Get clarity on your fertility journey with thorough in vitro fertilization diagnosis and tests. learn about the simple and advanced testing needed before starting IVF.
Send us all your questions or requests, and our expert team will assist you.
In Vitro Fertilization (IVF) is a journey of hope, science, and patience. For many couples, the prospect of starting treatment feels overwhelming—a blur of injections, appointments, and medical jargon. At Liv Hospital, we believe that knowledge is the antidote to anxiety. When you understand exactly what is happening inside your body at each stage, you regain a sense of control over your fertility journey.
The IVF process is a carefully choreographed series of events designed to maximize your chances of success. While every patient’s protocol is unique (tailored to your age, hormone levels, and medical history), the fundamental IVF procedure steps remain the same. Here is your comprehensive, day-by-day guide to creating life at our center.

In a natural menstrual cycle, your body selects only one egg to mature and release. The goal of IVF is to recruit a “cohort” of eggs so that we have multiple chances to create a healthy embryo.
This is the day of the “harvest.” It is a minor surgical procedure performed in our sterile IVF operating room.
While you rest at your hotel, the most critical work begins in the laboratory.

The next morning (Day 1 post-retrieval), we check for fertilization. Seeing two “pronuclei” (one from mom, one from dad) confirms a successful embryo. Now, the waiting game begins.
For patients over 35, those with recurrent miscarriages, or those seeking gender-linked disease screening, we pause here for genetics.

Send us all your questions or requests, and our expert team will assist you.
Whether it is a “Fresh Transfer” (Day 5) or a “Frozen Transfer” (weeks later), this is the emotional climax of the cycle.
For the next 12 days, you must support the uterine lining to help the embryo stick.
12 days after the transfer, you will have a blood test to measure Beta-hCG (the pregnancy hormone).
Empty follicle syndrome is rare, but sometimes follicles are empty, or eggs do not detach. If this happens, the doctor will review the trigger shot timing and medication protocol to adjust for a future attempt.
Modern practice emphasizes Single Embryo Transfer (SET) to avoid the high risks associated with twin or triplet pregnancies. The goal is one healthy baby at a time.
Most women compare the feeling to a Pap smear. It involves a speculum and a thin catheter passing through the cervix. It is generally not painful, though a full bladder is required, which can be uncomfortable.
Day 5 embryos (blastocysts) are more developed and have passed a natural selection point, offering higher success rates. Day 3 embryos are smaller and more challenging to select, but may be transferred if few embryos are available.
Embryos frozen via vitrification can be stored indefinitely. There have been successful live births from embryos frozen for over 20 years, as biological time stops at -196 degrees Celsius.


Guide to the ideal location where in the uterus does the embryo implant (upper posterior wall). Knowing embryo implantation location is key for a healthy
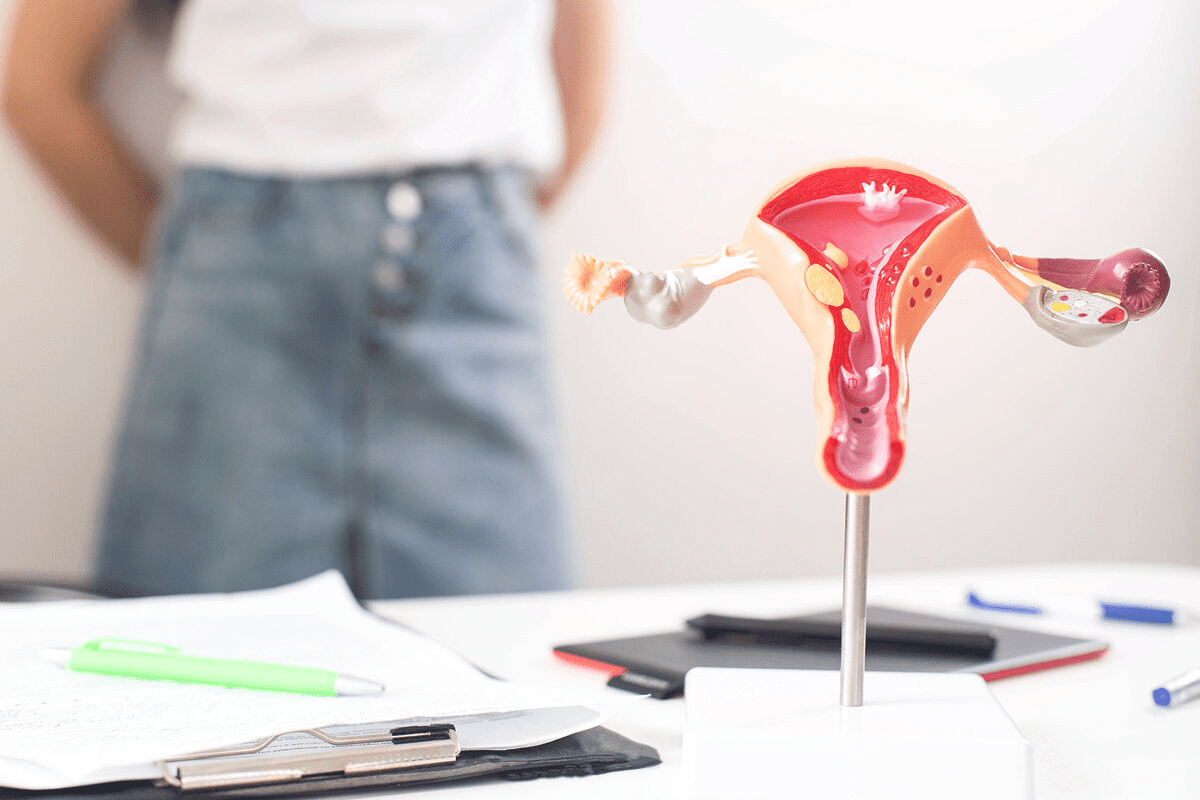
Explaining the best location where do embryos implant in the uterus for successful pregnancy. Embryo implantation is a key step in human reproduction, starting a
The bloating after embryo transfer is filled with hope and worry. People watch their bodies for signs of a successful embryo implantation. Knowing what to

FET ultrasound is key in modern fertility treatments. It helps place embryos exactly in the uterus. This makes IVF treatments more successful for many people.
The Depo-Provera shot is a popular birth control option for many women. But, it’s important to know what happens when you stop using it. This
The Depo-Provera injection, also known as the Depo shot, is a top-notch birth control option. It has a success rate of over 99% in preventing

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)