Frontotemporal dementia (FTD) is a brain disease that changes how people behave, talk, and think. It affects the frontal and temporal lobes. Knowing how long someone with FTD might live is important for patients, families, and caregivers. Learn the crucial facts about Sinus Infection and Neck Pain ExplainedFTD life expectancy for Frontotemporal Dementia. Get a clear understanding of the average longevity and outlook.
The average frontotemporal dementia life expectancy is between 7 to 13 years after symptoms start. But, how long someone lives can really vary. This depends on the type of FTD and other health factors.
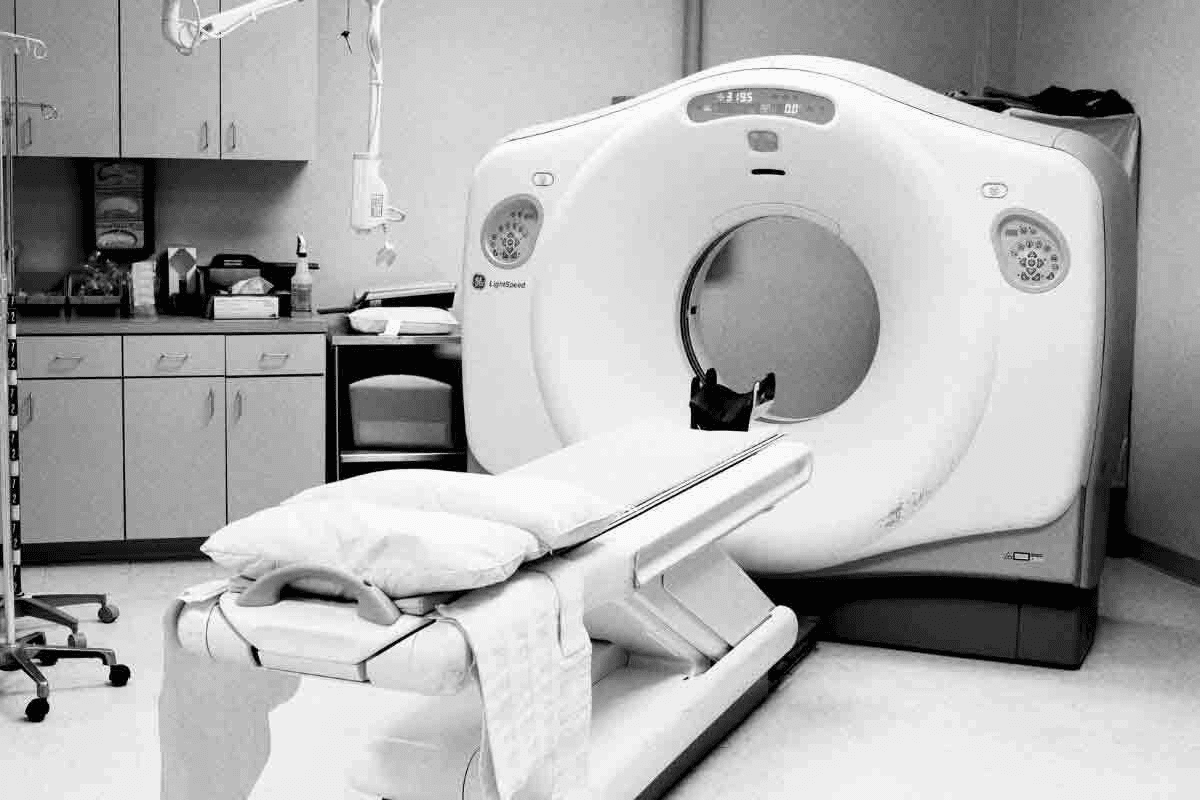
At Liv Hospital, we offer top-notch care for FTD patients and their families. We have the latest diagnostic tools and treatments that work.
Key Takeaways
- FTD is a progressive neurodegenerative disorder affecting behavior, language, and cognitive function.
- Average life expectancy after symptom onset ranges from 7 to 13 years.
- Individual outcomes vary significantly based on disease type and clinical features.
- Liv Hospital provides comprehensive care for FTD patients and their families.
- Advanced diagnostic capabilities and evidence-based treatments are available.
Understanding Frontotemporal Dementia

It’s important to understand frontotemporal dementia for both patients and doctors. Frontotemporal dementia (FTD) is a brain disorder that affects the frontal and temporal lobes. This leads to changes in behavior, language, and thinking.
What Is Frontotemporal Dementia?
FTD is a rare brain disorder that affects people in their 40s to 65. It causes different symptoms in each person. FTD is a rare condition that often strikes people in the prime of life, typically between the ages of 40 and 65.
