Cerebral amyloid angiopathy (CAA) is a big health issue for older people. It affects up to 60% of seniors with brain problems. Early diagnosis is key to avoid serious problems like brain hemorrhages and losing cognitive skills amyloid brain disease.
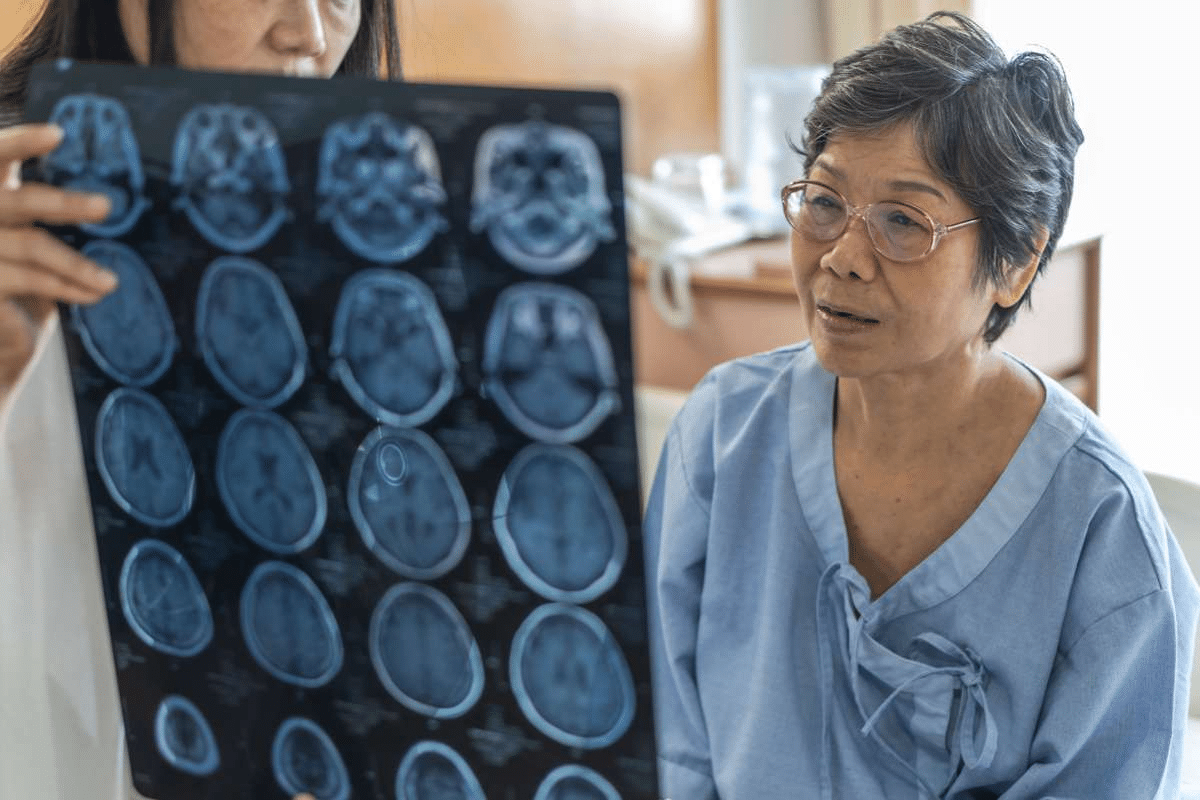
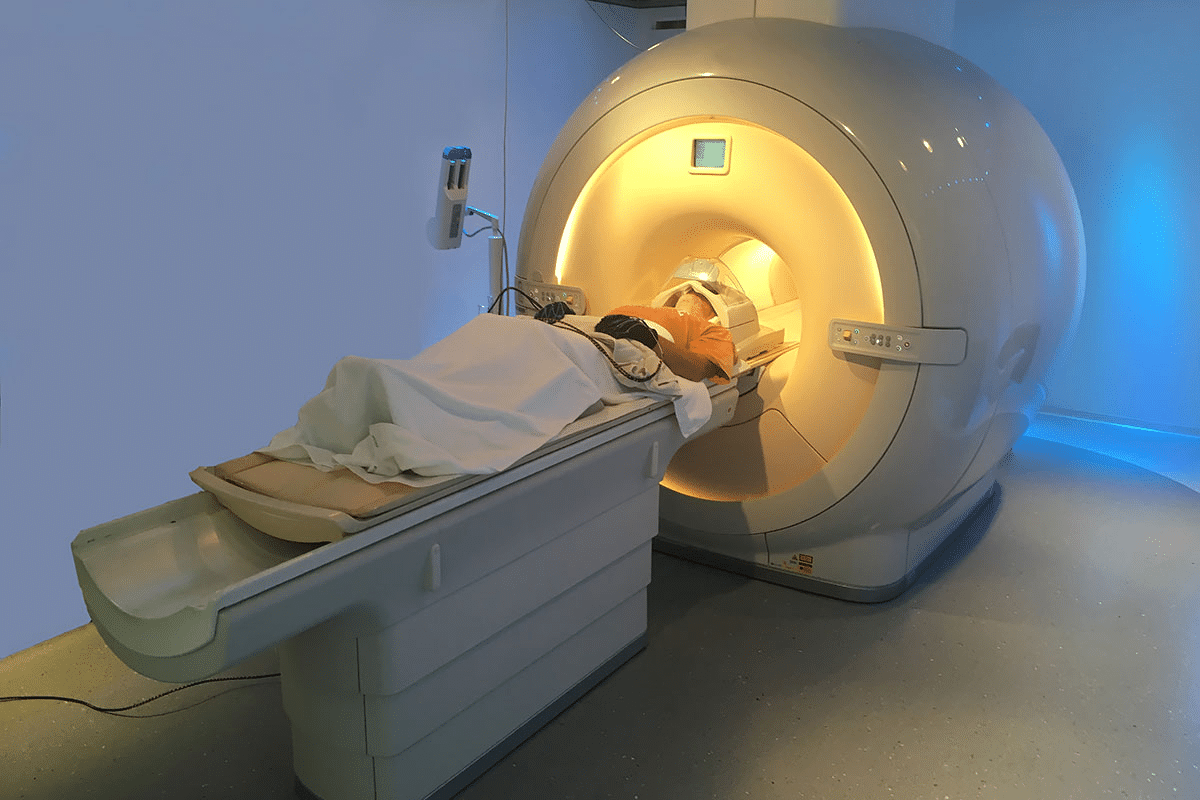
Liv Hospital uses top-notch MRI scans to find CAA early. MRI is a key tool for spotting CAA. It can find signs of both bleeding and non-bleeding in the brain.
Doctors need to know how to read MRI scans to help patients with CAA. This knowledge helps them give the right care fast.
Key Takeaways
- Early diagnosis of CAA is critical to prevent cognitive decline and brain hemorrhages.
- MRI neuroimaging plays a vital role in detecting CAA markers.
- Advanced MRI sequences improve diagnostic accuracy for CAA.
- Understanding MRI markers and diagnostic criteria is essential for timely care.
- CAA affects a significant portion of the elderly population with cognitive issues.
Understanding Cerebral Amyloid Angiopathy as an Amyloid Brain Disease
Cerebral amyloid angiopathy (CAA) is a condition where amyloid-beta peptides build up in blood vessel walls. It’s a major amyloid brain disease. Knowing about CAA is key for diagnosing and treating it.
Pathophysiology of Amyloid-Beta Deposition in Cerebral Vessels
CAA happens when amyloid-beta peptides gather in blood vessels. This makes them weak and can cause them to burst. Many things, like genes and age, can affect this process.
We’ll look into how amyloid-beta affects blood vessels. We’ll also talk about what this means for diagnosing CAA.
Epidemiology and Age-Related Prevalence
CAA gets more common with age. Almost all people over 80 have some CAA. Knowing this helps us understand its impact on older people.
|
Age Group |
Prevalence of CAA |
|---|---|
|
60-69 years |
20% |
|
70-79 years |
50% |
|
80+ years |
nearly 100% |
Genetic Factors and Risk Assessment
Genes, like the apolipoprotein E (APOE) genotype, affect CAA risk. Some APOE genotypes increase the risk of CAA. This shows why genetic tests are important for assessing risk.
We’ll explore how genes influence CAA. We’ll see how they affect the disease’s progression and diagnosis.
