Chest radiography is the most common imaging test worldwide. Yet, spotting abnormal chest x-rays can be tough. At Liv Hospital, we know how vital it is to find common lung x-ray issues in healthcare today.Quick visual guide to identifying seven common lung x ray abnormalities, including nodules, effusions, and masses.
Studies show that atelectasis and patchy pulmonary opacity are often seen, like in pulmonary embolism. Spotting these signs is key to better patient care.
We’ll show you the seven most common lung x-ray abnormalities. Our visual guide aims to improve diagnosis and care for patients.
Key Takeaways
- Chest radiography is a key tool in healthcare today.
- Common lung x-ray issues include atelectasis, consolidation, and pleural effusions.
- Spotting these issues is vital for patient care.
- Liv Hospital offers international expertise in pulmonary imaging.
- Knowing common chest x-ray issues helps doctors diagnose better.
The Critical Role of Chest Radiography in Pulmonary Diagnosis

Chest radiography is key in finding lung problems worldwide. It helps us spot many lung conditions. This makes it a vital tool in healthcare.
Global Prevalence of Chest X-Rays in Clinical Practice
Chest X-rays are the most common imaging test globally. They are quick and give important info. We use them in many situations, from regular checks to urgent diagnoses.
They help us screen, diagnose, and watch lung diseases. The abnormal lung X-ray images show us a lot about a patient’s health. This helps us decide on treatment.
Fundamentals of Radiographic Interpretation
Reading chest X-rays needs a careful method. We must check the image quality, patient position, and any artifacts. Knowing these basics is key for correct diagnosis.
We look for signs of chest X-ray abnormality lung issues like atelectasis and consolidation. Spotting these signs is important for accurate diagnosis.
Recognizing Normal versus Abnormal Patterns
Telling normal from abnormal X-ray patterns is a big skill. We need to know the normal anatomy and its changes to spot problems. Common abnormal X-ray of chest findings include opacities and nodules.
By understanding how to read X-rays and knowing how common they are, we can get better at diagnosing. This knowledge is vital for better patient care.
Systematic Approach to Identifying Lung X-Ray Abnormalities

Looking closely at lung X-rays is key to spotting problems and making correct diagnoses. We need to carefully study the images, taking into account several factors. This helps us make accurate diagnoses.
Methodical Review of Lung Zones
It’s important to methodically check each lung zone for abnormalities. We split the lungs into different areas and look at each one carefully. This way, we make sure we don’t miss anything.
- Examine the upper, middle, and lower lung zones.
- Compare the left and right lungs for symmetry.
- Check for any areas of increased or decreased opacity.
Recognizing Radiographic Density Asymmetry
Spotting radiographic density asymmetry is key to finding lung problems. Asymmetry can mean many things, like consolidation or atelectasis. We must compare the density of both lungs to spot any differences.
Research shows that lung issues on chest X-rays can be subtle and not clear-cut. They need careful comparison of both lung zones to spot.
Comparative Analysis Techniques
Using comparative analysis techniques is essential for accurate diagnosis. By comparing current X-rays with past ones, we can see changes and track lung problems over time.
- Compare current X-rays with previous images.
- Use digital tools to enhance image quality and facilitate comparison.
- Consider clinical history and symptoms when interpreting X-ray findings.
Atelectasis: Visual Patterns of Lung Collapse
Healthcare professionals need to know how to spot atelectasis on chest X-rays. Atelectasis shows up as denser areas and less lung volume. It can take many forms, like resorptive, relaxation, adhesive, cicatricial, and round atelectasis.
Radiographic Hallmarks and Distribution Patterns
Atelectasis shows up on X-rays with denser areas and shifted fissures. It can happen in any lung zone, but some types prefer certain areas.
Key Radiographic Features:
- Homogeneous or heterogeneous opacification
- Volume loss indicated by displaced fissures or hilar/mediastinal shift
- Compensatory changes in adjacent lung zones
Compensatory Hyperinflation Recognition
When part of the lung expands to fill a collapsed area, it’s called compensatory hyperinflation. This can be seen on X-rays as less dense areas and more lung volume. It’s a key way the lung tries to keep working despite collapse.
“The recognition of compensatory hyperinflation is vital as it indicates the lung’s attempt to maintain respiratory function despite the collapse.”