The symptoms of FTD can be broadly categorized into three main types: behavioral changes, language difficulties, and motor symptoms. Some of the common symptoms include:
- Significant changes in personality and behavior
- Difficulty with language, including speaking, reading, and writing
- Motor symptoms, such as weakness or paralysis
- Problems with executive function, such as planning and decision-making
How FTD Differs From Other Dementias
FTD is different from other dementias, like Alzheimer’s disease. Alzheimer’s mainly affects memory, while FTD impacts behavior, language, and motor skills early on.
Some of the distinguishing features of FTD include:
- Early onset: FTD often occurs at a younger age than Alzheimer’s disease.
- Behavioral changes: FTD can cause significant changes in personality and behavior.
- Language difficulties: FTD can affect an individual’s ability to communicate effectively.
Brain Regions Affected
The frontal and temporal lobes are mainly affected by FTD. The frontal lobe handles executive functions like decision-making. The temporal lobe is key for language processing.
Damage to these areas leads to FTD symptoms. These include changes in behavior, language issues, and cognitive problems.
FTD Life Expectancy: General Statistics
Frontotemporal Dementia (FTD) life expectancy varies a lot among people. It’s key to look at general stats. FTD has many subtypes, each affecting life expectancy differently. Knowing these stats helps families plan for the future.
Average Survival Rates
Studies say FTD patients live 7 to 13 years after diagnosis. The median survival is about 8 years from symptom start. But, this can change a lot based on the FTD subtype and other factors.
A study in Neurology found bvFTD patients live about 9.4 years after symptoms start. Remember, these numbers are averages and not predictions for everyone.
“The variability in survival rates among FTD patients shows how complex this condition is. It highlights the need for care tailored to each person.”
Measuring From Symptom Onset vs. Diagnosis
It’s important to know the difference between measuring from symptom start and diagnosis. Symptom onset is when symptoms first appear. Diagnosis is when a doctor confirms FTD.
It can take 3 to 6 years to get a diagnosis after symptoms start. This delay can change how we see survival time. So, studies report survival from both symptom onset and diagnosis.
|
Measurement Point |
Median Survival Time |
Range |
|---|---|---|
|
From Symptom Onset |
8-10 years |
5-15 years |
|
From Diagnosis |
3-6 years |
2-10 years |
Individual Variation in Prognosis
Every person with FTD is different. Age at onset, genetic mutations, and other health issues can affect life expectancy. For example, some genetic mutations can change survival rates.
Younger onset often means faster disease progress. But, this isn’t always true. The big difference in prognosis shows why care plans need to change often.
Understanding these factors helps doctors give better, more personal predictions to patients and their families.
Life Expectancy by FTD Subtypes
Knowing the different types of frontotemporal dementia (FTD) helps predict life expectancy and plan care. FTD is a complex disorder with several subtypes, each with its own traits and life spans.
Behavioral Variant FTD (bvFTD)
Behavioral variant FTD is the most common type. It’s marked by big changes in personality and behavior. Studies show that people with bvFTD usually live about 9 years after symptoms start.
Early diagnosis and managing behavioral symptoms are key to improving life quality for these patients.
“The median survival time for bvFTD is approximately 9 years from symptom onset, highlighting the need for timely and effective care strategies.”
FTD With Motor Neuron Disease (FTD-ALS/FTD-MND)
FTD with motor neuron disease is very aggressive. It combines FTD’s cognitive and behavioral changes with ALS’s motor symptoms. Research shows that FTD-ALS has a much shorter survival time, usually 2 to 3 years after symptoms start.
|
FTD Subtype |
Median Survival Time |
|---|---|
|
bvFTD |
9 years |
|
FTD-ALS/FTD-MND |
2-3 years |
|
Semantic Dementia |
8-10 years |
|
Progressive Non-Fluent Aphasia |
6-12 years |
Semantic Dementia
Semantic dementia is known for losing semantic information. This makes it hard to understand word meanings and recognize objects. Studies suggest a median survival time of 8 to 10 years after symptoms start.
Progressive Non-Fluent Aphasia
Progressive non-fluent aphasia is characterized by a decline in language skills, mainly in speaking. The prognosis varies, with survival times ranging from 6 to 12 years after symptoms begin.
Knowing the life expectancy for each FTD subtype is vital for providing specific care and support. By understanding each subtype’s unique characteristics and life spans, healthcare providers can better meet patients’ needs.
Factors Affecting FTD Prognosis
Understanding what affects FTD prognosis is key to managing the condition well. Several factors play a big role in how fast the disease progresses and how long someone lives with it.
