Asthma affects millions worldwide. It’s important to understand its causes for prevention and management. Asthma development is a mix of genetic and environmental factors.what causes asthmaWhat Is Dyspnoea on Exertion and What Causes Shortness of Breath During Activity?
Genetic predisposition and environmental exposures are key in asthma development. This often starts early in life. Studies show that family history, allergies, and work exposures raise the risk.
Key Takeaways
- Asthma is a complex condition influenced by genetic and environmental factors.
- Family history and allergies are significant risk factors.
- Occupational exposures can increase asthma risk.
- Early life exposures are critical in asthma development.
- Understanding risk factors is key to prevention and management.
The Nature of Asthma: A Complex Respiratory Condition

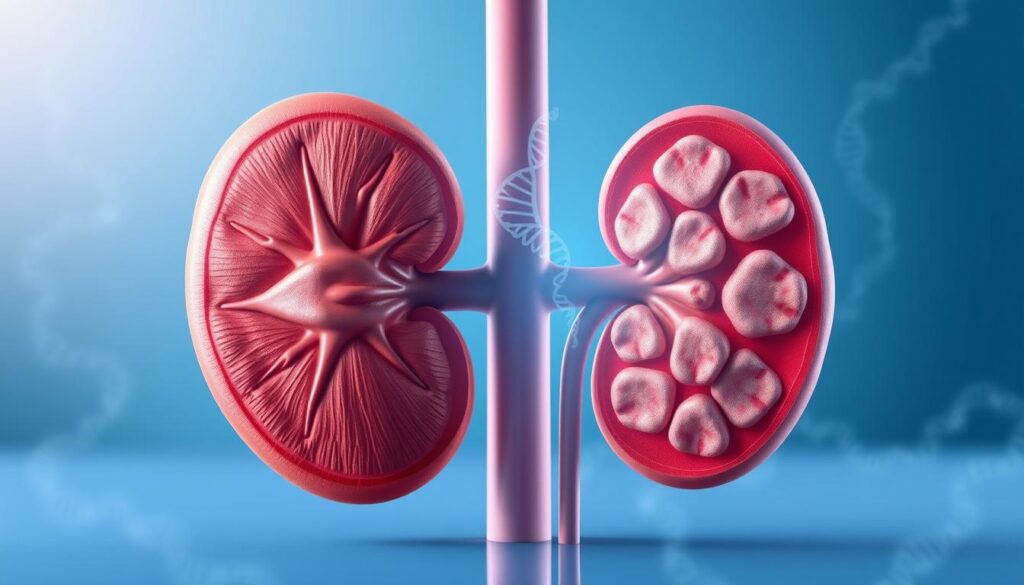
Asthma is a complex condition with chronic inflammation, airway obstruction, and hyperresponsiveness. It makes your airways narrow and swell, producing extra mucus. This makes breathing hard and can cause coughing, wheezing, and shortness of breath.
Defining Asthma and Its Characteristic Symptoms
Asthma is marked by symptoms like wheezing, coughing, shortness of breath, and chest tightness. These symptoms can change in severity and frequency. This makes asthma hard to manage.
Asthma Symptoms: Wheezing, coughing, shortness of breath, chest tightness.
How Asthma Affects the Airways and Breathing
Asthma causes inflammation in the airways, leading to obstruction. This obstruction can get worse with triggers like allergens, infections, and environmental factors. Knowing how asthma affects the airways is key to managing it.
|
Aspect of Asthma |
Effect on Airways |
Impact on Breathing |
|---|---|---|
|
Chronic Inflammation |
Narrowing and swelling of airways |
Difficulty breathing, wheezing |
|
Airway Obstruction |
Reduced airflow |
Shortness of breath, coughing |
|
Hyperresponsiveness |
Exaggerated response to triggers |
Chest tightness, wheezing |
Understanding asthma’s complex nature helps us see the challenges it poses. Effective management goes beyond treating symptoms. It also involves addressing the underlying causes and triggers.
The Multifactorial Origins of Asthma Development

Asthma comes from a mix of genes and the environment. It’s not just one thing that causes it. Instead, many factors work together in complex ways.
The Interplay Between Genetics and Environment
Genes and the environment both play a part in asthma. Genetic factors can make some people more likely to get asthma. But, it’s often the environment that actually triggers it.
Things like allergens, pollutants, and infections can start asthma in people who are already at risk. The hygiene hypothesis says that not being exposed to enough germs in childhood might increase asthma risk.
Why Pinpointing a Single Cause Is Challenging
Finding one cause for asthma is hard because it’s so complex. It affects people differently and can be caused by many things. This makes it tough to find just one reason.
