At Liv Hospital, we aim to provide top-notch medical care for complex conditions like Alzheimer’s. Alzheimer’s is a complex disorder with specific signs.
Amyloid plaques and neurofibrillary tangles are key in the disease’s growth. Amyloid plaques are clumps of amyloid-beta peptides between nerve cells. Neurofibrillary tangles are twisted filaments of tau protein inside neurons.
Knowing about these features helps us find better treatments. We use the newest medical innovations to help our patients.
Key Takeaways
- Alzheimer’s disease is marked by amyloid plaques and neurofibrillary tangles.
- Amyloid plaques are clumps of amyloid-beta peptides outside nerve cells.
- Neurofibrillary tangles are twisted tau protein inside neurons.
- Understanding these signs is key for diagnosis and treatment.
- Liv Hospital is dedicated to top care for Alzheimer’s patients.
The Pathological Hallmarks of Alzheimer’s Disease
Understanding Alzheimer’s disease is key to diagnosing and managing it. This neurodegenerative disorder has distinct features.
Understanding Alzheimer’s Disease
Alzheimer’s disease is known for amyloid plaques and neurofibrillary tangles in the brain. These features cause loss of connections between brain cells. Medical Expert, “These plaques and tangles are key signs of the disease. Knowing about them is vital for finding treatments.”
“The presence of amyloid plaques and neurofibrillary tangles is a defining feature of Alzheimer’s disease, and research into these pathological hallmarks has significantly advanced our understanding of the condition.”
Key Biological Markers
Important biological markers like amyloid-beta peptides and tau protein help diagnose Alzheimer’s. They are linked to the formation of amyloid plaques and neurofibrillary tangles. Studies have found:
- Amyloid-beta peptides are involved in the formation of amyloid plaques.
- Tau protein is a primary component of neurofibrillary tangles.
- Biological markers can help identify individuals at risk of developing Alzheimer’s disease.
By understanding these hallmarks and markers, we can better diagnose and manage Alzheimer’s. This helps improve patient care.
Amyloid Plaques and Neurofibrillary Tangles: Definition and Structure
To understand Alzheimer’s disease, we must look at amyloid plaques and neurofibrillary tangles. These are key signs of the disease and help it grow.
Composition of Amyloid Plaques
Amyloid plaques are mainly made of amyloid-beta peptides. These come from the amyloid precursor protein (APP). APP is a big protein in the neuron’s membrane. The buildup of amyloid-beta outside neurons is a key sign of Alzheimer’s. The makeup of amyloid plaques is complex, with amyloid-beta, other proteins, and parts of cells.
Structure of Neurofibrillary Tangles
Neurofibrillary tangles are made of tau protein that’s been changed by too much phosphate. Normally, tau helps keep microtubules in neurons strong. But in Alzheimer’s, tau changes and forms insoluble fibrils. This changed tau protein messes up neurons and leads to their death.
The tangles are made of paired helical filaments of tau protein. These tangles build up inside neurons, messing up their work.
Historical Discovery by Medical Expert
The history of Alzheimer’s disease started with Medical Expert’s detailed study in 1906. This discovery is key to understanding Alzheimer’s today.
Medical Expert. His work at the Royal Psychiatric Hospital in Munich, Germany, helped us understand many brain disorders.
The First Documented Case
In 1906, Medical Expert 51-year-old woman named Auguste Deter. She had memory loss, language issues, and odd behavior. Medical Expert.
Auguste Deter’s case was the first known Alzheimer’s disease. It showed how complex the disease is. Medical Expert’s work changed how we study brain diseases.
Evolution of Scientific Understanding
Our knowledge of Alzheimer’s has grown a lot over time. New technology and research methods have helped us learn more. Finding amyloid precursor protein (APP) and its role in amyloid plaques was a big step.
Today, we remember Medical Expert’s groundbreaking work. His commitment to brain research has shaped neurology forever.
Formation and Development of Amyloid Plaques
Understanding how amyloid plaques form is key to understanding Alzheimer’s disease. These plaques are a major sign of the disease. Their development is a complex series of molecular events.