Age at Onset
The age when FTD symptoms start can greatly affect the prognosis. Early onset often means a faster disease progression. Research shows that those who get FTD young can live with it for over 10 years.
On the other hand, those who get it later might have a shorter time with the disease. Knowing this helps doctors give better predictions to patients and their families.
Genetic Factors
Genetic mutations are very important in FTD prognosis. Mutations in genes like GRN, C9ORF72, and MAPT are linked to FTD. These mutations can change when symptoms start, how fast the disease gets worse, and how long someone lives.
For example, people with C9ORF72 expansions might have a different disease course. Genetic tests can help predict how the disease will progress and help with family planning.
Comorbid Conditions
Having other health issues can greatly affect FTD prognosis. Conditions like heart disease, diabetes, or other brain diseases can make managing FTD harder and might shorten life expectancy.
|
Comorbid Condition |
Impact on FTD Prognosis |
|---|---|
|
Cardiovascular Disease |
Increases risk of mortality and complicates management |
|
Diabetes |
Can affect overall health and disease progression |
|
Other Neurological Conditions |
May accelerate cognitive decline and complicate care |
Access to Specialized Care
Getting specialized care and support is essential for managing FTD well. Teams with neurologists, psychologists, speech therapists, and social workers can offer care that fits each person’s needs.
Early care and ongoing support can greatly improve life quality for those with FTD and their families. Being part of clinical trials and new treatments also gives hope for changing the disease’s course.
Early Signs and Disease Progression
It’s key to spot the first signs of Frontotemporal Dementia (FTD) for both patients and their caregivers. FTD shows different symptoms in different people, making it hard to diagnose early. We’ll look at the early signs, how fast the disease can progress, and how it varies from person to person.
Initial Symptoms and Recognition
FTD starts slowly, with symptoms that can sneak up on you. Early signs include changes in behavior, trouble with language, or motor issues. These can be mistaken for other problems or stress, which can delay getting a diagnosis. It’s vital for families and doctors to know these signs to act quickly.
How Fast Does FTD Progress?
How fast FTD gets worse can vary a lot. Some people live over 10 years after being diagnosed, while others decline faster. The speed of progression depends on the type of FTD, when it starts, and genetics. Knowing these can help plan care and set realistic expectations.
Variability in Progression Rates
FTD doesn’t progress the same for everyone. Some may get worse slowly over years, while others decline quickly. Things like other health issues and access to care can also affect how fast it gets worse. Understanding these factors is key to giving the right support and care.
We stress the need for care plans that fit each person’s unique situation with FTD. This approach can enhance the lives of both patients and their caregivers.
Stages of Frontotemporal Dementia
Frontotemporal dementia (FTD) goes through different stages. Each stage has its own signs and challenges. Knowing these stages helps in giving the right care and support.
Early Stage Manifestations
In the early stages, people might show small changes in how they act, talk, or think. These changes can happen slowly and might not be easy to see at first. Some common signs include:
- Apathy or pulling away from social activities
- Changes in what they eat or like to eat
- Not taking care of their personal hygiene or grooming
- Having trouble finding the right words
It’s important for family and caregivers to notice these changes. If they see a big drop in how someone functions, they should get medical help.
Middle Stage Challenges
When FTD moves to the middle stage, symptoms get worse. This makes life harder for the person and those caring for them. Signs of this stage include:
- More acting out or being aggressive
- Big trouble with talking, making it hard to communicate
- Motor problems, like weakness or trouble moving
- Needing more help with everyday tasks
Caregivers need to change how they care for the person. They might need to help with daily tasks and manage behavior problems.
Advanced Stage Symptoms
In the advanced stages, people lose a lot of their thinking and doing skills. Symptoms include:
- Severe trouble with talking, maybe not being able to speak at all
- Big motor problems, which can make it hard to move
- Trouble eating or swallowing
- Higher risk of getting sick or having other health problems
Care at this stage focuses on making the person comfortable. It’s about managing symptoms and keeping their dignity and quality of life.
End-Stage FTD Characteristics
In the last stages, people need full-time care for everything. Signs of end-stage FTD include:
- Nearly no ability to talk
- Big motor problems, often making them unable to move
- Higher risk of getting sick or having serious health issues
- Need for constant care and support
At this point, care shifts to making the person comfortable. It’s about managing pain and supporting the person and their family through the end-of-life process.
Comparing FTD Life Expectancy to Other Dementias
Learning about Frontotemporal Dementia (FTD) life expectancy compared to other dementias is key. It helps patients, caregivers, and doctors make better care plans. This knowledge is vital for everyone involved in a person’s care.
