Osteogenesis imperfecta, also known as brittle bone disease, is a genetic disorder. It affects the production of type I collagen. This leads to bones that break easily.
About one in 15,000 to 20,000 people have this condition. It makes bones fracture easily because of genetic defects in type I collagen.
At Liv Hospital, we know how important care is for those with osteogenesis imperfecta. Our team offers top-notch care and compassion. We help manage this tough condition for life.
Key Takeaways
- Osteogenesis imperfecta is a genetic disorder affecting type I collagen production.
- The condition causes fragile bones prone to easy fractures.
- Approximately one in 15,000 to 20,000 people are affected worldwide.
- Comprehensive management is key to improving quality of life.
- Liv Hospital provides specialized care for those with brittle bone disease.
Understanding Osteogenesis Imperfecta: An Overview
 sl
sl
Osteogenesis imperfecta is a genetic disorder that affects bone production. It makes bones very fragile and prone to breaking. We will look into what it is, how common it is, and its other names to understand it better.
Definition and Prevalence of Brittle Bones Disease
Osteogenesis imperfecta, or brittle bone disease, affects how bones are made. It happens when bones don’t get the right protein, leading to weakness. It’s found in about 1 in 15,000 to 1 in 20,000 babies worldwide. It affects both boys and girls and can cause a variety of symptoms.
Alternative Names: Vrolik Syndrome, Lobstein Syndrome, and Glass Bone Disease
Osteogenesis imperfecta is also called Vrolik syndrome and Lobstein syndrome. It’s also known as glass bone disease because bones are so fragile. Knowing these names helps doctors diagnose and treat it.
Dealing with osteogenesis imperfecta is complex. By knowing its causes, symptoms, and names, we can help those affected.
What Causes Brittle Bones Disease?

Genetic mutations are key in causing brittle bones disease. They affect the body’s ability to make healthy collagen. This disease, also known as Osteogenesis Imperfecta (OI), mainly comes from defects in genes that make type I collagen.
Genetic Mutations in COL1A1 and COL1A2 Genes
The main cause of OI is mutations in the COL1A1 and COL1A2 genes. These genes tell the body how to make the chains of type I collagen. This protein is vital for strong bones. When these genes mutate, the collagen made is weak, leading to brittle bones.
Studies show that about 80-90% of OI cases are due to COL1A1 and COL1A2 mutations. The severity of the disease varies based on the mutation’s impact on collagen.
Additional Genetic Factors: CRTAP and P3H1 Mutations
While COL1A1 and COL1A2 mutations are the main causes, other genes can also play a role. Genes like CRTAP and P3H1 (also known as LEPRE1) are involved in collagen processing. Mutations in these genes can also lead to weak collagen production.
A study found that CRTAP and P3H1 mutations are linked to severe OI. This form often includes multiple fractures at birth and significant bone deformities.
Inheritance Patterns: Autosomal Dominant, Recessive, and X-linked Forms
Osteogenesis Imperfecta can be inherited in different ways. The most common is autosomal dominant, where one mutated gene is enough to cause the disease.
|
Inheritance Pattern |
Description |
Genes Involved |
|---|---|---|
|
Autosomal Dominant |
A single copy of the mutated gene causes the condition. |
COL1A1, COL1A2 |
|
Autosomal Recessive |
Two copies of the mutated gene (one from each parent) are required to cause the condition. |
CRTAP, P3H1, others |
|
X-linked |
The mutated gene is located on the X chromosome. |
Specific genes on X chromosome |
Knowing how OI is inherited is key for genetic counseling. By identifying the specific mutation in a family, doctors can help with family planning. This helps understand the risk of the disease in future pregnancies.