Clinical Correlation and Management Implications
Understanding atelectasis means knowing its causes and how it affects patients. Causes include blockages, post-surgery, or long-term lung diseases. Treatment can range from simple steps like physiotherapy to more serious actions in severe cases.
|
Type of Atelectasis |
Causes |
Management |
|---|---|---|
|
Resorptive Atelectasis |
Obstruction of airway |
Relief of obstruction, bronchoscopy |
|
Cicatricial Atelectasis |
Chronic scarring |
Management of underlying disease |
|
Relaxation Atelectasis |
Pleural effusion or pneumothorax |
Drainage of effusion or pneumothorax |
Knowing how to spot atelectasis and its effects helps doctors treat lung collapse better. This can lead to better health outcomes for patients.
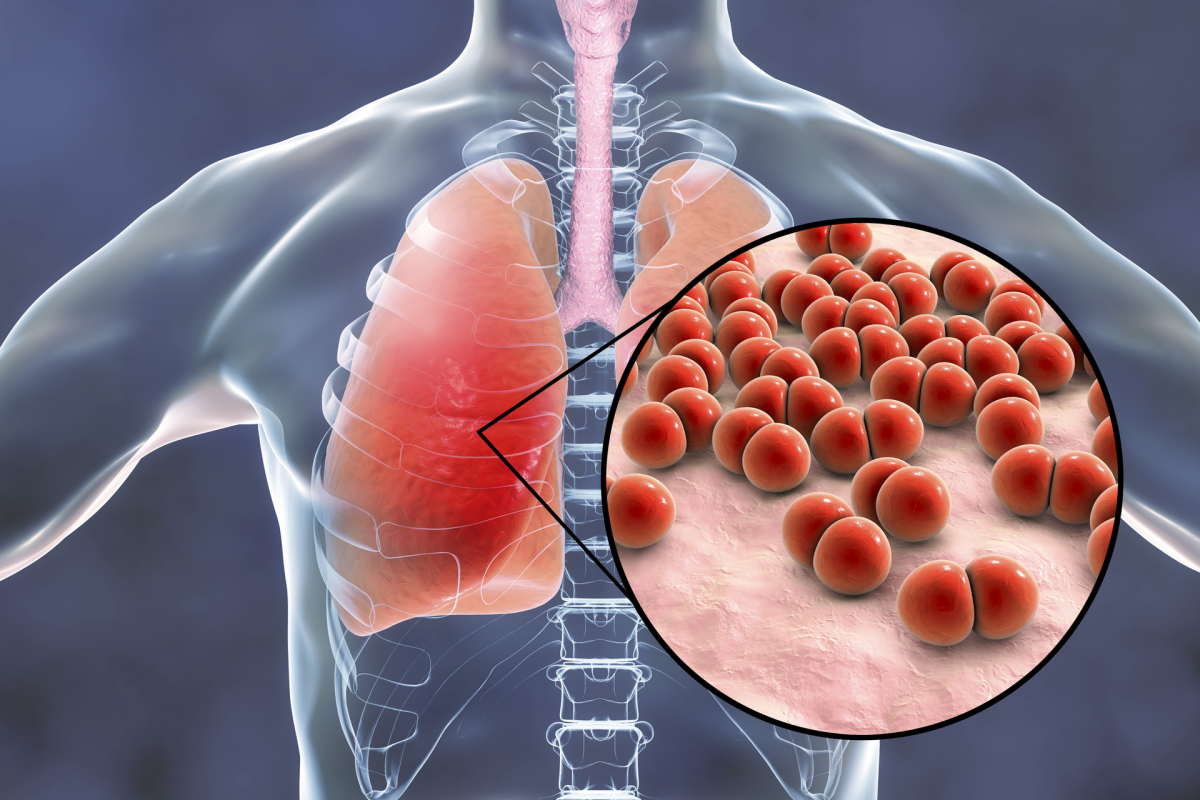
Consolidation: Identifying Airspace Opacification
Consolidation shows up as a darker area on chest X-rays. It means the air sacs in the lungs are filled with fluid or cells. This is key in spotting lung problems like pneumonia.
Classic Radiographic Features and Silhouette Signs
Consolidation is marked by airspace opacification and air bronchograms. Air bronchograms show the bronchi are filled with air, while the alveoli are full of fluid. Silhouette signs are also key; they hide the outline of nearby structures when consolidation is close.