FTD vs. Alzheimer’s Disease
FTD usually starts in people in their 50s or 60s. It often lasts 6 to 12 years after symptoms start, which is shorter than Alzheimer’s. Alzheimer’s patients can live 8 to 12 years or more after being diagnosed. FTD tends to progress faster than Alzheimer’s.
FTD vs. Vascular Dementia
Vascular dementia is the second most common dementia after Alzheimer’s. It’s life expectancy can be shorter than FTD, mainly because of heart risks. But, how long someone lives with vascular dementia can really vary. It depends on how much and where the brain is damaged.
FTD vs. Lewy Body Dementia
Lewy body dementia is marked by abnormal brain proteins. People with Lewy body dementia usually live 5 to 7 years after diagnosis. FTD patients might live a bit longer, but both conditions can be unpredictable in how long they last.
Looking at FTD alongside other dementias shows the need for tailored care. Knowing these differences helps in setting realistic goals and planning for the future.
Medical Management and Its Impact on Survival
FTD treatment involves many steps to help manage symptoms and slow the disease. There’s no cure for Frontotemporal Dementia (FTD) yet. But, different treatments and strategies can greatly improve life quality for those affected.
Current Treatment Approaches
Today’s FTD treatment combines medicines and non-medical methods. Medicines help with symptoms like behavior changes, speech issues, and motor problems.
Pharmacological Interventions: SSRIs might be used to control behavior. Other drugs can help with agitation or aggression.
Symptom Management Strategies
Managing symptoms is key to better life quality for FTD patients. Strategies include:
- Behavioral therapy for behavior changes
- Speech therapy for communication issues
- Physical therapy for mobility and strength
- Occupational therapy for daily activities
Emerging Therapies and Clinical Trials
Research into FTD is active, with new therapies and trials showing hope. These include:
|
Therapy Type |
Description |
Potential Benefit |
|---|---|---|
|
Gene Therapy |
Aims to tackle FTD’s genetic causes |
Could slow or stop disease growth |
|
Immunotherapy |
Targets proteins linked to FTD |
May lessen symptom severity |
|
Stem Cell Therapy |
Looks into stem cells repairing brain damage |
Could bring back lost functions |
Living With FTD: Practical Considerations
Living with Frontotemporal Dementia (FTD) means making big changes. Patients and caregivers need to adjust as the disease gets worse. This includes changing how we care for and support each other.
Adapting the Home Environment
Making the home safe and supportive is key for FTD patients. This might mean removing things that could cause falls, putting in safety locks, and making the home simpler. This helps reduce confusion.
It’s important to check the home for dangers and make changes to avoid accidents. For example, putting labels on rooms and using signs can help patients find their way around.
Managing Behavioral Changes
FTD can cause big changes in behavior, like feeling less interested in things or acting in ways that are not usual. Dealing with these changes takes patience, understanding, and sometimes, help from experts.
Caregivers can learn ways to handle tough behaviors. This might include setting clear routines, using positive feedback, or finding ways to distract them.
Communication Strategies
Talking effectively is very important when caring for someone with FTD. As the disease gets worse, patients may have trouble with words. So, we need to find new ways to communicate.
Using simple, clear language and gestures or pictures can help. It’s also important to be patient and let the patient take their time to answer.
Legal and Financial Planning
Getting a diagnosis of FTD means thinking about legal and financial matters. It’s important to plan early to make sure the patient’s wishes are followed and their affairs are in order.
This planning might include setting up power of attorney, making a living will, and planning for long-term care. Getting advice from experts in law and finance who know about dementia is very helpful.
Caregiving and Support Systems
Frontotemporal Dementia caregiving needs a full plan, including medical care, emotional support, and practical help. Caregivers are key in managing the disease and improving life for those with FTD.
Challenges Faced by Caregivers
Caregivers of FTD patients face big challenges. They must handle behavioral changes, provide physical care, and deal with emotional stress. The caregiver burden can really affect their health.
We know caregivers need help and resources. They need education on FTD, ways to manage behavior, and access to professional care.
Professional Care Options
Professional care is key for supporting caregivers and FTD patients. Services like home care, adult day care, and residential care offer many benefits. They give caregivers a break and provide specialized care for FTD patients.
We stress the need for these services. They help caregivers by taking some of the load off, so they can take care of themselves.
Support Groups and Resources
Support groups and resources are vital for caregivers. They offer a place to share, get emotional support, and get practical advice. These groups can be in-person or online, fitting different schedules and needs.
We encourage caregivers to use these resources. They can make caregiving better. Support groups and online forums connect caregivers with others who get FTD caregiving.