The Role of Type I Collagen in Bone Health
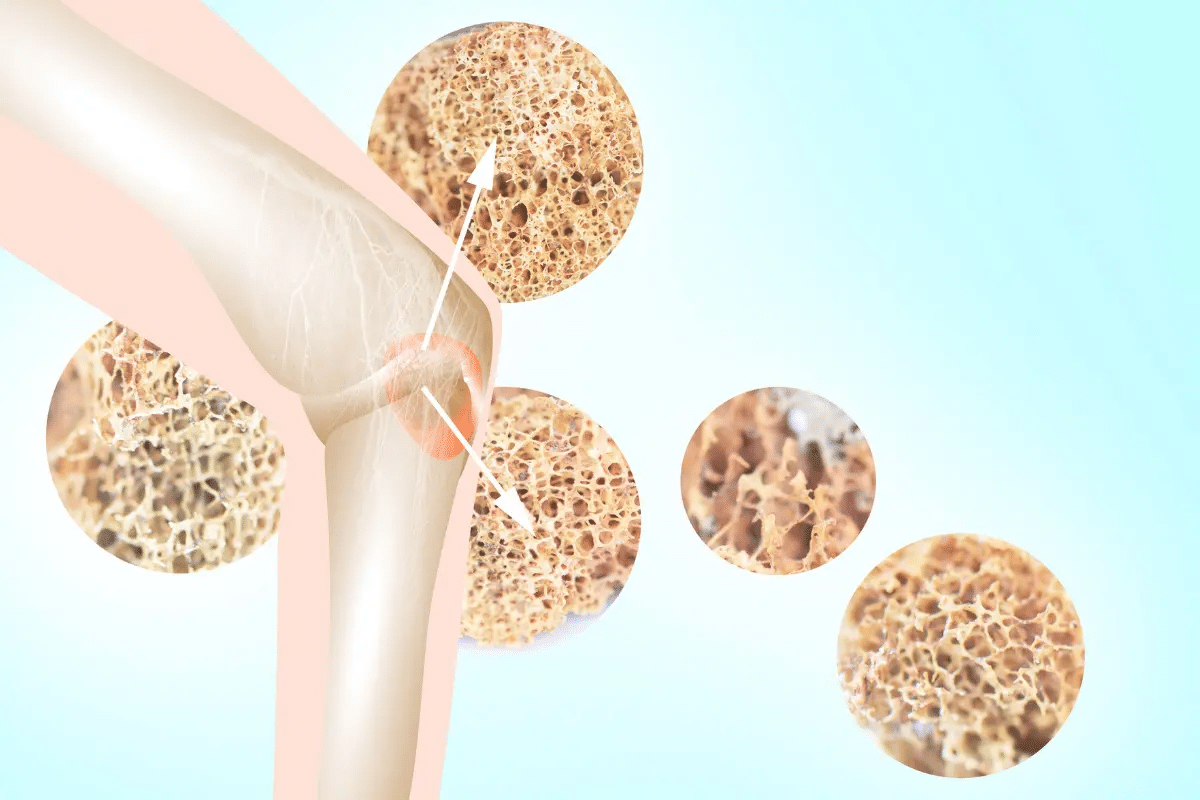
Type I collagen is key to keeping bones strong and healthy. It’s a protein that makes up bones, skin, muscles, and tendons. In bones, type I collagen is very important because it’s the most common type.
The way collagen works in bones is complex. It acts as a base for minerals to attach to, making bones strong. The collagen structure is a triple helix, giving it great strength. This strength helps bones handle stress and support our bodies.
Collagen Structure and Function in Normal Bone Development
In normal bone growth, osteoblasts make type I collagen. These collagen molecules then form fibrils. These fibrils are mineralized with calcium and phosphate, making bones hard.
The process of bone mineralization is carefully controlled. It involves cells, growth factors, and the matrix outside cells. Type I collagen is essential for this process. It helps bones grow strong and support our weight and movement.
How Collagen Deficiency Leads to Bone Fragility
A lack of type I collagen makes bones weak, a sign of osteogenesis imperfecta (OI). In OI, the body either doesn’t make enough collagen or makes it wrong. This makes bones break easily.
