Community-Acquired Pneumonia (CAP) is a big health problem worldwide. It affects millions and causes a lot of sickness and death. We will look into what CAP is, why it happens, and how it’s classified. This will help doctors and healthcare workers a lot.
CAP is an infection of the lungs that happens outside of hospitals. It’s caused by different germs like bacteria, viruses, and fungi. Knowing about CAP is key to giving the right care and helping patients get better.
At Liv Hospital, our teams use the latest research to care for CAP patients. We want to give a full picture of CAP, including what it is, why it happens, and how it’s sorted.
Key Takeaways
- Understanding CAP is key to giving the right care.
- CAP is an infection of the lungs caused by different germs.
- Liv Hospital uses the latest research to care for CAP patients.
- CAP is a big problem worldwide and leads to a lot of hospital stays.
- Knowing how to sort CAP is important for treating it well.
What You Need to Know About CAP Disease
CAP is a big health problem that affects millions around the world. It’s important to know the basics. Community Acquired Pneumonia is a lung infection that people get outside of hospitals. This is different from pneumonia that people get in hospitals.
The Fundamentals of Community Acquired Pneumonia
CAP is caused by different things like bacteria, viruses, and fungi. The most common bacteria is Streptococcus pneumoniae. Viruses like the influenza virus also cause it. Knowing what causes CAP helps doctors treat it better.
The symptoms of CAP include coughing, fever, and trouble breathing. Some cases are mild and can be treated at home. But, some cases are very serious and need hospital care.
Distinguishing CAP from Hospital-Acquired and Healthcare-Associated Pneumonia
CAP is different from HAP and HCAP. HAP happens 48 hours after someone is in the hospital. It’s often caused by bacteria that are hard to treat. HCAP is pneumonia that people get in places like nursing homes. It also involves hard-to-treat bacteria.
It’s important to know these differences. They help doctors choose the right medicine for treatment. This is based on the type of bacteria and the patient’s situation.
In short, CAP is a big health problem worldwide. It needs a full understanding of its causes, symptoms, and treatments. By knowing the differences and causes, doctors can give better care.
Key Point #1: Definition and Pathophysiology of Community Acquired Pneumonia
Community Acquired Pneumonia is an acute inflammatory response in the lungs. It’s important to understand how it occurs and how the body reacts to it.
Acute Lung Infection in Community Settings
Community Acquired Pneumonia happens outside of hospitals. It’s a big cause of sickness and death worldwide, hitting older adults and those with health issues hard.
The main culprits are bacteria, viruses, and fungi. Streptococcus pneumoniae, Haemophilus influenzae, and viruses like influenza are common offenders.
Inflammatory Response and Lung Tissue Damage
The pathophysiology of CAP involves an acute inflammatory response in the lung. This can damage lung tissue, affecting gas exchange and leading to serious issues.
The body’s immune system kicks in when pathogens are found in the lungs. This leads to the activation of immune cells and the release of cytokines and chemokines. This process can cause lung tissue to become solid, making it hard for oxygen to get to the blood.
Grasping the definition and pathophysiology of CAP is key to finding effective treatments. We’ll dive deeper into its epidemiology, etiology, and classification in the next sections.
Key Point #2: Epidemiology and Global Burden
CAP is a complex disease that affects many people worldwide. It puts a big strain on healthcare systems everywhere. Looking into CAP’s spread shows it hits different groups in various places.
Worldwide Incidence: 1.5 to 14 Cases per 1000 Person-Years
The number of CAP cases varies globally, from 1.5 to 14 per 1000 person-years. This big range comes from different study groups, how they diagnose, and where they are. Knowing these differences helps us make health plans that fit each area’s needs.
United States Impact: 24.8 Cases per 10,000 Adults Annually
In the U.S., CAP hits a lot of adults, with 24.8 cases per 10,000 each year. This leads to a lot of hospital stays and use of healthcare resources. The cost of treating CAP in the U.S. is high, showing we need better ways to manage and prevent it.
CAP as the Third Leading Cause of Hospital Admission
CAP is a top reason for hospital visits, coming in third. This shows how serious CAP is and its big impact on healthcare. The high number of hospital visits for CAP means we need quick and proven treatments to help patients and save money.
In summary, CAP’s global impact is huge, and we must keep studying and working on it. By understanding how CAP spreads and affects people, we can do better to manage and stop it.
Key Point #3: Etiological Agents Behind CAP Disease
The causes of CAP include many different microbes. Knowing these causes is key to treating the disease effectively.
Bacterial Pathogens in Community Acquired Pneumonia
Bacteria are a big reason for CAP. Streptococcus pneumoniae is the top bacterial cause, leading to many CAP cases. Other bacteria like Haemophilus influenzae and Moraxella catarrhalis also play a role.