So, doctors and researchers look at risk factors and triggers instead. Knowing these can help in preventing and managing asthma.
The Concept of Asthma Phenotypes
Asthma phenotypes show that asthma is not just one disease. It’s a group of different conditions. Each has its own causes, symptoms, and treatments.
Knowing the specific type of asthma a person has helps doctors give better care. There are many types, like allergic asthma and asthma caused by exercise.
Understanding how genes, environment, and other factors interact is key to fighting asthma. By recognizing these connections, we can improve how we diagnose, treat, and prevent asthma.
“Asthma is a complex disorder with multiple phenotypic expressions, requiring a comprehensive approach to diagnosis and treatment.”
Genetic Predisposition: The Role of Family History
Genetic predisposition is a key factor in determining asthma risk. This is more true when there’s a family history of asthma. Research shows that people with a family history of asthma are more likely to get it.
Hereditary Patterns in Asthma Development
Family history is very important in asthma development. If you have a parent with asthma, you are three to six times more likely to get asthma. This shows how important genetics are in asthma.
Studies also show that people with a family history of allergies are at higher risk. This includes allergic rhinitis and eczema. It suggests that there’s a shared genetic link among these conditions.
Specific Genes Associated with Asthma Risk
Several genes have been found to increase asthma risk. These genes affect airway function and immune response. For example, genes that control IgE antibodies, which are key in allergic reactions, are linked to asthma.
More research is needed to find new genetic variants linked to asthma. Knowing these genetic factors can help identify people at higher risk. It could lead to targeted interventions.
Epigenetic Factors in Asthma Development
Epigenetic factors also play a role in asthma development. These factors affect gene expression without changing the DNA. They can be influenced by environmental exposures and may contribute to asthma’s increasing prevalence.
Studies have shown that epigenetic changes can impact genes involved in airway inflammation and responsiveness. This shows how genetics and environment interact in asthma development.
|
Genetic Factor |
Description |
Impact on Asthma Risk |
|---|---|---|
|
Family History |
Having a parent with asthma |
Increases risk 3-6 times |
|
Specific Genes |
Genes regulating IgE production |
Associated with allergic asthma |
|
Epigenetic Modifications |
Environmental influences on gene expression |
Affects airway inflammation and responsiveness |
Early Life Exposures and Asthma Risk
Early life exposures are key in figuring out if someone will get asthma. The time before birth and early childhood are very important. These times are when many things can affect how well our lungs work.
Prenatal Influences on Respiratory Development
Things that happen before a baby is born can affect their lungs and asthma risk. If a mom smokes while pregnant, it can harm her baby’s lungs. Exposure to cigarette smoke in utero can change how lungs work and make breathing harder.
Critical Windows of Immune System Development
The immune system grows a lot before and after birth. Critical windows are times when a baby or young child is very sensitive to things around them. These times can shape how the immune system works and affect asthma risk.
Maternal Health Factors Affecting Fetal Lung Development
Things like what a mom eats and how stressed she is can affect her baby’s lungs. A good diet and not being too stressed can help the baby’s lungs and immune system grow right. For example, eating enough folate and omega-3 fatty acids can lower asthma risk in kids.
|
Maternal Health Factor |
Impact on Fetal Lung Development |
Asthma Risk |
|---|---|---|
|
Maternal Smoking |
Altered lung structure and function |
Increased |
|
Maternal Nutrition |
Influences fetal immune system development |
Variable, depending on nutrient intake |
|
Maternal Stress |
Potential impact on fetal development through stress hormones |
Increased |
Knowing how early life exposures affect asthma risk helps us prevent it. By changing things we can, we can lower asthma rates and improve breathing health.
Environmental Triggers: What Causes Asthma in Susceptible Individuals
Asthma can start in people who are more likely to get it because of environmental factors. We can control or lessen these factors. Knowing what triggers asthma is key to stopping symptoms and managing the disease well.
Indoor Air Quality Concerns
Indoor air quality is a big issue for asthma triggers. Pollutants like dust mites, pet dander, mold, and chemicals from household items are common indoors.
- Dust mites: These tiny creatures live in bedding, carpets, and furniture. Their waste can make people with asthma worse.
- Pet dander: Proteins in pets’ skin, saliva, and urine can cause allergies and asthma.
- Mold: When it’s too damp, mold grows. Its spores can make asthma symptoms worse.
- VOCs: Chemicals from cleaning products, paints, and adhesives can irritate airways and trigger asthma.