Collagen deficiency and bone fragility are linked. Genetic mutations can affect collagen production. Mutations in COL1A1 and COL1A2 genes can lead to bad collagen or less of it. This weakens the bone matrix, making bones more likely to break.
|
Condition |
Effect on Collagen |
Impact on Bone Health |
|---|---|---|
|
Normal Collagen Production |
Normal type I collagen structure and function |
Strong bones with normal density |
|
Type I Collagen Deficiency |
Reduced or defective type I collagen |
Increased bone fragility and fracture risk |
Understanding type I collagen’s role in bone health is vital. It helps us manage conditions like osteogenesis imperfecta better. Knowing how collagen affects bones and what happens when it’s lacking helps us care for people with brittle bones more effectively.
Types of Osteogenesis Imperfecta
Osteogenesis imperfecta, or brittle bones disease, is not just one condition. It’s a range of disorders with different severities. These variations are based on clinical features and genetic traits.
Type I: The Mildest and Most Common Form
Type I osteogenesis imperfecta is the mildest and most common. People with Type I OI usually have few fractures and little bone deformity. They might have blue sclerae, hearing loss, and dental issues. But, they can live active lives with the right care.
Type II: The Most Severe and Often Fatal Form
Type II osteogenesis imperfecta is the most severe and often fatal in infancy. Babies with Type II OI have extremely fragile bones. This leads to many fractures and serious breathing problems. Sadly, many do not live past early childhood.
Type III and IV: Moderate to Severe Manifestations
Types III and IV osteogenesis imperfecta are moderate to severe. Type III has progressive bone deformities and frequent fractures. Type IV is milder, with fewer fractures and less severe deformities. Both types need careful management to improve life quality.
Rarer Types of OI (Types V-XIII)
There are rarer forms of osteogenesis imperfecta, Types V through XIII. These have unique clinical and genetic features. For example, Type V OI has calcification in the forearm. Other rare types may have special skeletal or extraskeletal features.
As research goes on, understanding these different types is key. It helps in developing specific treatments and improving patient care. “The classification of OI into different types helps clinicians tailor their approach to the specific needs of each patient,” says a leading expert in the field.
Signs and Symptoms of Brittle Bones Disease
Brittle Bones Disease, or Osteogenesis Imperfecta, shows different signs and symptoms in people. These symptoms can vary a lot. It’s important to know them to give the right care.
Skeletal Manifestations
Skeletal signs are key in Brittle Bones Disease. These include:
- Frequent Fractures: People with Osteogenesis Imperfecta often break bones easily.
- Bone Deformities: Broken bones can cause bone shape changes, affecting bone function.
The severity of these signs can differ a lot. Some people have many fractures and big bone shape changes. Others might have fewer fractures and less severe changes.
Non-Skeletal Features
Brittle Bones Disease also has non-skeletal signs, like:
- Blue Sclera: Many have blue or grayish sclera because of the tissue’s transparency.
- Dentinogenesis Imperfecta: Teeth can look discolored (blue or yellow) and clear.
- Hearing Loss: Hearing problems are common, affecting how sound is conducted or sensed.
These signs can greatly affect life quality and need careful management.
Symptom Variations Across Different Age Groups
Symptoms of Brittle Bones Disease change with age. Babies and young kids often have fractures and bone shape issues. Adults might face hearing loss and dental problems. It’s key to understand these changes for proper care.
As people with Osteogenesis Imperfecta get older, their symptoms and needs evolve. They need ongoing care and management plan updates.
Diagnosing Osteogenesis Imperfecta
To diagnose Osteogenesis Imperfecta, doctors use several methods. They look at the patient’s history, do imaging tests, and do genetic tests. This helps them figure out if someone has the condition and how severe it is.
Clinical Evaluation and Physical Examination
Doctors start by looking at the patient’s medical history and doing a physical exam. They check for signs like blue sclerae, hearing loss, and bone deformities. They use this to see if the condition is present and how bad it is.
They also check for skeletal deformities and fractures. Finding these signs means they might need to do more tests.
