Last Updated on December 2, 2025 by Bilal Hasdemir

Identifying a lowest success rate surgery based on common metrics and understanding the contributing factors. Research lowest success rate surgery. Did you know some surgeries have a higher risk of problems or failure? High-risk surgeries can have a significant impact on patients’ lives. It’s important to know what makes them risky.
Looking at surgical outcome statistics helps both patients and doctors make better choices. Some surgeries are riskier because they’re complex or the patient’s health is fragile. This increases the chance of poor outcomes.
Key Takeaways
- Certain surgeries have higher risks of complications or failure.
- Understanding surgical outcome statistics is key for making smart choices.
- High-risk procedures need careful thought and planning.
- The patient’s health and the surgery’s complexity affect results.
- Making informed decisions can improve surgical success.
Understanding Surgical Success and Failure
Surgical success rates are important for judging how well surgeries work. It’s key to know what makes a surgery successful and how to measure it. This helps us see the risks and benefits of different surgeries.
Defining Success in Surgical Outcomes
Success in surgery means more than just the surgery going well. It also includes how well the patient recovers and their quality of life after surgery. Surgical success is about:
- Completing the surgery well
- No major problems during or after surgery
- The condition that needed surgery getting better or gone
- The patient being happy and living well after surgery
- Living a long time and not having the problem come back
How Surgical Success Rates Are Measured
Success rates are tracked through different ways, like how many patients die, get complications, and how they do long-term. These numbers show how safe and effective a surgery is. Researchers often use the National Surgical Quality Improvement Program (NSQIP) to get this data.
Factors That Influence Success Statistics
Many things can change how successful a surgery is, including:
- Patient-related factors: Things like age, health problems, and overall health can really affect how well a surgery goes.
- Surgical technique and expertise: The surgeon’s skill and the surgery method used can also change success rates.
- Post-operative care: How well the patient is cared for after surgery can also impact recovery and how many problems they have.
Knowing these factors helps us understand success rates better. It helps us make smarter choices about surgery.
Methodology Behind Surgical Outcome Statistics
It’s key to understand how surgical outcome stats are made. These stats help us see how well and safely surgeries work. They are a big part of checking if surgeries are good and safe.
Data Collection and Analysis Methods
Getting data on surgery results means recording patient info before, during, and after. This includes things like who the patient is, their health before surgery, how the surgery was done, and how they were cared for after.
Then, this data is analyzed using stats that look at many factors. This helps find trends, risks, and ways to get better at surgery.
Limitations in Surgical Success Reporting
Even with better data collection and analysis, there are big challenges in reporting surgery success. One big issue is that what counts as success can vary a lot.
Also, data quality can be affected by things like missing records, not keeping up with follow-ups, and different reporting standards. These issues can make it hard to really know how well surgeries are doing.
Interpreting Surgical Risk Data
Understanding surgical risk data needs a deep look at the stats used and where the data came from. It’s important to think about the patients, the surgical team’s skills, and the surgery methods.
By carefully looking at surgical risk data, doctors can help patients understand what might happen in their surgery. This helps patients make better choices about their care.
Pancreatic Surgeries: The Whipple Procedure
Pancreatic surgeries, like the Whipple procedure, are very hard. The Whipple procedure removes parts of the pancreas, duodenum, gallbladder, and sometimes stomach. It’s mainly for cancer in the pancreas.
Complexity and Technical Challenges
The Whipple procedure is very hard because of its complex anatomy. Surgeons have to be very careful with blood vessels and organs. It’s a big challenge, even for skilled surgeons.
The technical challenges include:
- Delicate dissection around major blood vessels
- Precise reconstruction of the digestive tract
- Management of possible complications like leakage or infection
Mortality and Morbidity Statistics
The Whipple procedure used to have high death and complication rates. But, better surgery and care have made things better.
Now, the death rate is under 5% in big hospitals. But, complications like infections and fistulas are common, affecting 30% to 50% of patients.
Long-term Survival Outcomes
Survival after a Whipple procedure depends on the cancer type. For pancreatic cancer, survival is usually low, around 20% to 30% for those who get the surgery.
But, for other cancers like ampullary or duodenal, survival chances are better. This is true if the cancer is caught early.
In summary, the Whipple procedure is complex but getting better thanks to new techniques and care. Knowing the risks helps doctors and patients make better choices.