The types of bacteria causing CAP can change based on age, where you live, and your health. For example, Streptococcus pneumoniae is more common in older people and those with health issues.
Viral Causes of CAP
Viruses are also a big cause of CAP, mainly in certain groups. Influenza viruses are well-known for causing CAP, often during flu seasons. Recently, SARS-CoV-2, the COVID-19 virus, has been linked to CAP, leading to severe cases.
Other viruses, like RSV and adenovirus, can also lead to CAP. This is more common in kids and people with weakened immune systems.
Fungal Pathogens in Community Settings
Fungal causes of CAP are less common but important for some groups, like those with weakened immune systems. Histoplasma capsulatum and Coccidioides species are examples of fungi that can cause CAP. This is more likely in areas where these fungi are common.
Knowing the causes of CAP helps doctors choose the right antibiotics. This knowledge is vital for better treatment and care of patients. The variety of pathogens shows why a detailed approach to diagnosing CAP is needed.
Key Point #4: Classification of Community Acquired Pneumonia
To manage CAP well, knowing its types is key. CAP is divided into typical and atypical forms. This helps doctors figure out how serious it is and what treatment to use.
Typical Bacterial Pneumonia vs. Atypical Forms
CAP is split into two main types. Typical bacterial pneumonia is caused by bacteria like Streptococcus pneumoniae. It shows symptoms quickly, like high fever and cough.
Atypical pneumonia is caused by different bacteria. It starts slower, with symptoms like headache and dry cough.
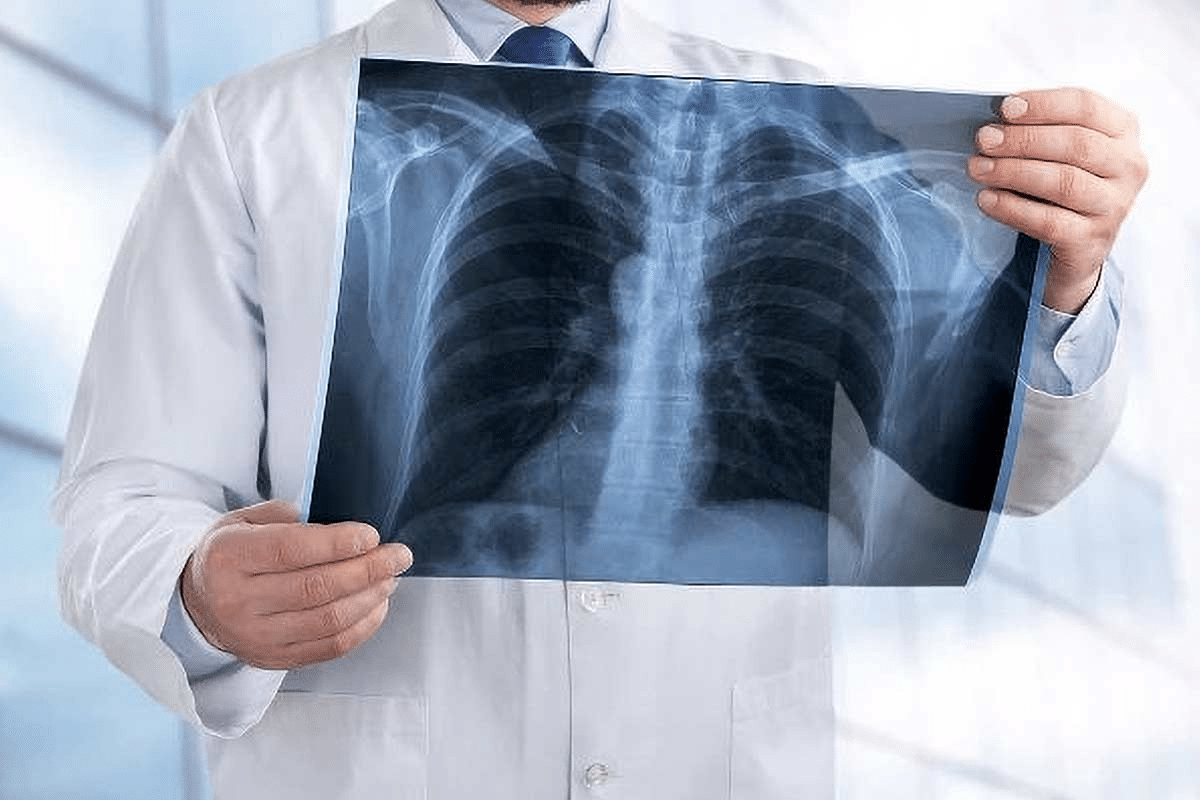
Clinical and Radiological Classification Systems
CAP can also be sorted by how sick it makes you and what the X-rays show. The CURB-65 score helps doctors see how bad it is. This decides if you need to stay in the hospital.