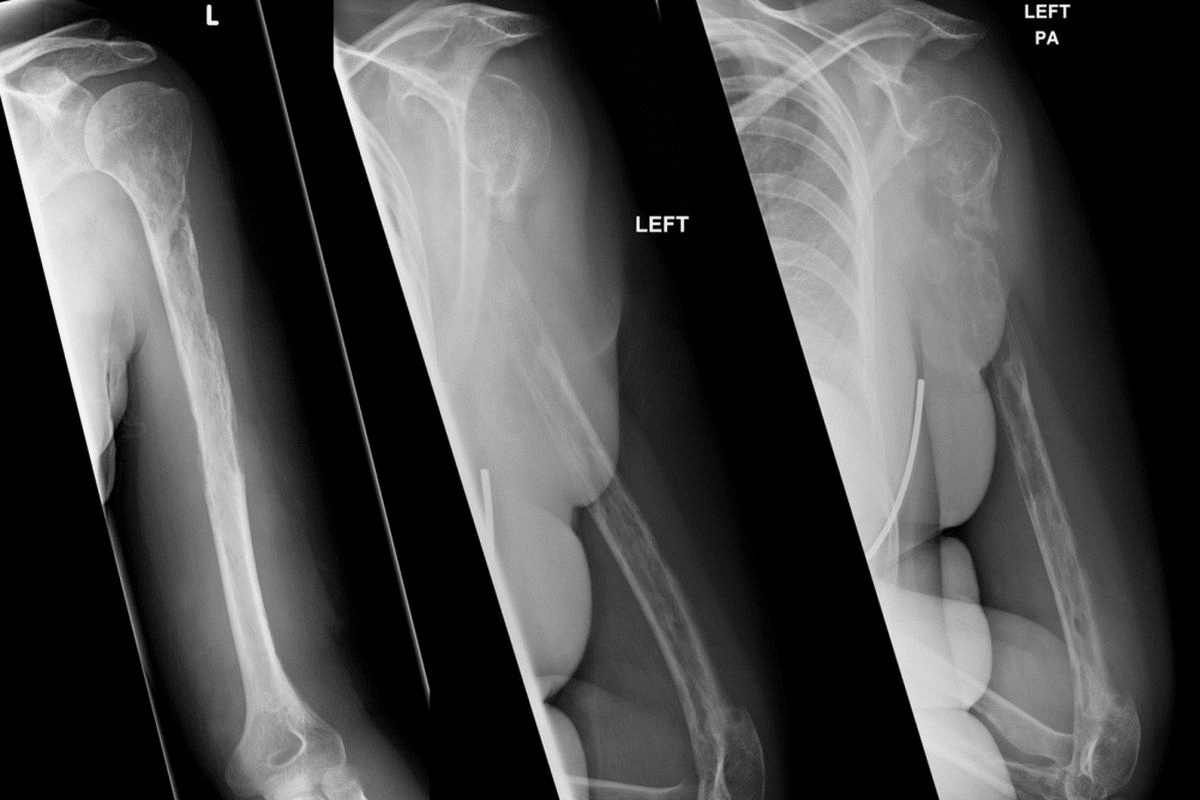
Imaging Studies: X-rays, DXA Scans, and Bone Markers
Imaging tests are key for checking bone health. X-rays help spot fractures or deformities. DXA scans measure bone density, which shows how healthy the bones are. Bone markers also help check bone health.
A leading expert says, “Imaging studies, like X-rays and DXA scans, are very important for diagnosing and managing Osteogenesis Imperfecta.” This shows how important these tests are in diagnosing the condition.
Genetic Testing and Prenatal Diagnosis Options
Genetic testing is a big part of diagnosing Osteogenesis Imperfecta. It finds the gene mutations that cause the condition. It helps confirm the diagnosis and helps with family planning.
There are prenatal tests for families with a history of Osteogenesis Imperfecta. CVS and amniocentesis can find genetic mutations early.
“Prenatal diagnosis allows families to make informed decisions about pregnancy management and prepares them for the possible needs of their child.”
Medical Treatment Options for Brittle Bones Disease
Osteogenesis imperfecta treatment has made big strides, bringing hope to patients and their families. The main goal of treatment is to lower the chance of fractures and improve life quality for those with brittle bones disease.