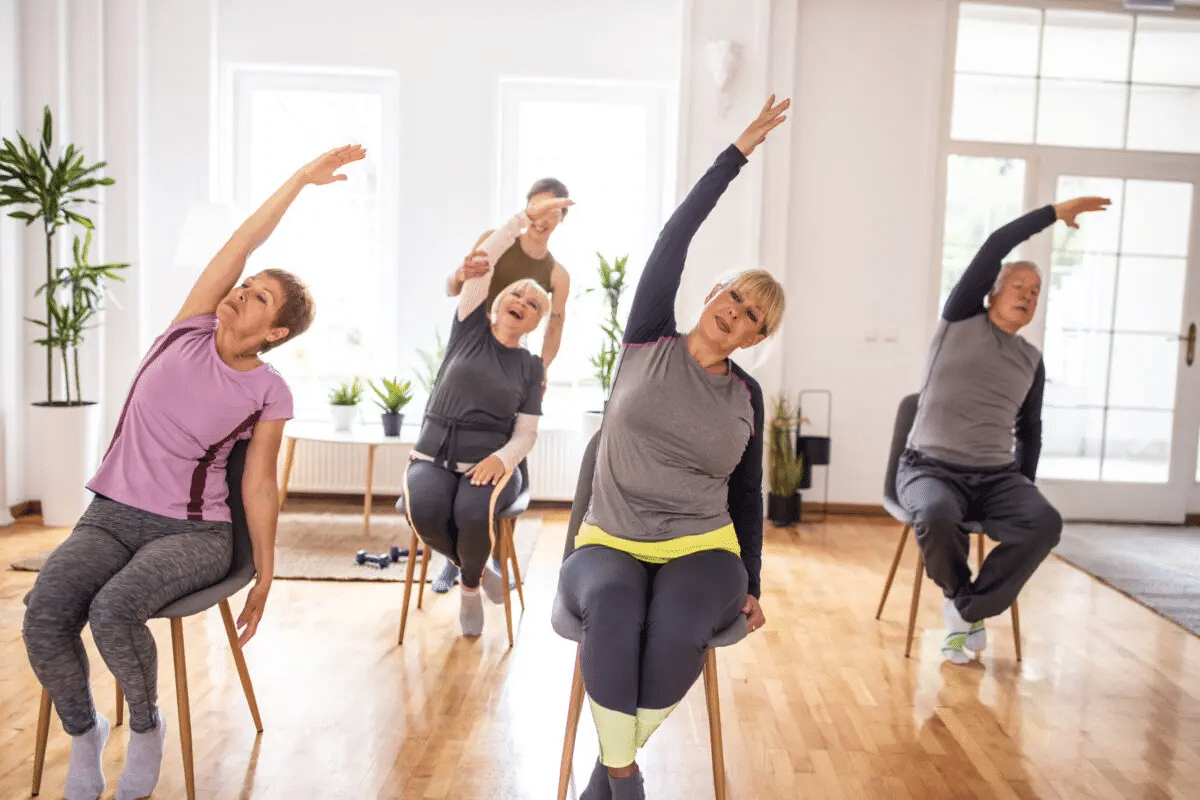
Clinical Presentations of Cerebral Amyloid Angiopathy

Cerebral Amyloid Angiopathy (CAA) shows different symptoms that help in early diagnosis and treatment. It happens when amyloid beta peptides build up in the brain’s blood vessels. This leads to various neurological problems.
Spontaneous Lobar Hemorrhages
One key symptom of CAA is spontaneous lobar hemorrhages. These happen when blood vessel walls weaken due to amyloid buildup. This can be very dangerous.
Transient Neurological Episodes
People with CAA might have short-term neurological issues. These can affect speech, movement, or feeling. These episodes are like TIAs but need a specific diagnosis.
Progressive Cognitive Decline
CAA also causes a gradual decline in thinking skills. This can range from mild memory loss to dementia. The buildup of amyloid and tissue damage are the main causes.
Because CAA shows different symptoms, a detailed diagnosis is key. This includes both clinical checks and imaging studies. This helps in accurately diagnosing and treating CAA.
The Boston Criteria Version 2.0 for CAA Diagnosis
The diagnosis of cerebral amyloid angiopathy (CAA) uses the Boston Criteria. These have been updated to make diagnosis more accurate. The new version includes advanced imaging and clinical findings to help diagnose.
Criteria for Probable CAA
Probable CAA is diagnosed with specific MRI findings. These include lobar hemorrhages or microbleeds. These signs help tell CAA apart from other causes of bleeding.
Criteria for Possible CAA
Possible CAA is when the criteria aren’t fully met or other causes of bleeding are present. This category shows the complexity and variety of CAA.
Using the Boston Criteria Version 2.0 helps doctors diagnose CAA better. Knowing and using these criteria helps manage patients with this condition.
Essential MRI Protocols for CAA Assessment
Diagnosing cerebral amyloid angiopathy (CAA) depends on MRI protocols. These protocols help spot changes in the brain. Using both conventional and advanced MRI sequences is key for a correct diagnosis.