X-rays help doctors see how much of your lung is affected. This helps them decide what tests and treatments you need.
Knowing these ways to sort CAP is important. It helps doctors treat it better and make patients feel better.
Key Point #5: Clinical Presentation and Diagnosis
Understanding community acquired pneumonia (CAP) is key to managing it well. We’ll cover typical symptoms and how doctors diagnose CAP.
Classic Symptoms and Signs of CAP
CAP symptoms can differ, but common ones are cough, fever, and shortness of breath. Cough often brings up yellow or green mucus. Fever is usually high, and some people feel chills.
Shortness of breath can be mild or severe. Physical checks might show fast breathing, heart rate, and sounds from the lungs. In serious cases, patients might look blue or use extra muscles to breathe.
Diagnostic Approaches: Imaging and Laboratory Tests
Diagnosing CAP involves clinical checks, imaging, and lab tests. Chest X-rays are key, showing lung areas affected by pneumonia.
Lab tests help find the cause and how severe the infection is. Tests include blood counts, blood cultures, and sputum tests.
|
Diagnostic Test |
Purpose |
Expected Findings |
|---|---|---|
|
Chest Radiography |
Confirm pneumonia, assess extent |
Lobar or segmental consolidation |
|
CBC |
Assess severity, identify leukocytosis |
Elevated white blood cell count |
|
Blood Cultures |
Identify bacteremia, guide antibiotic therapy |
Positive for pathogens in some cases |
|
Sputum Gram Stain and Culture |
Identify causative pathogen |
Presence of bacteria, neutrophils |
These methods help doctors confirm CAP, find the cause, and see how bad it is. This guides the right treatment.
Severity Assessment Tools for CAP Management
Severity assessment tools are key in managing CAP. They help healthcare providers make smart decisions. These tools show how severe Community Acquired Pneumonia is, guiding treatment and hospital needs.
CURB-65 and Pneumonia Severity Index
CURB-65 and the Pneumonia Severity Index (PSI) are two main tools. CURB-65 is a simple score that looks at confusion, urea levels, respiratory rate, blood pressure, and age. The PSI is more detailed, using many factors to predict risk of death.
CURB-65 Score: Scores range from 0 to 5. Higher scores mean the pneumonia is more severe. A score of 0 or 1 means treatment can be done at home. Scores of 2 or more might need hospital care.
|
CURB-65 Score |
Severity |
Recommended Management |
|---|---|---|
|
0-1 |
Low |
Outpatient treatment |
|
2 |
Moderate |
Consider hospitalization |
|
3-5 |
High |
Hospitalization recommended |
Determining Outpatient vs. Inpatient Treatment
Deciding if a patient should stay home or go to the hospital depends on the severity tools. Patients with low scores can usually stay home. Those with higher scores need hospital care for better monitoring and treatment.
Using these tools, healthcare providers can give each patient the right community acquired pneumonia treatment. This approach improves care and lowers the chance of serious problems.
Treatment Strategies and Antibiotic Selection
Community acquired pneumonia treatment focuses on starting antibiotics right away. We adjust them based on how the patient responds and lab results. We’ll cover the main steps in treating CAP, including picking the right antibiotics.
Empiric Antibiotic Therapy Guidelines
When treating CAP, we start with antibiotics based on likely causes and patient factors. These include age, health conditions, and how sick the patient is. We also consider local resistance patterns.
For healthy outpatients, amoxicillin or doxycycline are good choices. Patients with health issues might get amoxicillin-clavulanate or a respiratory fluoroquinolone.
Targeted Treatment Based on Pathogen Identification
After finding out the cause of pneumonia, we can fine-tune the treatment. This makes the treatment more effective and helps prevent antibiotic resistance.
The table below shows the initial antibiotic choices for CAP:
|
Patient Category |
Recommended Antibiotics |
|---|---|
|
Outpatient, previously healthy |
Amoxicillin or Doxycycline |
|
Outpatient, with comorbidities |
Amoxicillin-clavulanate or a respiratory fluoroquinolone |
|
Inpatient, non-ICU |
Beta-lactam plus a macrolide or a respiratory fluoroquinolone |
|
Inpatient, ICU |
Beta-lactam plus a macrolide or a respiratory fluoroquinolone |
Effective CAP treatment needs careful thought about the patient’s situation and lab results. By following guidelines and tailoring treatment, we can better outcomes and lower complication risks.