The silhouette sign helps pinpoint where consolidation is. For example, right middle lobe consolidation can hide the right heart border.
Distribution Patterns and Diagnostic Significance
The way consolidation spreads can hint at its cause. Lobar consolidation often points to pneumococcal pneumonia. Multifocal consolidation might suggest other issues like multilobar pneumonia or ARDS.
Knowing how consolidation spreads is vital for figuring out what’s causing it. A lobar pattern usually means a bacterial infection. But a diffuse pattern could point to something more complex or widespread.
Distinguishing from Other Opacities
Telling consolidation apart from other lung issues is key for correct diagnosis. Atelectasis and pulmonary nodules are often confused with consolidation. Atelectasis shows volume loss and displaced fissures, but consolidation doesn’t usually shrink the lung.
Looking closely at the X-ray features, like air bronchograms and how it spreads, helps tell consolidation apart from other lung problems.
Ground Glass Opacities: Subtle Findings and Clinical Significance
Ground glass opacities are tricky to spot on chest X-rays because they are so subtle. They look like a hazy patch in the lungs. This patch doesn’t block the view of the airways or blood vessels inside. Spotting these opacities is key because they can signal many lung problems, like infections or early signs of scarring.
Recognition Challenges on Plain Radiographs
Finding ground glass opacities on chest X-rays is hard because they are faint. Things like how the X-ray is taken and the patient’s position can make them harder to see. Also, it takes a lot of skill to tell these opacities apart from other lung issues on X-rays.
Disease Progression Patterns
About 55% of early lung problems show up as ground glass opacities. In 20% of cases, these opacities can turn into something more serious. How a disease gets worse can depend on the cause. Watching how the disease changes over time is key to treating it right.
Correlation with Advanced Imaging Findings
While chest X-rays are often the first step, high-resolution CT (HRCT) scans give more detailed views. HRCT scans can show more about the extent and spread of ground glass opacities. This helps doctors make a better diagnosis and plan treatment.
In short, ground glass opacities are important but hard to spot on chest X-rays. Knowing how to recognize them and what they mean is vital for good care.
Pulmonary Nodules: Focal Abnormalities Detection Guide
Pulmonary nodules are common on chest X-rays. They need careful checking to see if they’re serious. These spots can be harmless or cancerous, and finding them early is key to treating lung diseases.
Size Classification and Morphological Features
The size and shape of pulmonary nodules tell us a lot. Nodules are sized based on their diameter. Small ones are under 5 mm, 5-10 mm are small, and over 10 mm are big and need more looking into.
The shape of the nodule also matters. Calcification, cavitation, or irregular margins give clues. For example, smooth edges often mean it’s not cancer, but spiky edges might be a worry.
Solitary versus Multiple Nodule Patterns
Whether there’s one nodule or many changes how we look at it. Solitary nodules are checked based on size, shape, and risk of cancer.
Multiple nodules might mean cancer has spread or something else is going on. How these nodules are spread out and what they look like helps figure out what’s happening.
Risk Assessment and Management Algorithms
Figuring out the risk of pulmonary nodules involves looking at age, smoking history, and nodule details. Management plans use these to decide on next steps, like more scans or biopsies.
The Fleischner Society has guidelines for these nodules. Low-risk patients with small nodules might just need watching. But those at higher risk or with bigger nodules might need more tests, like PET-CT or biopsies.
Cavitary Lesions: Recognizing Air-Containing Lung X-Ray Abnormalities
Cavitary lesions are important to spot on chest X-rays. They can be signs of different health issues. Knowing what they mean is key for doctors to make the right diagnosis.
Wall Characteristics and Diagnostic Implications
The look of the walls of cavitary lesions tells doctors a lot. Thin-walled cavities might be harmless or related to birth defects. But thick-walled cavities could mean cancer or an infection.
“The thickness and regularity of the cavity wall are critical factors in determining the likelihood of malignancy,” as noted by radiologists. We will examine these characteristics closely to narrow down the differential diagnoses.
Common Etiologies and Differential Considerations
Cavitary lesions can come from many sources. Infectious causes like tuberculosis and lung abscesses are common. Malignant lesions like squamous cell carcinoma can also cause cavities.
- Infections (e.g., tuberculosis, lung abscess)
- Malignancies (e.g., squamous cell carcinoma)
- Autoimmune diseases (e.g., Wegener’s granulomatosis)
When looking at cavitary lesions, we must think about these causes and their typical X-ray signs.