Conventional MRI Sequences
Conventional MRI sequences, like T1-weighted and T2-weighted images, are a starting point. They help see structural changes in the brain.
Susceptibility-Weighted Imaging (SWI) and Gradient-Recalled Echo (GRE)
SWI is great at finding hemorrhages and spotting microbleeds. GRE sequences also help find hemorrhagic changes.
|
Sequence |
Description |
Utility in CAA Diagnosis |
|---|---|---|
|
T1-weighted |
Provides detailed anatomy |
Assesses structural changes |
|
T2-weighted |
Sensitive to changes in tissue |
Identifies edema and lesions |
|
SWI |
Highly sensitive to hemorrhages |
Detects microbleeds |
Identifying Hemorrhagic Markers of CAA on MRI
Cerebral Amyloid Angiopathy (CAA) is a condition where amyloid protein builds up in brain blood vessels. This buildup can cause bleeding in the brain. Finding signs of bleeding is key to diagnosing and treating CAA.
Lobar Cerebral Microbleeds
Lobar cerebral microbleeds are a key sign of CAA. These tiny bleeds show up on MRI scans. They are found in the brain’s lobes and raise the risk of more bleeding.
Cortical Superficial Siderosis
Cortical superficial siderosis is another important sign of CAA. It happens after bleeding in the brain’s covering. MRI scans can spot it as dark spots. It’s linked to brain decline in people with CAA.
Lobar Intracerebral Hemorrhage
Lobar intracerebral hemorrhage is a serious sign of CAA. It’s when big bleeds happen in the brain’s lobes. These bleeds can greatly affect a patient’s outcome. Finding these bleeds early is critical for better care.
Spotting these signs is vital for diagnosing and treating CAA. By recognizing these signs, doctors can provide the right care and support to those affected.
Non-Hemorrhagic MRI Markers in CAA Diagnosis
Non-hemorrhagic markers are key in diagnosing cerebral amyloid angiopathy (CAA). They offer insights into the disease’s progression. This helps us understand its effects on the brain.
White Matter Hyperintensities
White matter hyperintensities (WMH) are common in CAA patients. They show up on MRI, mainly in the FLAIR sequence. WMH are linked to aging, high blood pressure, and other vascular risks.
Enlarged Perivascular Spaces
Enlarged perivascular spaces (EPVS) are another marker in CAA. EPVS are fluid-filled spaces around blood vessels, visible on MRI. They are often found in the basal ganglia and centrum semiovale. EPVS are linked to cognitive decline and small vessel disease.
Cortical Microinfarcts
Cortical microinfarcts are small ischemic lesions seen on MRI. They are linked to CAA and cognitive decline. These small lesions are hard to spot but are key markers of cerebral small vessel disease.
Understanding these non-hemorrhagic markers is vital for diagnosing and managing CAA. Recognizing WMH, EPVS, and cortical microinfarcts helps healthcare providers treat patients better.
Differential Diagnosis of Amyloid Brain Disease on MRI
Distinguishing CAA from other vascular conditions is vital. This is because they can look similar on scans and in symptoms. Getting the diagnosis right is key for the right treatment.
Hypertensive Microangiopathy vs. CAA
Hypertensive microangiopathy and CAA share some traits. But, they also have key differences. Knowing these differences is critical for making the right diagnosis.
- Distribution of Lesions: CAA mainly affects the lobar parts of the brain. Hypertensive microangiopathy can hit deeper brain areas.
- Presence of Microbleeds: Both can show microbleeds, but in different spots. CAA’s microbleeds are in the lobes, while hypertensive microangiopathy’s are deeper.
Differential Diagnosis Considerations
When diagnosing CAA, other conditions must be ruled out. These include:
- Vascular dementia
- Cerebral vasculitis
- Other small vessel diseases
A detailed medical history and imaging studies are essential. They help tell CAA apart from these other conditions.
Advanced Neuroimaging Techniques in CAA Assessment
Advanced neuroimaging has changed how we diagnose and understand Cerebral Amyloid Angiopathy (CAA). These methods offer deep insights into CAA’s pathology and how it progresses.
Amyloid PET Imaging Correlation
Amyloid PET imaging is a key tool for spotting amyloid in the brain. This is a key sign of CAA. Research shows it can pinpoint CAA patients and show how severe the disease is.