To improve indoor air, clean often, use allergen-proof bedding, keep humidity right, and make sure air circulates well.
|
Indoor Air Pollutant |
Asthma Impact |
Mitigation Strategy |
|---|---|---|
|
Dust Mites |
Allergic reactions, asthma symptoms |
Allergen-proof bedding, regular washing |
|
Pet Dander |
Allergic reactions, asthma symptoms |
Regular grooming, HEPA filters |
|
Mold |
Respiratory issues, asthma exacerbation |
Control humidity, fix leaks promptly |
|
VOCs |
Airway irritation, asthma symptoms |
Use eco-friendly products, ensure ventilation |
Tobacco Smoke Exposure
Being around tobacco smoke is a big risk for asthma. Being exposed to smoke before birth or after birth can make asthma more likely.
“Exposure to tobacco smoke is a significant risk factor for the development of asthma in children and can exacerbate symptoms in individuals with existing asthma.”American Lung Association
To cut down on tobacco smoke, parents and guardians should quit smoking. Also, make homes and public places smoke-free.
Outdoor Pollution and Asthma Development
Outdoor air pollution is another big asthma trigger. Pollutants like PM, O3, NO2, and SO2 can make airways irritated and trigger asthma symptoms.
To lessen outdoor pollution, check air quality indexes, stay inside when it’s bad, and use air purifiers indoors.
By tackling these environmental triggers, we can help prevent asthma in those at risk. We can also improve life for those already living with asthma.
The Hygiene Hypothesis: Too Clean for Our Own Good?
The hygiene hypothesis suggests that our clean environments might be causing more asthma. It challenges the idea that being clean is always good for us. It says that a bit of dirt in childhood is key for a strong immune system.
Early Microbial Exposure and Immune System Development
Being exposed to many microorganisms early on shapes our immune system. Studies show kids who meet lots of microbes are less likely to get asthma. This helps their immune system stay balanced and avoid overreacting.
Key factors influencing early microbial exposure include:
- Presence of siblings
- Exposure to pets
- Daycare attendance
- Farm living
Modern Lifestyle Changes and Rising Asthma Rates
Our modern lives have made us less exposed to good microbes. Antibiotics, better hygiene, and city living have all played a part. This means our immune systems don’t get the challenge they used to, making us more likely to get asthma.
Farm Living and Reduced Asthma Risk
Kids who live on farms are less likely to get asthma. This is because they’re exposed to many different microbes. Being around farm animals and drinking unpasteurized milk helps protect them.
Understanding the hygiene hypothesis helps us see how our environment affects asthma. This knowledge can help us find ways to lower asthma risk, mainly in high-risk groups.
Respiratory Infections and Asthma Development
Respiratory infections, like those in early childhood, are a big risk for asthma. We’ll look at how these infections lead to asthma. This includes viral infections and their effects on the lungs.
Viral Infections in Early Childhood
Viral respiratory infections are common in young kids. They can really hurt the growing lungs. Respiratory syncytial virus (RSV) and rhinoviruses are big culprits.
These viruses can cause inflammation and damage in the airways. This can make kids more likely to get asthma. Studies show that bad viral infections early on can lead to more wheezing and asthma.
The Link Between Bronchiolitis and Future Asthma
Bronchiolitis, often caused by RSV, is a big deal in babies. It’s a lower respiratory tract infection. Research shows a strong link between bronchiolitis in young kids and asthma later on.
The reasons for this link are complex. It involves genetics, environment, and how the body fights off the infection.
How Infections May Alter Immune Responses
Viral respiratory infections can change how the immune system works. This can lead to asthma. For example, these infections can make the immune system lean more towards Th2 responses. This is linked to allergic inflammation and asthma.
Also, early infections can shape the airway epithelium and immune regulation. This can make kids more likely to get asthma.
It’s key to understand how respiratory infections lead to asthma. This helps in finding ways to prevent and manage asthma. By spotting high-risk kids early, doctors can start interventions to lower asthma risk.
Allergic Conditions as Asthma Predictors
Understanding allergic conditions is key to predicting asthma risk. Allergic conditions, such as eczema and hay fever, are strong predictors of asthma development. We will explore how these conditions are linked to asthma and what this means for individuals at risk.
The Atopic March: From Eczema to Asthma
The atopic march describes the progression from eczema to asthma and other allergic conditions. This concept highlights the link between early allergic manifestations and the later development of respiratory allergies. The atopic march is a significant indicator of asthma risk, as it often begins with skin manifestations like eczema in early childhood.