Associated Radiographic Findings
Other X-ray signs can also help doctors understand what’s going on. For example, air-fluid levels might mean a lung abscess. Surrounding consolidation could point to an infection or inflammation.
By studying these signs, doctors can make a more accurate diagnosis. This helps decide the best course of action.
Pleural Effusions and Pneumothorax: Peripheral Lung Abnormalities
When we look at lung X-rays, it’s key to spot signs of pleural effusions and pneumothorax. These issues can greatly affect how well a patient does. We’ll talk about what these lung problems look like on X-rays and why they matter.
Blunting of Costophrenic Angles and Fluid Levels
Pleural effusions happen when fluid builds up in the pleural space. This can make the costophrenic angles look less sharp on chest X-rays. The amount of fluid affects how much the angles are blurred. Also, seeing fluid levels means the effusion might be more complex.
Massive Effusions and Mediastinal Shift
When there’s a lot of fluid in the pleural space, the mediastinum might move away from the fluid side. This movement is important for how we treat the patient. We must look at where the mediastinum is and think about why there’s so much fluid.
Pneumothorax: Visceral Pleural Line Identification
Pneumothorax shows up as a line on chest X-rays. This line is the edge of the lung. We look for it, mainly in the upper lung areas, to spot a pneumothorax. The size of the pneumothorax matters for treatment.
Knowing how to spot pleural effusions and pneumothorax on X-rays helps us better diagnose and treat these issues.
Conclusion: Mastering Lung X-Ray Interpretation in Clinical Practice
Understanding lung x-rays is key for spotting and treating lung diseases. We’ve looked at common issues like atelectasis and consolidation. Knowing these signs helps doctors care for patients better.
To get good at reading lung x-rays, follow a step-by-step guide. Look at lung areas carefully and notice any density changes. This skill helps doctors make accurate diagnoses and plan treatments.
Using pictures of chest x-rays helps spot lung problems. An odd chest x-ray can show many conditions, from mild to serious. Knowing what these signs mean lets doctors give top-notch care.
In short, knowing how to read lung x-rays is a must for doctors. By keeping up with learning and practice, we can better diagnose and treat lung diseases. This skill is vital for giving the best healthcare possible to our patients.
FAQ
What are the most common lung x-ray abnormalities?
Common lung x-ray abnormalities include atelectasis, consolidation, and ground glass opacities. Also, pulmonary nodules, cavitary lesions, pleural effusions, and pneumothorax are common.
How do I differentiate between normal and abnormal patterns on a chest x-ray?
To tell normal from abnormal, we use a systematic method. This involves looking at lung zones and noticing density differences. We also compare different parts of the image.
What are the radiographic hallmarks of atelectasis?
Atelectasis shows up as increased opacity and volume loss. You’ll also see fissures displaced and adjacent lung tissue inflated.
How do I distinguish consolidation from other types of opacities on chest x-rays?
Consolidation has distinct features like homogeneous opacity and silhouette signs. Its distribution patterns help distinguish it from other opacities.
What are ground glass opacities, and how are they recognized on plain radiographs?
Ground glass opacities are subtle, hazy areas. They can be hard to spot on plain radiographs. But, they often match up with CT scan findings.
How are pulmonary nodules classified and managed?
Nodules are sorted by size, shape, and number. Risk assessment and management plans guide further steps and treatment.
What are the characteristic features of cavitary lesions on lung x-rays?
Cavitary lesions have air inside and specific walls. They can be caused by infections or cancers.
How do I identify pleural effusions and pneumothorax on chest x-rays?
Pleural effusions show up as blunted costophrenic angles and fluid levels. Massive effusions can shift the mediastinum. Pneumothorax is seen by the visceral pleural line.
What is the clinical significance of abnormal lung x-ray findings?
Abnormal findings on lung x-rays are very important. They guide further tests, treatment, and monitor disease.
How can I improve my skills in interpreting lung x-rays?
To get better at interpreting lung x-rays, keep learning and practicing. Stay current with guidelines and research. Use a systematic approach to interpretation.
References
World Health Organization. Evidence-Based Medical Guidance. Retrieved from https://www.who.int/publications/i/item/9789240011445