Role of Diffusion Tensor Imaging
DTI is a special MRI that checks the brain’s white matter tracts. It’s useful in CAA because it spots changes in these tracts linked to the disease.
Functional MRI Applications in CAA
fMRI looks at brain activity in CAA patients. It helps us grasp the disease’s neural basis. It also aids in finding new treatments.
|
Technique |
Description |
Application |
|---|---|---|
|
Amyloid PET Imaging |
Detects amyloid deposits |
Diagnosis and assessment of CAA severity |
|
Diffusion Tensor Imaging (DTI) |
Assesses white matter integrity |
Identifying microstructural changes |
|
Functional MRI (fMRI) |
Assesses brain activity patterns |
Understanding neural mechanisms |
Conclusion: Clinical Implications and Reporting Best Practices
Getting Cerebral Amyloid Angiopathy (CAA) right on MRI matters a lot for patient care. Knowing how to diagnose and report it is key to helping patients.
When MRI spots CAA, it changes how doctors treat patients. It can even help patients get better. It’s important for doctors and radiologists to talk clearly about MRI results for CAA.
Using the Boston Criteria Version 2.0 and the right MRI scans helps doctors make accurate diagnoses. This information helps doctors decide on treatments and predict how well patients will do. Clear and simple MRI reports help doctors work together better.
Good patient care starts with accurate CAA diagnosis and reporting. By following the best practices and keeping up with new research, healthcare teams can do better for their patients.
FAQ
What is cerebral amyloid angiopathy (CAA) and how is it related to amyloid brain disease?
Cerebral amyloid angiopathy is a condition where amyloid-beta peptides build up in blood vessel walls. This makes them weak and prone to rupture. It’s a big worry for older people and can lead to memory loss and bleeding in the brain.
What is the role of MRI in diagnosing CAA?
MRI is key in spotting CAA. It can find signs of the disease, like bleeding and non-bleeding markers. New MRI scans, like susceptibility-weighted imaging (SWI), help doctors diagnose CAA better.
What are the clinical presentations of CAA?
CAA can show up in different ways. People might have sudden brain bleeds, short-term brain problems, or slow memory loss. Doctors look for these signs to diagnose CAA.
What are the Boston Criteria Version 2.0, and how are they used in CAA diagnosis?
The Boston Criteria Version 2.0 is a big step forward in diagnosing CAA. It uses both clinical signs and MRI findings. It helps doctors decide if someone has probable or possible CAA based on MRI markers.
What are the essential MRI protocols for assessing CAA?
To check for CAA, MRI uses special scans. These include regular MRI, susceptibility-weighted imaging (SWI), and T2*-weighted gradient-recalled echo (GRE). These scans help spot signs of CAA.
What are the hemorrhagic markers detectable on MRI that are associated with CAA?
MRI can find signs of CAA like small brain bleeds, bleeding under the brain’s surface, and big brain bleeds. Knowing about these signs is important for diagnosing CAA and predicting future bleeds.
What are the non-hemorrhagic MRI markers that are important for CAA diagnosis?
MRI also looks for signs that aren’t related to bleeding. These include white matter changes, big spaces in the brain, and tiny brain strokes. These signs show how CAA affects the brain.
How is CAA differentiated from other conditions that affect the brain’s small vessels or cause similar MRI findings?
To tell CAA apart from other brain problems, doctors look at MRI findings. They compare them with other conditions like high blood pressure damage, other vascular issues, and bleeding from trauma. Knowing the differences helps doctors make accurate diagnoses.
What are the advanced neuroimaging techniques being explored for CAA assessment?
New imaging methods are being tested for CAA. These include amyloid PET scans, diffusion tensor imaging, and functional MRI. They might help us understand and diagnose CAA better.
What are the clinical implications of accurately diagnosing CAA using MRI?
Accurate CAA diagnosis with MRI is very important. It helps doctors manage patients better and might improve their outcomes. It’s key for doctors and radiologists to communicate clearly about MRI findings for CAA.
How does the deposition of amyloid-beta affect cerebral vessels?
Amyloid-beta buildup in blood vessel walls makes them weak. This can lead to rupture and contribute to CAA.
What is the significance of genetic factors, such as APOE genotype, in the prevalence and risk assessment of CAA?
Genes, like APOE, play a role in amyloid-beta buildup. They affect the risk of getting CAA. Knowing about these genes is important for diagnosing and assessing risk.
Reference
National Center for Biotechnology Information. MRI Diagnosis of Cerebral Amyloid Angiopathy in Seniors. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC6501479/