Esophageal Resection and Reconstruction
Esophageal resection is a big surgery that removes part of the esophagus. It’s often done for esophageal cancer or severe damage. After, the patient needs reconstruction to swallow again.
Procedural Complications
Esophageal resection and reconstruction come with big risks. These can include:
- Anastomotic leaks: Leaks where the esophagus meets the stomach or intestine.
- Respiratory complications: Issues like pneumonia because of the esophagus’s close location to the lungs.
- Bleeding and hematoma: Too much bleeding or a blood clot forming.
Post-Operative Challenges
Patients face many challenges after surgery. These include:
- Hard time swallowing because of the changed anatomy.
- Problems with nutrition, as eating can be tough.
- Reflux symptoms, as the body’s natural barriers against reflux may be broken.
Managing these issues well is key to a good recovery.
Success Rate Variations by Technique
The success of the surgery depends a lot on the technique used. Minimally invasive methods might lead to quicker recovery and fewer problems than open surgery. The choice of method depends on the patient’s health, cancer stage, and the surgeon’s skills.
Research shows that specialized centers with lots of esophageal surgeries have better results. The skill of the surgical team and post-operative care are also very important for success.
High-Risk Cardiovascular Procedures
Cardiovascular surgeries are often lifesaving but carry big risks. Some procedures are more risky than others. They can lead to serious complications.
Aortic Aneurysm Repair Outcomes
Aortic aneurysm repair is a complex surgery with serious risks. It involves replacing a weak part of the aorta with a graft. Despite progress, there’s a risk of failure, with aortic aneurysm repair fail rates varying.
Research shows EVAR has a lower short-term death rate than open surgery. But, long-term issues like endoleaks and graft migration can complicate outcomes.
Complex Cardiac Revascularization
Complex cardiac revascularization is risky for those with severe heart disease. It aims to improve blood flow by bypassing blocked arteries. Risks include cardiac surgery complications like graft failure or heart attack during surgery.
The success of this surgery depends on the patient’s health and the surgeon’s skill. While techniques and care have improved, challenges persist.
Vascular Bypass Surgery Challenges
Vascular bypass surgery is also high-risk, used to bypass blocked or narrowed blood vessels. Success can be affected by graft patency and comorbid conditions, leading to vascular bypass unsuccess.
Choosing the right graft material and managing post-op care are key challenges. Yet, it’s a vital option for severe vascular disease patients.
Neurosurgical Procedures with Challenging Outcomes
Neurosurgical procedures, like brain tumor removal and spinal surgeries, are very risky. They need a lot of skill and knowledge of the brain and spine.
Brain Tumor Removal Success Rates
Removing brain tumors is a very delicate task. The success rate depends on the tumor’s size, location, and type. Experienced surgeons and advanced imaging help a lot.
A study in the Journal of Neurosurgery found better survival rates for brain tumor surgery. This is thanks to new surgical methods and better care after surgery.
“The success of brain tumor surgery is multifactorial, involving not just the surgical technique but also the patient’s overall health and the tumor’s characteristics.”
Tumor Type | 5-Year Survival Rate | Recurrence Rate |
Glioblastoma | 5-10% | 80-90% |
Meningioma | 80-90% | 10-20% |
Craniotomy Complications and Outcomes
A craniotomy is a procedure where part of the skull is removed to access the brain. It’s a common neurosurgery method but comes with risks like infection and brain damage.
The success of a craniotomy depends on the patient’s health and the skill of the surgical team.
Common Complications of Craniotomy:
- Infection
- Cerebral edema
- Seizures
- Hemorrhage
High-Risk Spinal Surgeries
Spinal surgeries, like those in the cervical or thoracic spine, are very risky. They can cause nerve damage, paralysis, and infection.
The success of spinal surgery relies on accurate diagnosis, the right surgical technique, and good care after surgery. New technologies like navigation systems and intraoperative monitoring have helped improve results.
- Pre-operative planning is key for success.
- Intraoperative monitoring helps prevent nerve damage.
- Post-operative care is vital for recovery.
Organ Transplantation Success Challenges
Organ transplantation is a lifesaving procedure but comes with risks and complications. This makes its success rates vary a lot.
The complexity of organ transplantation shows in its varied success rates. Liver transplantation, for example, is a critical procedure for those with end-stage liver disease.
Liver Transplant Rejection Rates
Liver transplant rejection is a big concern. It can happen in up to 30% of patients in the first year.