How Allergic Sensitization Affects Asthma Risk
Allergic sensitization is the process by which the body becomes sensitive to specific allergens, leading to allergic reactions. This sensitization plays a key role in the development of asthma. When an individual becomes sensitized to airborne allergens, their risk of developing asthma increases significantly. Understanding and managing allergic sensitization is, therefor, critical in preventing asthma.
The Role of IgE Antibodies in Allergic Asthma
IgE antibodies are central to the development of allergic reactions, including those that lead to asthma. These antibodies trigger the release of chemical mediators, which cause the symptoms associated with allergic asthma. The presence of IgE antibodies is a hallmark of allergic asthma, and their role in the disease process is well established.
By understanding the link between allergic conditions, such as eczema and hay fever, and asthma, we can better identify individuals at risk. We can then intervene early to prevent the development of asthma. This knowledge highlights the importance of managing allergic conditions in preventing asthma.
Occupational Asthma: Workplace Exposures and Risk
Occupational asthma is a serious health issue in many workplaces. It happens when workers are exposed to certain substances. These exposures can cause asthma symptoms.
Industries and Occupations at High Risk
Some jobs are more likely to lead to occupational asthma. For example, farming, hairdressing, and manufacturing jobs expose workers to asthma triggers. Farmers might breathe in organic dusts, while manufacturing workers face chemicals and irritants.
- Farmers and agricultural workers exposed to organic dusts
- Hairdressers and beauticians exposed to chemical dyes and fragrances
- Manufacturing workers handling various chemicals and materials
Common Workplace Triggers and Sensitizers
Many substances in the workplace can trigger occupational asthma. Chemicals, dusts, and irritants are common culprits. Knowing these triggers is key to preventing asthma at work.
Common triggers include:
- Isocyanates found in paints and coatings
- Flour dust in bakeries
- Latex proteins in medical gloves
Distinguishing Between Irritant and Allergic Occupational Asthma
Occupational asthma can be either irritant-induced or allergic. Irritant-induced asthma happens after a single, high exposure to an irritant. Allergic asthma develops with repeated exposure to a sensitizer.
It’s important to know the difference for proper diagnosis and treatment.
|
Characteristics |
Irritant-Induced Occupational Asthma |
Allergic Occupational Asthma |
|---|---|---|
|
Exposure Pattern |
Single high-level exposure |
Repeated exposure to sensitizer |
|
Latency Period |
No latency period |
Variable latency period |
Lifestyle Factors Influencing Asthma Development
Modifiable lifestyle factors can greatly affect the risk of getting asthma. We see how lifestyle choices can either make asthma worse or better. This shows that what we do can change our asthma risk.
Impact of Diet and Nutrition
Diet and nutrition are key in managing asthma. Eating lots of fruits, veggies, and omega-3s can help. But, eating too much processed food, sugar, and unhealthy fats can up asthma risk.
Some nutrients, like vitamin D, can help asthma by improving lung function. Vitamins C and E can also reduce stress in the body.
|
Nutrient |
Potential Benefits for Asthma |
Food Sources |
|---|---|---|
|
Omega-3 Fatty Acids |
Reduces inflammation |
Fatty fish, flaxseeds, chia seeds |
|
Vitamin D |
Improves lung function |
Fatty fish, fortified dairy products, sunlight exposure |
|
Antioxidants (Vitamin C, E) |
Reduces oxidative stress |
Fruits, nuts, leafy greens |
Physical Activity and Obesity Connections
Being active and keeping a healthy weight are important for asthma. Exercise can boost lung health and overall well-being. But, being obese can lead to more inflammation and higher asthma risk.
Obesity and Asthma Risk
- Obesity increases the risk of developing asthma
- Excess weight can worsen asthma symptoms
- Weight loss can improve asthma control
Stress and Psychological Factors
Stress and mental health can also affect asthma. Chronic stress can make asthma symptoms worse. But, managing stress with meditation and yoga can help overall health.
Knowing how lifestyle affects asthma can help us make better choices. This can lower our risk and better manage symptoms.
Preventing Asthma: Modifiable Risk Factors
To prevent asthma, we must understand and tackle its modifiable risk factors. By doing so, we can lower the chance of getting asthma.
Reducing Environmental Exposures
One key way to prevent asthma is to cut down on environmental triggers. This means avoiding tobacco smoke, both before and after a baby is born. Tobacco smoke is a big risk factor for asthma.
Also, making indoor air cleaner is important. This can be done by reducing dust mites, pet dander, and mold. Using allergen-proof bedding and keeping humidity levels right can help a lot.
Early Interventions for High-Risk Children
Spotting children at risk of asthma and starting early interventions is very effective. This includes watching kids with asthma in their family or who got sick early.