Amyloid Precursor Protein (APP) Processing
The journey of amyloid plaque formation starts with APP, a brain protein. APP is cut by enzymes called secretases. This creates beta-amyloid peptides, which can stick together.
APP processing is a critical step. The beta-amyloid peptides that result are sticky. They form insoluble fibrils that deposit outside of cells.
Beta-Amyloid Aggregation
Beta-amyloid peptides stick together, forming plaques. Their hydrophobic nature makes them aggregate. This process is influenced by peptide length, metal ions, and the brain’s environment.
Research shows that beta-amyloid aggregation harms neurons. It disrupts synaptic function and leads to neuron loss. The exact ways it causes harm are being studied.
Extracellular Deposition Patterns
Amyloid plaques mainly deposit in the brain’s gray matter. This includes areas like the neocortex and hippocampus. Plaques can deposit differently in each person, but often start in the neocortex and spread.
The deposition of plaques is linked to inflammation and gliosis. This further worsens Alzheimer’s disease. Knowing how plaques deposit is key for diagnosis and treatment.
|
Process |
Description |
Key Factors Involved |
|---|---|---|
|
APP Processing |
Cleavage of APP by secretases |
Beta-secretase, gamma-secretase |
|
Beta-Amyloid Aggregation |
Aggregation of beta-amyloid peptides |
Peptide length, metal ions, local environment |
|
Extracellular Deposition |
Deposition of amyloid plaques in brain tissue |
Gray matter, neocortex, hippocampus |
Tau Protein and Neurofibrillary Tangle Development
Understanding tau protein and neurofibrillary tangles is key to Alzheimer’s disease. Neurofibrillary tangles are a major sign of Alzheimer’s. They form because of tau protein dysfunction.
Normal Tau Function in Healthy Neurons
Tau protein helps keep neurons stable. It binds to microtubules, aiding in axonal transport and keeping neurons in shape. The normal function of tau is critical for neuronal health and function.
Tau protein is involved in many cellular processes. These include:
- Regulation of microtubule dynamics
- Axonal transport
- Maintenance of neuronal shape
Hyperphosphorylation Process
Hyperphosphorylation of tau protein is a major step in neurofibrillary tangle formation. When tau is hyperphosphorylated, it detaches from microtubules and aggregates. This process is believed to be triggered by various factors, including abnormal kinase activity. Hyperphosphorylation of tau leads to neurofibrillary tangle formation.
|
Kinase |
Role in Tau Hyperphosphorylation |
|---|---|
|
CDK5 |
Phosphorylates tau at multiple sites |
|
GSK3β |
Primarily responsible for tau hyperphosphorylation |
Intracellular Aggregation Mechanisms
The aggregation of hyperphosphorylated tau is complex. It forms insoluble fibrils that accumulate in neurons, leading to neurofibrillary tangles. The aggregation process is influenced by factors such as tau isoform composition and post-translational modifications.
“The aggregation of tau protein is a critical step in the development of neurofibrillary tangles, and understanding this process is essential for the development of therapeutic strategies targeting tau pathology.”
— Medical Expert, Alzheimer’s Researcher
Recent studies highlight the importance of tau protein dynamics in Alzheimer’s disease. By understanding tau dysfunction and neurofibrillary tangle formation, researchers can develop targeted therapies. This can help slow Alzheimer’s progression.