Bisphosphonate Therapy for Increasing Bone Density
Bisphosphonate therapy is a key treatment for osteogenesis imperfecta. It uses medicines to boost bone density, cutting down fracture risks. Bisphosphonates stop bone resorption, the process where osteoclasts break down bone.
A study in the Journal of Bone and Mineral Research showed bisphosphonate therapy cuts fracture rates in kids with osteogenesis imperfecta. Pamidronate and zoledronic acid are the top bisphosphonates used.
“Bisphosphonate therapy has been shown to improve bone density and reduce fracture risk in patients with osteogenesis imperfecta.”
Surgical Interventions: Rodding and Correction of Deformities
Surgery is vital in managing osteogenesis imperfecta. Rodding is a common surgery where a metal rod is placed in the bone for support and to prevent fractures. This is very helpful for long bones like the femur and tibia.
|
Surgical Procedure |
Purpose |
Benefits |
|---|---|---|
|
Rodding |
To provide internal support to bones |
Reduces fracture risk, improves mobility |
|
Correction of Deformities |
To correct bone deformities |
Improves bone alignment, enhances quality of life |
Emerging Treatments: Gene Therapy and Stem Cell Approaches
Gene therapy and stem cell approaches are new treatments for osteogenesis imperfecta. Gene therapy aims to fix the genetic issues causing the condition. Stem cell therapy tries to grow healthy bone tissue.
Research in these areas is promising. For example, a study in Nature showed gene editing can fix the COL1A1 gene mutation behind osteogenesis imperfecta.
Comprehensive Management Strategies
Managing brittle bones disease needs a full approach. This includes preventing fractures, physical therapy, managing pain, and nutritional support. This strategy is key to bettering life for those with osteogenesis imperfecta.
Fracture Prevention Techniques and Safety Measures
Stopping fractures is vital in managing brittle bones disease. It’s about making a safe space by removing hazards and using padding. Also, using walkers or wheelchairs can help avoid fractures. Safe mobility practices are also key, like taking breaks and avoiding heavy lifting.
Experts say preventing fractures in osteogenesis imperfecta needs a proactive plan. This includes changing the environment and using protective gear. It shows the need for early action in managing the condition.
Physical and Occupational Therapy Approaches
Physical and occupational therapy are very important for brittle bones disease. They help improve how well you move, your strength, and your ability to do daily tasks. Personalized exercise programs aim to boost bone density and lower fracture risk.
- Physical therapy works on muscle strength and flexibility.
- Occupational therapy helps people adapt to their condition and find ways to live daily life.
Pain Management Protocols
Managing pain well is key for those with brittle bones disease. This might include medicine, physical therapy, and other methods like acupuncture. Pain assessment is the first step in creating a plan that meets the person’s needs.
“Pain management in osteogenesis imperfecta needs a full plan that looks at both physical and emotional pain.” Expert Opinion
Nutritional Support for Optimal Bone Health
Good nutrition is vital for bone health in brittle bones disease. Eating foods rich in calcium and vitamin D is important for bone density. Nutritional counseling helps make better diet choices.
|
Nutrient |
Role in Bone Health |
Food Sources |
|---|---|---|
|
Calcium |
Essential for bone density |
Dairy products, leafy greens |
|
Vitamin D |
Critical for calcium absorption |
Fatty fish, fortified dairy products |
Living with Brittle Bones Disease
For those with brittle bones disease, a supportive environment is key to staying independent. This condition, also known as osteogenesis imperfecta, brings unique challenges. We’ll look at how to make homes and schools safe, use adaptive equipment, and offer psychological support to improve life quality.
Creating Safe Home and School Environments
Making a safe space is vital to avoid fractures and keep independence. This means making changes at home and school. Home modifications might include removing hazards, installing handrails, and using non-slip mats. Schools can also adapt classrooms and playgrounds for students with brittle bones disease.
Some important adaptations include:
- Padding sharp corners and edges
- Using wheelchair-accessible ramps and elevators
- Providing extra support during physical activities
- Ensuring that classrooms are organized to minimize clutter and tripping hazards
Adaptive Equipment and Mobility Aids
Adaptive equipment and mobility aids are key to independence and mobility for those with brittle bones disease. Wheelchairs, walkers, and canes offer support and reduce fracture risks. Specialized gear like standing frames and adjustable beds also help maintain bone density and health.