Early steps might include giving kids inhaled corticosteroids if they show asthma signs. Teaching parents how to spot and handle asthma symptoms is also key.
|
Intervention Strategy |
Description |
Potential Benefits |
|---|---|---|
|
Monitoring High-Risk Children |
Regular check-ups for children with a family history of asthma or early respiratory infections. |
Early detection of asthma symptoms, timely intervention. |
|
Inhaled Corticosteroids |
Use of corticosteroid medication for children showing early signs of asthma. |
Reduced inflammation, prevention of asthma symptoms. |
|
Parental Education |
Educating parents on recognizing and managing asthma symptoms. |
Improved asthma management, reduced hospitalizations. |
Breastfeeding and Its Protective Effects
Breastfeeding might help protect against asthma, mainly when done for at least 4 months. The exact reasons are not clear, but it’s thought to shape the baby’s immune system.
Even though more studies are needed, breastfeeding is advised as a way to prevent asthma, mainly in high-risk groups.
Conclusion: Understanding the Complex Origins of Asthma
Asthma is a complex condition with many risk factors. These include genetic predisposition, early life exposures, and environmental triggers. We’ve looked at how these factors work together to cause asthma.
The exact cause of asthma is not fully understood. It’s thought to come from a mix of genetic and environmental factors. Knowing what causes asthma and how risk factors play a part is key to managing it.
Even though asthma can’t be cured, its symptoms can be controlled. By tackling risk factors, we can lessen the severity and frequency of asthma attacks. This helps healthcare providers create better plans and gives patients the tools to manage their asthma.
As we learn more about asthma, it’s clear we need a complete approach to tackle it. By working together, we can make a big difference in the lives of those with asthma.
FAQ
What is asthma and how does it affect the airways?
Asthma is a chronic respiratory condition. It causes inflammation, obstruction, and hyperresponsiveness in the airways. Symptoms include wheezing, coughing, shortness of breath, and chest tightness, making breathing difficult.
Are people born with asthma or does it develop later in life?
Asthma can be present from birth or develop later. It depends on a mix of genetic and environmental factors.
What are the main risk factors for developing asthma?
Key risk factors include genetic predisposition and early life exposures. Environmental triggers like tobacco smoke and outdoor pollution also play a role. Respiratory infections, allergic conditions, and lifestyle factors such as diet and physical activity are important too.
How does genetic predisposition contribute to asthma development?
Genetic factors significantly influence asthma development. Specific genes are linked to asthma risk. Hereditary patterns also affect an individual’s chance of developing the condition.
Can environmental triggers cause asthma in susceptible individuals?
Yes, environmental triggers can cause asthma symptoms. Indoor air quality concerns, tobacco smoke exposure, and outdoor pollution are examples.
What is the hygiene hypothesis and how does it relate to asthma?
The hygiene hypothesis suggests a lack of early microbial exposure may lead to more asthma. Modern lifestyle changes have reduced exposure to beneficial microorganisms, affecting immune system development.
How do respiratory infections affect asthma development?
Respiratory infections, like viral infections in early childhood, can increase asthma risk. They may alter immune responses, contributing to asthma development.
Can allergic conditions predict the development of asthma?
Yes, allergic conditions like eczema and allergic sensitization can predict asthma. The atopic march describes the progression from eczema to asthma.
What is occupational asthma and how can it be prevented?
Occupational asthma is caused by workplace exposures to specific triggers and sensitizers. It can be prevented by reducing exposure and implementing protective measures in high-risk industries and occupations.
How can lifestyle factors influence asthma development?
Lifestyle factors like diet, physical activity, and stress can influence asthma development. A healthy diet and regular physical activity may reduce asthma risk.
Can asthma be prevented by modifying risk factors?
Yes, modifying risk factors can help prevent asthma. Reducing environmental exposures, implementing early interventions for high-risk children, and promoting breastfeeding are effective strategies.
What causes asthma?
The exact cause of asthma is unknown. It is believed to result from a complex interplay of genetic, environmental, and lifestyle factors.
How do people develop asthma?
People develop asthma due to genetic predisposition, environmental triggers, and lifestyle factors. These factors lead to chronic inflammation and airway hyperresponsiveness.
Are you born with asthma?
Asthma can be present from birth or develop later. It depends on genetic and environmental factors.
What is the main cause of asthma?
Asthma’s main cause is a complex interplay of genetic, environmental, and lifestyle factors. These factors contribute to its development.
References
World Health Organization. Evidence-Based Medical Guidance. Retrieved from
https://www.who.int/news-room/fact-sheets/detail/asthma