Chronic rejection can cause graft loss, needing another transplant. Better immunosuppressive therapy has helped improve graft survival rates.
Multi-Organ Transplant Outcomes
Multi-organ transplants, like liver and kidney transplants at the same time, face unique challenges. The procedure’s complexity and the patient’s health status add to the difficulty.
Research shows that survival rates for multi-organ transplant patients are generally lower than for single-organ transplants.
Long-term Survival Statistics
Long-term survival after organ transplantation has gotten better. This is thanks to better surgical techniques, immunosuppression management, and post-transplant care.
For liver transplant patients, the 5-year survival rate is about 70-80%. But this rate can change based on the disease and the patient’s health.
It’s important to understand these challenges and outcomes. This helps manage patient expectations and work towards better transplant success rates.
Lowest Success Rate Surgery: A Comparative Analysis
The world of surgery has many procedures, each with its own success rate. Some surgeries fail more often than others. It’s important for doctors and patients to know this when deciding on surgery.
Ranking Procedures by Mortality Risk
Surgeries can be ranked by how risky they are. Some surgeries are very dangerous and can be life-threatening. Here are a few examples:
- Pancreatic surgeries, like the Whipple procedure, can have a death rate of 2-8% in top hospitals.
- Esophageal resections are very risky, leading to serious problems, mainly in older people or those with health issues.
- High-risk heart surgeries, like complex heart bypasses and aortic repairs, can have death rates of 5-10% or more.
Comparing Failure Rates Across Specialties
Failure rates also differ between specialties. For example:
- Neurosurgery, like brain tumor removals, is very challenging and often has high failure rates.
- Organ transplants, like liver transplants, struggle with rejection and long-term survival.
- Cancer surgeries, where cancer has spread, usually have worse results than surgeries for localized cancers.
Looking at these failure rates across specialties helps us understand the risks and outcomes of surgery better.
Risk-Benefit Assessment of High-Risk Surgeries
For risky surgeries, it’s key to weigh the benefits against the risks. This means:
- Looking at what the surgery might improve, like survival or quality of life.
- Checking the risks, like death, serious illness, and long-term problems.
- Thinking about the patient’s own health, age, and other conditions.
By carefully considering these points, doctors and patients can make better choices about risky surgeries.
Emergency and Trauma Surgeries
In emergency and trauma surgery, the difference between success and failure is small. These surgeries are urgent, complex, and need quick action. This makes it hard to predict and manage their outcomes.
Success Challenges in Time-Critical Procedures
Emergency and trauma surgeries are tough because they happen fast. The main challenge is the short time for planning and preparing the patient. Damage control surgery is key in trauma care. It aims to keep the patient stable, not fix everything right away.
- Quick decisions are essential.
- Dealing with many injuries makes planning hard.
- Every minute counts to stop things from getting worse.
Damage Control Surgery Outcomes
Damage control surgery is a method for treating severely injured patients. It aims to stop bleeding and prevent infection. The plan is to do more detailed repairs when the patient is stable.
- The first surgery focuses on damage control.
- Then, patients are cared for in the ICU to stabilize.
- More detailed surgery is planned when the patient is better.
This method has helped improve care for critically injured patients. It reduces the initial surgery load. This allows for better recovery and stabilization.
Trauma-Related Mortality Factors
How likely a trauma patient is to die depends on several things. These include how bad the injury is, the patient’s age and health, and the quality of care they get.
Key factors include:
- The severity and cause of the injury.
- The patient’s overall health and any existing conditions.
- How fast and well the patient is treated before and after arrival.
Knowing these factors helps in finding ways to improve trauma patient outcomes.
Cancer-Related Surgical Procedures
Cancer treatment often includes surgery, which can be tough due to the disease’s severity. These surgeries are complex and need careful planning and execution.
The results of these surgeries vary a lot. This depends on the cancer’s stage, the patient’s health, and the surgical team’s skill. It’s important for doctors and patients to understand the challenges and possible complications.
Metastatic Cancer Resection Outcomes
Metastatic cancer resection is a tough procedure with mixed results. Success depends on the metastases’ location and number, and the patient’s health.
Research shows that in some cases, removing metastatic cancer can help patients live longer and feel better. But, there’s a big risk of complications, so choosing the right patients is key.
Lung Cancer Lobectomy Success Rates
Lung cancer lobectomy is a big surgery that removes a lung lobe with cancer. Success depends on the cancer’s stage and the patient’s lung health.