Choosing the right adaptive equipment is important. Healthcare professionals, like occupational therapists, can help pick the best devices for each person’s needs.
Psychological Support and Quality of Life Considerations
Brittle bones disease can affect mental health and overall well-being. Psychological support is vital to address these issues. This support can include counseling, support groups, and stress management.
Improving quality of life also means encouraging social interaction and activities that bring joy. By creating a supportive community and providing access to resources, we can help those with brittle bones disease live more fulfilling lives.
Conclusion: Advances in Understanding and Managing Osteogenesis Imperfecta
We’ve made big strides in understanding and managing osteogenesis imperfecta, a condition where bones are very brittle. New research and better medical treatments are helping us manage it well.
Genetic studies have helped us understand what causes osteogenesis imperfecta. This knowledge helps doctors diagnose and treat it better. We now know more about type I collagen and its role in bone health. This info is leading to new treatments.
Dealing with osteogenesis imperfecta needs a full plan. This includes medical care, physical therapy, and making lifestyle changes. Treatments like bisphosphonates, surgery, and even gene therapy are being used. They help make bones stronger and lower the chance of fractures.
As we learn more about osteogenesis imperfecta, we’re making life better for those with it. With the right support and care, people with brittle bones can live active and happy lives.
FAQ
What is osteogenesis imperfecta?
Osteogenesis imperfecta, also known as brittle bones disease or glass bone syndrome, is a genetic disorder. It affects the production of type I collagen, a key protein for bone strength.
What causes brittle bones disease?
Brittle bones disease is mainly caused by genetic mutations. These mutations affect type I collagen production, found in genes like COL1A1 and COL1A2. Other genes, such as CRTAP and P3H1, also play a role.
How is osteogenesis imperfecta inherited?
Osteogenesis imperfecta can be inherited in different ways. It can be autosomal dominant, recessive, or X-linked. This makes genetic counseling important for family planning.
What are the different types of osteogenesis imperfecta?
There are several types of osteogenesis imperfecta. They are classified based on clinical features and genetic characteristics. Types range from I (the mildest) to II (the most severe), and include rarer types like V-XIII.
What are the signs and symptoms of brittle bones disease?
Symptoms of brittle bones disease vary. They include frequent fractures and bone deformities. Other signs are blue sclera, dentinogenesis imperfecta, and hearing loss.
How is osteogenesis imperfecta diagnosed?
Diagnosing osteogenesis imperfecta involves several steps. It includes clinical evaluation, physical examination, imaging studies, and genetic testing. Prenatal diagnosis is also available for families with a history of the condition.
What are the treatment options for brittle bones disease?
Treatment options for brittle bones disease include bisphosphonate therapy. This increases bone density. Surgical interventions like rodding are also used. New treatments like gene therapy and stem cell approaches are emerging.
How can brittle bones disease be managed comprehensively?
Managing brittle bones disease requires a multi-disciplinary approach. It includes fracture prevention, physical and occupational therapy, pain management, and nutritional support. These help promote optimal bone health.
What is the role of type I collagen in bone health?
Type I collagen is essential for bone health. It provides strength and structural integrity. A deficiency or defect in type I collagen leads to bone fragility, characteristic of osteogenesis imperfecta.
How can individuals with brittle bones disease improve their quality of life?
Improving the quality of life for individuals with brittle bones disease is important. Creating safe environments, using adaptive equipment, and providing psychological support are key. These address the complex needs of those affected.
What is Vrolik syndrome?
Vrolik syndrome is another name for osteogenesis imperfecta. It refers to the more severe forms of the condition.
What is Lobstein syndrome?
Lobstein syndrome is also known as osteogenesis imperfecta. It describes the condition’s milder forms.
What is glass bone disease?
Glass bone disease is a colloquial term for osteogenesis imperfecta. It describes the condition’s characteristic bone fragility.
Reference
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4927363/