Complications and Prognosis of Community Acquired Pneumonia
CAP can lead to serious complications like respiratory failure and sepsis. These can change a patient’s outlook. They happen due to the infection’s severity, health issues, or late treatment.
Short-term Complications: Respiratory Failure and Sepsis
Respiratory failure and sepsis are serious short-term issues with CAP. Respiratory failure means the lungs can’t get enough oxygen. Sepsis is a dangerous body reaction to an infection. Both need quick medical help.
It’s key to spot these complications early. Look for signs like trouble breathing, fast heart rate, and confusion. Quick action can greatly help patient recovery.
Mortality Rates: 6% at 30 Days, Rising to 34% in Unresolving Cases
CAP’s death rate changes based on how severe it is and how well it responds to treatment. At 30 days, about 6% of patients die. But, this number jumps to 34% if the pneumonia doesn’t get better.
|
Time Frame |
Mortality Rate |
|---|---|
|
30 Days |
6% |
|
Unresolving Cases |
34% |
ICU Admission and 23% Mortality Rate in Severe Cases
Severe CAP cases often need ICU care. The death rate for these patients is about 23%. ICU care is for those with serious respiratory issues, septic shock, or other critical problems.
Knowing CAP’s complications and outlook is vital. It helps set patient hopes and guide treatment. By spotting risks and using the right treatments, we can better care for CAP patients.
Prevention Strategies for Community Acquired Pneumonia
We can lower CAP cases by using prevention methods. These include vaccines and lifestyle changes to cut down risks.
Vaccination Recommendations
Vaccines are key in fighting CAP. Pneumococcal and influenza vaccines are very important. The pneumococcal vaccine guards against Streptococcus pneumoniae, a common CAP cause. The influenza vaccine helps avoid flu, which can turn into pneumonia.
People at high risk, like older adults and those with chronic health issues, should get these shots. Adults 65 years and older need both pneumococcal conjugate (PCV) and pneumococcal polysaccharide (PPSV23) vaccines. Also, annual influenza vaccination is a must for all adults, but it’s even more important for those at high risk.
Lifestyle Modifications and Risk Reduction
Changing your lifestyle can also lower CAP risk. Quitting smoking is essential because smoking harms the lungs and raises infection risk. It’s also wise to stay away from indoor and outdoor air pollution, as it can irritate the lungs and make them more open to infection.
Living a healthy lifestyle is also key. This includes eating well and exercising regularly to boost your immune system. Taking care of chronic health issues, like diabetes and heart disease, is also critical, as these can up the CAP risk.
By using vaccines and making these lifestyle changes, we can cut down CAP cases and improve health outcomes.
Conclusion: Advancing Our Approach to CAP Management
Managing community acquired pneumonia (CAP) well needs a deep understanding of its causes, diagnosis, and treatment. We’ve looked into CAP’s key points, from its spread and causes to how it’s diagnosed and treated.
Knowing what CAP is helps doctors treat patients right. They can make plans based on each patient’s needs. This makes care better and cuts down on problems.
To better handle CAP, we must improve how we diagnose and treat it. We also need to focus on preventing it. Vaccines and healthy living choices help lower CAP risk. A complete plan for CAP care can make patients’ lives better.
As we learn more about CAP, keeping up with new advice is key. This ensures we give patients the best care. It also helps fight CAP worldwide, making life better for many.
FAQ
What is Community Acquired Pneumonia (CAP)?
Community Acquired Pneumonia (CAP) is pneumonia that people get outside of hospitals. It’s usually caused by bacteria, viruses, or fungi.
What are the causes of CAP?
CAP can be caused by many things, like bacteria, viruses, or fungi. The most common cause is Streptococcus pneumoniae.
How is CAP differentiated from Hospital-Acquired Pneumonia (HAP) and Healthcare-Associated Pneumonia (HCAP)?
CAP is different from HAP and HCAP because it happens outside of hospitals. HAP and HCAP occur in healthcare settings.
What is the definition of CAP disease?
CAP disease is an infection in the lungs that happens in community settings. It causes inflammation and damage to lung tissue.
What are the typical symptoms of CAP?
Symptoms of CAP include coughing, fever, chest pain, and trouble breathing. These are common signs.
How is CAP diagnosed?
Doctors diagnose CAP by looking at symptoms, doing chest X-rays, and running lab tests. These tests include blood cultures and sputum analysis.
What is the CURB-65 score used for in CAP management?
The CURB-65 score helps doctors decide how to treat CAP. It looks at age, confusion, and vital signs to guide treatment.
What are the treatment strategies for CAP?
Treatment for CAP includes starting antibiotics right away. Doctors also tailor treatment based on what caused the infection. The goal is to lower the risk of serious problems.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6778534/