The Importance of Respite Care
Respite care is a must for FTD caregiving. It gives caregivers a break, whether it’s in-home care, adult day care, or short stays in facilities. Respite care helps caregivers rest and recharge, preventing burnout.
We say respite care is essential, not a luxury. It helps caregivers stay healthy and keep providing quality care for their loved ones.
End-of-Life Care for FTD Patients
End-of-life care for Frontotemporal Dementia patients needs a mix of medical and emotional support. As the disease gets worse, patients and their families face big challenges. They need care that is both kind and all-encompassing.
Palliative Care Approaches
Palliative care is key in managing FTD symptoms, making life better for patients. We work to reduce pain, manage behavior, and offer emotional support. Palliative care teams work closely with patients and their families to create care plans that fit their needs and wishes.
Hospice Considerations
Hospice care is vital for many FTD patients nearing the end of life. Hospice focuses on comfort and quality of life, not on curing the disease. Hospice teams are trained to manage complex symptoms and offer emotional and spiritual support to patients and their families.
Comfort Measures and Dignity
Keeping patients comfortable and dignified is essential in the final stages of FTD. This means managing pain well, ensuring they eat and drink enough, and helping with daily tasks. We also make sure to respect patient autonomy and include their wishes in care plans when we can.
Supporting Family Through the Final Stages
Supporting FTD patients’ families is a big part of end-of-life care. We offer resources and counseling to help them deal with their emotions. Open communication and emotional support are key in helping families get through this tough time.
By taking a caring and all-encompassing approach to end-of-life care, we can greatly improve the lives of FTD patients and their families.
Conclusion
Understanding Frontotemporal Dementia (FTD) is key to helping patients and their families. FTD is a complex condition that needs a lot of care and support. We’ve looked at what FTD is, how long people live with it, its different types, and what affects its outcome.
Knowing how complex FTD is helps us meet its needs better. We’ve talked about how early diagnosis, medical care, and support for caregivers can improve life for those with FTD.
In short, FTD is a complex disorder that needs a full care approach. By summarizing the main points and stressing the need to understand FTD, we can offer better care and support. This helps improve the lives of those affected. This wraps up our look at FTD, laying a foundation for more study and understanding of this complex condition.
FAQ
What is the average life expectancy for someone diagnosed with Frontotemporal Dementia (FTD)?
People with FTD usually live between 6 to 12 years after symptoms start. This time can change a lot based on the type of FTD and other factors.
How does the life expectancy of FTD compare to other forms of dementia?
FTD often starts earlier and can last shorter than Alzheimer’s. But, it can last longer than some other types like FTD-ALS. Life expectancy varies a lot among different dementia types.
What factors influence the life expectancy of someone with FTD?
Several things can affect how long someone with FTD lives. These include when symptoms start, the type of FTD, other health issues, genes, and the care they get.
Does the rate of FTD progression vary among individuals?
Yes, how fast FTD gets worse can differ a lot. Some people may decline quickly, while others may get worse more slowly.
What are the different subtypes of FTD and how do they affect life expectancy?
FTD has several types, like bvFTD, FTD-ALS, semantic dementia, and progressive non-fluent aphasia. FTD-ALS usually means a shorter life because of the linked motor neuron disease.
How does age at onset impact FTD prognosis?
When symptoms start can affect how long someone with FTD lives. Starting earlier often means a longer illness, while starting later might mean a quicker decline.
Are there any genetic factors that influence FTD life expectancy?
Yes, genes are very important in FTD. Certain genetic changes can affect when symptoms start and how fast the disease gets worse.
What are the early signs of FTD and how is it diagnosed?
Early signs of FTD include changes in behavior, trouble with language, and motor issues. Doctors diagnose it by looking at symptoms, imaging, and sometimes genetic tests.
How can caregivers support individuals with FTD?
Caregivers can help by making the home safe, managing behavior changes, using good communication, and getting help from professionals and support groups.
What are the options for end-of-life care for FTD patients?
For FTD patients nearing the end, options include palliative care, hospice, comfort measures, and support for the family during this time.
Can current treatments or therapies impact the life expectancy of someone with FTD?
There’s no cure for FTD, but treatments can help manage symptoms and slow the disease. This can improve quality of life and possibly life expectancy.
What is the role of clinical trials in FTD management?
Clinical trials are key in FTD management. They test new treatments and therapies that could slow disease progression and improve life expectancy.
How does FTD life expectancy compare to that of Alzheimer’s disease?
FTD usually starts younger and has a variable life expectancy compared to Alzheimer’s. Alzheimer’s often starts later and has a more predictable course.
References
National Center for Biotechnology Information. Frontotemporal Dementia: Life Expectancy After Diagnosis. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC3953732/