Patients with early-stage lung cancer who have lobectomy tend to do better than those diagnosed later. New surgical methods and care after surgery have made things better for these patients.
Advanced-Stage Cancer Surgical Challenges
Surgery for advanced cancer is very challenging. There’s a higher risk of complications and lower success rates than in early-stage surgeries.
Deciding to have surgery for advanced cancer is based on many factors. These include the chance to improve quality of life or extend life. Palliative care is also a big part of the treatment plan.
Patient-Specific Factors Affecting Surgical Success
Each patient’s unique factors greatly influence surgery success. It’s key for doctors to know these to assess risks and make smart choices.
Age-Related Surgical Risks
Age is a big factor in surgery results. Older people face more risks because their bodies can’t handle surgery as well. They also have more health problems and take longer to get better.
A study in the Journal of the American College of Surgeons showed older patients face more complications and longer hospital stays. This is compared to younger patients having the same surgery.
Table: Age-Related Surgical Risks and Complications
Age Group | Complication Rate (%) | Average Hospital Stay (Days) |
< 65 | 15 | 5 |
65-75 | 25 | 7 |
> 75 | 35 | 10 |
Impact of Comorbidities on Outcomes
Health problems like diabetes, high blood pressure, and heart disease affect surgery results. People with many health issues are at higher risk of problems and death.
Checking and managing health issues before surgery is very important. This helps lower risks. For example, controlling blood sugar in diabetics and managing blood pressure to avoid heart problems.
Nutritional and Functional Status Considerations
A patient’s nutrition and ability to function are key to surgery success. Poor nutrition and low function increase the chance of complications, infections, and longer recovery times.
Improving nutrition before surgery, like adding proteins and essential nutrients, can help outcomes. Also, improving function through prehabilitation programs can lower post-surgery problems.
By understanding and addressing these unique factors, healthcare providers can tailor care to each patient. This can lead to better surgery results.
Hospital and Surgeon Factors in Surgical Outcomes
Hospitals and surgeons play big roles in how well surgeries go. Knowing this helps patients, doctors, and policy makers make surgeries better.
Volume-Outcome Relationship
Research shows that doing more surgeries leads to better results. This is true for many types of operations.
Evidence from Research
- A study in the Journal of the American College of Surgeons found that more surgeries at a hospital means fewer deaths for complex operations.
- Cardiothoracic surgery shows that doing more surgeries makes outcomes better for patients.
Procedure Type | Low Volume Hospitals | High Volume Hospitals |
Complex Cancer Surgeries | Higher mortality rates | Lower mortality rates |
Cardiothoracic Surgeries | Increased complication rates | Reduced complication rates |
Specialized Centers vs. General Hospitals
There’s a debate on whether specialized centers or general hospitals do better in surgery. Specialized centers often have better results for complex surgeries because of their focus and setup.
Comparative Outcomes
- Specialized centers handle complex cases more efficiently, leading to better care.
- General hospitals can handle many cases but might not have the same level of specialized care.
Surgeon Experience and Specialization Impact
Surgeon experience and specialization greatly affect surgery results. More experienced surgeons do better because they have honed their skills and can handle problems well.
The Role of Specialization
- Surgeons who focus on certain areas do better in those areas because of their deep knowledge.
- Staying current with new techniques also helps improve surgery results.
Improving Outcomes in High-Risk Surgeries
To improve outcomes in high-risk surgeries, we need a mix of new technologies and smart strategies. These surgeries are complex and can lead to serious problems. So, they need careful planning and execution.