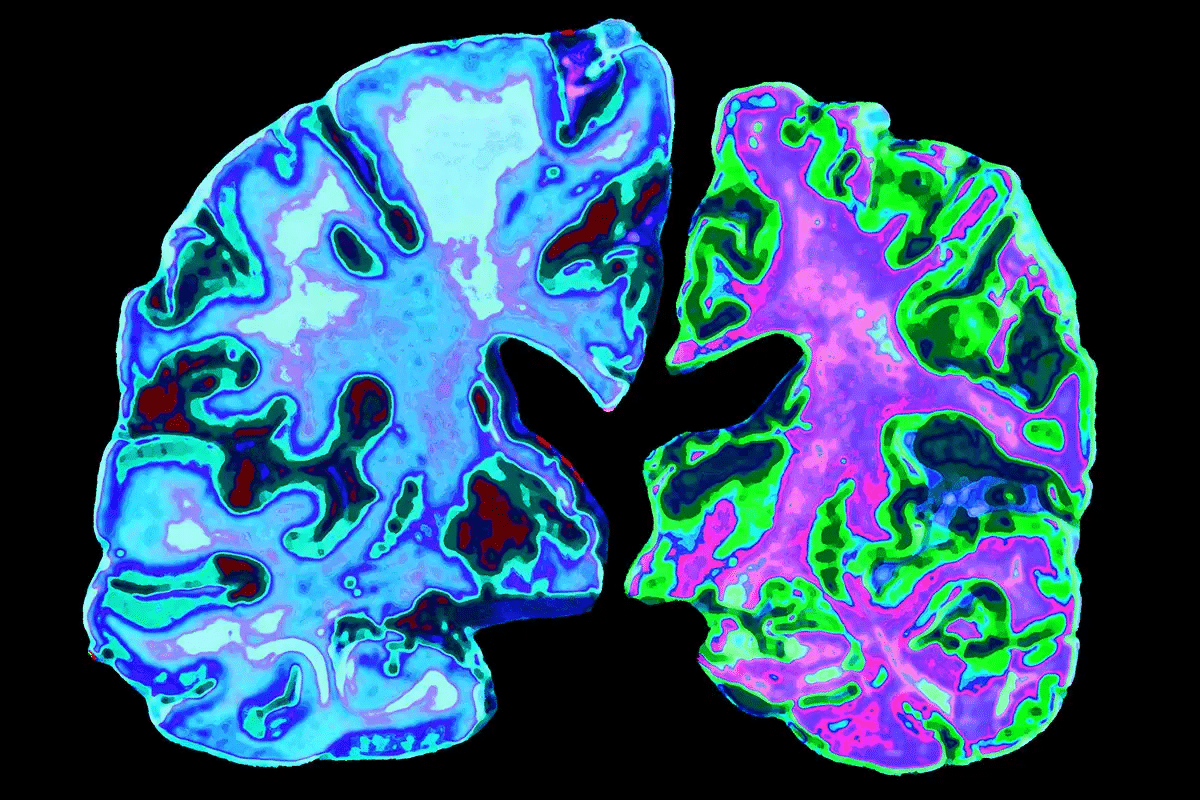
Anatomical Distribution in the Brain
Amyloid plaques and neurofibrillary tangles have a specific pattern in the brain. This pattern is key to understanding Alzheimer’s disease. They mainly affect the neocortex and hippocampus, leading to cognitive decline.
Affected Brain Regions
The neocortex is hit hard by amyloid plaques. It’s key for processing sensory info, controlling movement, and thought. The hippocampus, important for memory, is also damaged by neurofibrillary tangles.
Other areas like the entorhinal cortex and amygdala are also affected. This adds to the complex symptoms of Alzheimer’s disease.
Progression Patterns
The growth of amyloid plaques and neurofibrillary tangles follows a pattern. They first show up in the hippocampus and entorhinal cortex. These areas are vital for memory.
As the disease gets worse, plaques and tangles spread to other parts of the brain. This includes the neocortex, causing widespread damage to neurons.
Impact on Neocortex and Hippocampus
The neocortex and hippocampus are very sensitive to these changes. The buildup of plaques and tangles in these areas harms normal brain function. This leads to memory loss and cognitive decline.
Understanding how these areas are affected is vital. It helps in finding effective treatments for Alzheimer’s disease.
Relationship Between Plaques, Tangles, and Cognitive Decline
Amyloid plaques and neurofibrillary tangles are linked to how severe cognitive symptoms are in Alzheimer’s patients. Understanding how these work is key to finding better ways to diagnose and treat the disease.
Correlation with Symptom Severity
Studies show that amyloid plaques and neurofibrillary tangles are tied to how much cognitive decline there is in Alzheimer’s. The more of these there are, the worse the symptoms, like memory loss and thinking problems.
A study found that those with more tangles in certain brain areas had worse thinking skills. This shows how important these features are in Alzheimer’s getting worse.
