do embryos implant in the uterus for successful pregnancy. Embryo implantation is a key step in human reproduction, starting a
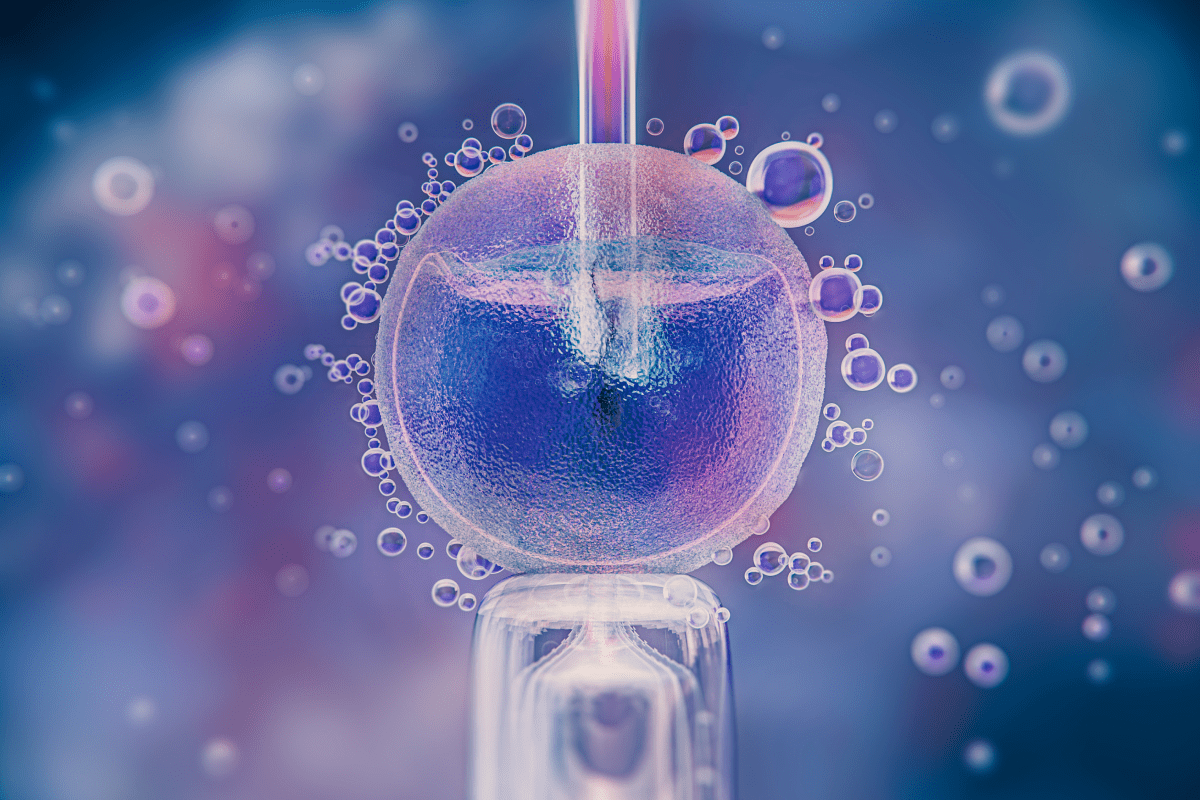
The bloating after embryo transfer is filled with hope and worry. People watch their bodies for signs of a successful embryo implantation. Knowing what to

FET ultrasound is key in modern fertility treatments. It helps place embryos exactly in the uterus. This makes IVF treatments more successful for many people.
The Depo-Provera shot is a popular birth control option for many women. But, it’s important to know what happens when you stop using it. This
The Depo-Provera injection, also known as the Depo shot, is a top-notch birth control option. It has a success rate of over 99% in preventing

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)