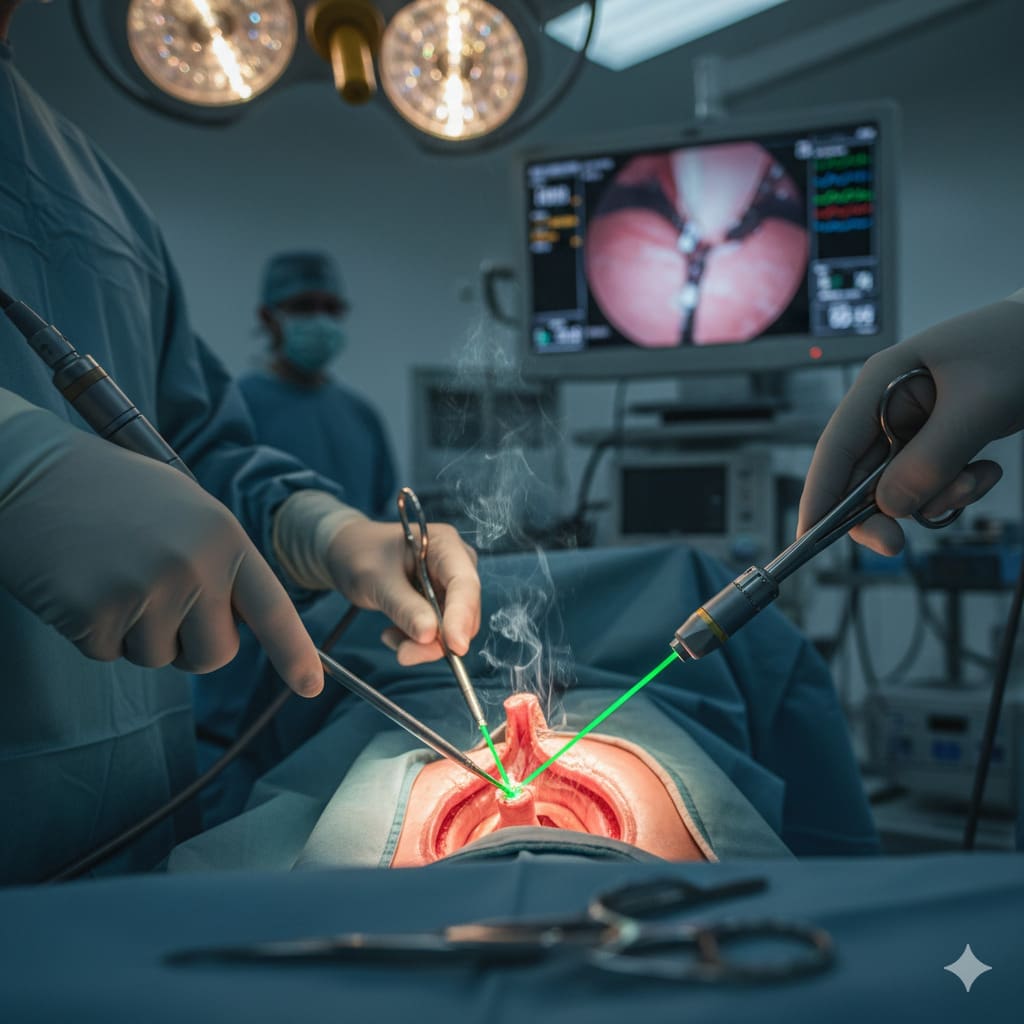
Technological Advancements
New technologies are key to bettering high-risk surgery results. 3D imaging and intraoperative MRI help plan and do surgeries more accurately. Robot-assisted surgery also helps, giving surgeons better control and vision.
- Enhanced precision through robotic systems
- Improved visualization with advanced imaging
- Better patient outcomes due to minimally invasive techniques
Using these technologies in surgery has shown great promise. Studies show fewer complications and faster recovery times for patients.
Multidisciplinary Approach Benefits
A team effort is essential for managing high-risk surgeries. This team includes surgeons, anesthesiologists, radiologists, and more. They work together to improve patient care.
- Comprehensive preoperative assessment
- Coordinated care plans
- Enhanced postoperative support
This teamwork not only helps with surgery results but also improves long-term health.
Pre-habilitation and Enhanced Recovery Protocols
Pre-habilitation and ERAS protocols aim to boost patient health before and after surgery. Pre-hab helps patients get physically and nutritionally ready. ERAS makes post-surgery care more efficient.
- Nutritional optimization
- Physical conditioning
- Standardized postoperative care pathways
These efforts help lower complications, reduce hospital stays, and improve patient results.
Ethical Considerations in High-Risk Procedures
High-risk surgeries bring up big ethical questions for both patients and doctors. These surgeries need careful thought about the benefits and risks. They can lead to serious problems or even death.
Informed Consent Challenges
Getting informed consent is a big issue in high-risk surgeries. Doctors must explain the surgery and its risks clearly. They also need to make sure patients understand and can make choices based on their own values.
Informed consent is hard because the information is complex. Patients might feel overwhelmed. Doctors have to find a balance between giving enough info and not stressing the patient too much.
Quality of Life vs. Survival Considerations
High-risk surgeries often mean choosing between quality of life and survival. Patients and their families have to think if living longer is worth the risk of a lower quality of life after surgery.