Neuronal Loss and Synaptic Dysfunction
Amyloid plaques and neurofibrillary tangles cause neuronal loss and synaptic dysfunction. These are big reasons why thinking gets worse in Alzheimer’s. They mess up how neurons work and lead to brain circuit damage.
Synaptic problems start early in the disease. They make it hard for neurons to talk to each other, leading to thinking problems.
Biomarkers and Disease Progression
Finding good biomarkers for Alzheimer’s is key. Biomarkers like amyloid-beta and tau protein in the brain fluid match up with how bad the disease is. They help doctors diagnose early and see how the disease is moving.
These biomarkers help doctors see if treatments are working. They help make better choices for patient care.
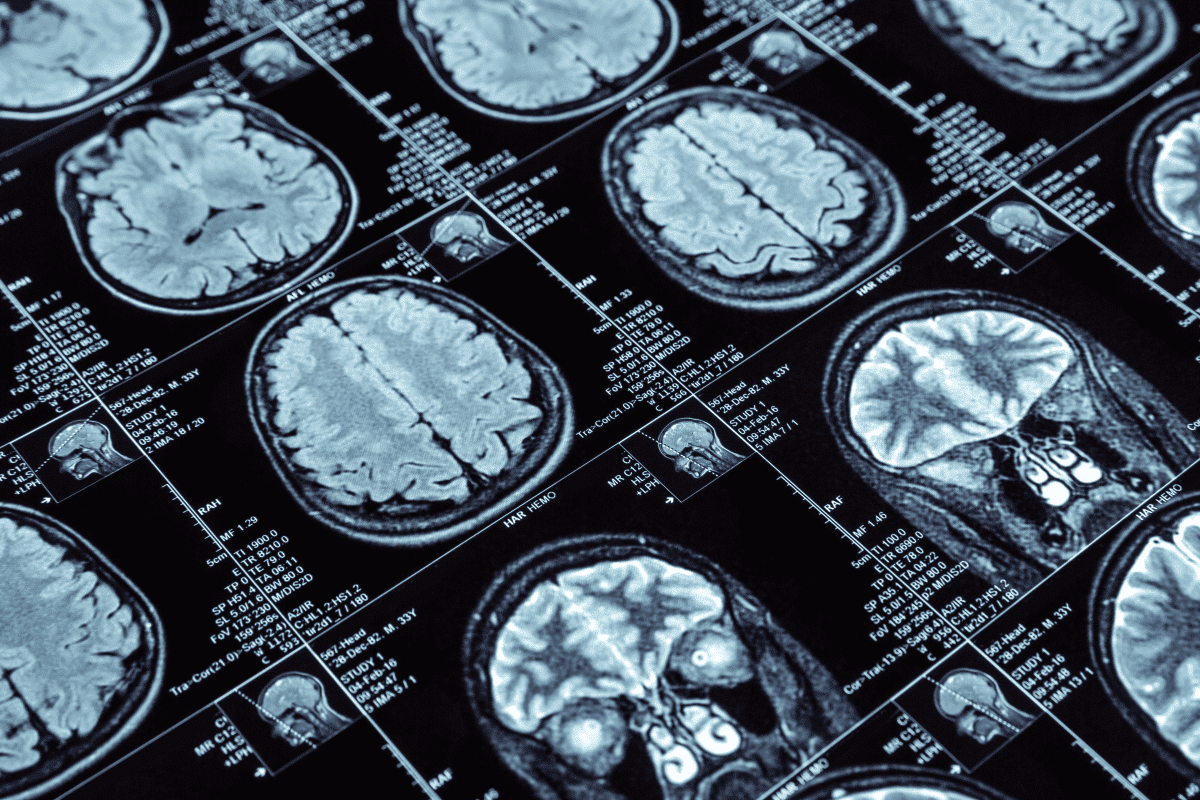
Current Diagnostic and Treatment Approaches
Medical technology has greatly improved how we diagnose and treat Alzheimer’s disease. Research is uncovering the condition’s complexities. This leads to better diagnostic tools and treatments.
Imaging Techniques for Detection
Imaging is key in diagnosing Alzheimer’s. Positron Emission Tomography (PET) scans and Magnetic Resonance Imaging (MRI) are used often. PET scans spot amyloid plaques and tau tangles. MRI shows brain structure and atrophy.