Doctors play a key role in helping patients and families make these tough choices. They need to respect the patient’s wishes while making sure they know what to expect.
Palliative Intent Surgeries
Some high-risk surgeries are done to ease suffering, not to cure the disease. These surgeries raise questions about the benefits and risks.
Deciding on these surgeries needs careful thought. Doctors must consider the patient’s values, how much relief the surgery might bring, and its impact on quality of life. Making these decisions ethically means understanding the goals of care and what outcomes are likely.
Future Directions in Improving Surgical Success Rates
New technologies and personalized medicine are changing how we do surgery. They are making high-risk surgeries safer. We’re seeing better results thanks to these advancements.
Emerging Technologies and Techniques
New tools like robotic-assisted surgery, artificial intelligence (AI), and augmented reality (AR) are shaping surgery. They make procedures more precise and help surgeons make better decisions.
Robotic surgery gives surgeons better control and vision. AI helps predict how patients will do and spot problems early. AR gives surgeons real-time data, helping them navigate complex areas.
Personalized Risk Assessment Models
New models are being made to guess how well surgery will go for each person. They look at genetics, medical history, and lifestyle. This makes risk assessments more accurate.
With these models, doctors can decide if surgery is right for each patient. This approach is expected to lead to better results and fewer complications.
Research Priorities for High-Risk Procedures
Research is key to understanding what makes surgery successful. It’s looking into new tech, surgical methods, and ways to help patients recover faster.
By focusing on these areas, we can keep improving surgery. It’s a team effort between doctors, researchers, and industry experts. Together, they aim to bring new ideas into practice.
Conclusion: Navigating Decisions About High-Risk Surgeries
Deciding on high-risk surgeries needs a deep understanding of risks and possible results. This article has looked at many high-risk surgeries, their complexity, and how success rates are affected.
It’s key to think about the good things a surgery might do versus the bad. Patients and doctors must talk openly. They should think about the patient’s health, the surgeon’s skill, and the hospital’s quality.
Knowing how high-risk surgeries work helps people make better choices. This knowledge lets patients understand the risks and benefits. It helps them make informed decisions, leading to better health.
FAQ
What is considered a high-risk surgery?
High-risk surgeries are those with a higher chance of complications or death. This is often due to the surgery’s complexity, the patient’s health, or other factors.
How are surgical success rates measured?
Success rates are measured by looking at things like death rates, complication rates, and how long patients stay in the hospital. They also look at long-term survival and recovery.
What factors influence surgical success rates?
Several things can affect success rates. These include the patient’s health, the surgeon’s skill, post-operative care, and the hospital’s quality.
What is the Whipple procedure, and what are its success rates?
The Whipple procedure is a complex surgery for pancreatic cancer. Success rates vary, with death rates between 2-5% in top centers. Long-term survival depends on the cancer’s stage and other factors.
How successful are esophageal resection and reconstruction surgeries?
Success rates for these surgeries vary. They are complex and can have high complication rates. The success depends on the technique and the surgeon’s experience.
What are the outcomes for high-risk cardiovascular procedures like aortic aneurysm repair?
Outcomes for these procedures can be tough. Death and complication rates are influenced by the patient’s health, the aneurysm’s complexity, and the surgeon’s experience.
How successful are neurosurgical procedures like brain tumor removal?
Success depends on the tumor’s location, size, and type, and the patient’s health. Success rates vary, with some procedures having higher complication rates or lower survival rates.
What are the challenges and success rates of organ transplantation?
Organ transplantation faces challenges like rejection rates and survival statistics. Success rates depend on the organ, the recipient’s health, and post-transplant care.
How do patient-specific factors like age and comorbidities affect surgical success?
Age, comorbidities, and health status can greatly impact success rates. Older patients or those with many health issues face higher risks.
Can the success of surgeries be improved with certain strategies?
Yes, using new technologies, team approaches, pre-habilitation, and recovery protocols can help. These strategies can reduce complications and improve recovery.
What are the ethical considerations in high-risk surgical procedures?
Ethical considerations include informed consent and balancing life quality with survival. Surgeries with palliative intent require careful discussions between patients, families, and healthcare providers.
What future directions are being explored to improve surgical success rates?
Future directions include new technologies, personalized risk models, and focused research. These aim to improve outcomes in high-risk surgeries.
References
The Lancet. Evidence-Based Medical Insight. Retrieved from
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(15)60806-3/fulltext