A study in the Journal of Alzheimer’s Disease found PET imaging improves diagnosis. It helps track disease progression.
“PET imaging has emerged as a valuable tool in the diagnosis and monitoring of Alzheimer’s disease, providing insights into the underlying pathology.”
Nature Reviews Neurology
Biomarker Testing
Biomarker testing is vital for diagnosing Alzheimer’s. Biomarkers like beta-amyloid and tau protein in cerebrospinal fluid (CSF) show Alzheimer’s signs. Blood biomarkers are being explored as a less invasive option.
|
Biomarker |
Description |
Clinical Significance |
|---|---|---|
|
Aβ42 |
Beta-amyloid 42 levels in CSF |
Low levels indicate amyloid plaque formation |
|
Total Tau |
Total tau protein levels in CSF |
High levels indicate neuronal damage |
|
p-Tau |
Phosphorylated tau protein levels in CSF |
High levels associated with neurofibrillary tangles |
Therapeutic Strategies Targeting Plaques and Tangles
Therapies aim to tackle amyloid plaques and neurofibrillary tangles. Amyloid-targeting therapies, like monoclonal antibodies, aim to lower plaque levels. Other methods prevent tau tangles.
Research is showing promise, with many clinical trials ongoing. We hope these new treatments will help patients with Alzheimer’s.
Conclusion
Alzheimer’s disease is marked by amyloid plaques and neurofibrillary tangles in the brain. These signs are key to understanding how the disease progresses and affects thinking.
The formation of these plaques and tangles is complex. It involves beta-amyloid peptides and tau protein. Studies show they lead to brain cell loss and problems with connections between cells. This is why people with Alzheimer’s struggle with memory and thinking.
Knowing how amyloid plaques and neurofibrillary tangles work in Alzheimer’s helps us see why we need more research. New treatments that target these problems are being developed. They offer hope for better care in the future.
As we continue, we must deepen our knowledge of Alzheimer’s. We need to find new ways to fight this disease. This will help improve the lives of those living with it.
FAQ
What are amyloid plaques and neurofibrillary tangles in Alzheimer’s disease?
Amyloid plaques are deposits of beta-amyloid protein outside neurons. Neurofibrillary tangles are twisted tau protein fibers inside neurons. Both harm neurons and lead to memory loss.
How are amyloid plaques formed?
Amyloid plaques form from amyloid precursor protein (APP) breakdown. This creates beta-amyloid peptides that clump outside neurons.
What is the role of tau protein in neurofibrillary tangle development?
Tau protein, when hyperphosphorylated, forms neurofibrillary tangles inside neurons. This is a hallmark of Alzheimer’s disease.
Which brain regions are affected by amyloid plaques and neurofibrillary tangles?
The neocortex and hippocampus are mainly affected. This leads to memory loss and cognitive decline.
How do amyloid plaques and neurofibrillary tangles relate to cognitive decline?
Their buildup causes neuronal loss and synaptic dysfunction. This results in cognitive decline, with symptoms worsening as plaques and tangles increase.
What are the current diagnostic approaches for Alzheimer’s disease?
Diagnoses use PET scans, biomarker tests, and clinical evaluations. These methods detect amyloid plaques and neurofibrillary tangles.
What are the therapeutic strategies targeting amyloid plaques and neurofibrillary tangles?
Strategies include treatments for beta-amyloid and tau protein. They also aim to manage cognitive decline symptoms.
Can Alzheimer’s disease be diagnosed with certainty before autopsy?
High probability diagnosis is possible with clinical evaluation, imaging, and biomarkers. Autopsy is needed for absolute certainty.
Are there any effective treatments for Alzheimer’s disease?
No cure exists, but treatments aim to manage symptoms. Research continues to find new strategies.
How do biomarkers contribute to the diagnosis and monitoring of Alzheimer’s disease?
Biomarkers like beta-amyloid and tau protein levels help diagnose and monitor the disease. They offer insights into progression and treatment response.
Reference
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK499922/










