Explore advanced lung disease treatments at LIV Hospital. From non-surgical therapies to pediatric lung surgery recovery, we provide expert care.
Send us all your questions or requests, and our expert team will assist you.
For years, the standard treatment for chronic lung diseases like COPD and Asthma was limited to inhalers and steroids. While these medications manage symptoms, they often fail to address the structural problems causing the breathlessness. Patients were told, “This is as good as it gets.”
At Liv Hospital, we reject that limitation. We have entered the era of Interventional Pulmonology—a cutting-edge field that sits between medical therapy and thoracic surgery. Using advanced endoscopic techniques, we can now mechanically repair airways, remove obstructions, and reduce lung volume without making a single incision on your chest.
Our Treatment and Management philosophy is holistic. We combine these high-tech interventions with personalized Biologic Therapies (Smart Drugs) and comprehensive Pulmonary Rehabilitation to restore not just your lungs, but your lifestyle. Whether you are an athlete with exercise-induced asthma or a senior struggling with emphysema, our goal is to help you breathe easier, sleep better, and live longer.
Chronic Obstructive Pulmonary Disease (COPD) is characterized by air trapping. The damaged air sacs lose their elasticity, causing old air to get stuck inside. This turns the chest into a hyper-inflated balloon, leaving no room for fresh air.
This is a revolutionary, non-surgical alternative to “Lung Volume Reduction Surgery.”
For patients who are not candidates for valves (due to “collateral ventilation” between lung lobes), we use Coils.
When standard inhalers (corticosteroids/bronchodilators) are not enough to control asthma attacks, we escalate to precision medicine.
Severe asthma is often driven by specific immune pathways. We don’t just suppress the immune system; we target the specific trigger.
For patients with thickened airway muscles that spasm uncontrollably.
While oncologists treat the cancer cells, Interventional Pulmonologists manage the complications, such as blocked airways or fluid buildup.
Tumors often grow into the main windpipe (trachea) or bronchi, causing suffocation.
For patients with “Malignant Pleural Effusion” (fluid recurring around the lung).
Obstructive Sleep Apnea (OSA) is a mechanical problem: the throat collapses during sleep.
Continuous Positive Airway Pressure (CPAP) is the gold standard, but adherence is low if the mask doesn’t fit.
For mild-to-moderate apnea or patients who refuse CPAP.
Chronic lung disease leads to a vicious cycle: you get breathless, so you stop moving; you stop moving, so your muscles get weak; your muscles get weak, so you get breathless faster. Pulmonary Rehab breaks this cycle.
Liv Hospital is a reference center for complex respiratory infections.
Quitting is the single most effective treatment for any lung disease. It is not just about willpower; it is about neurochemistry.
Send us all your questions or requests, and our expert team will assist you.
Always use a spacer if prescribed, shake the canister, exhale fully, seal your lips around the mouthpiece, press the canister once while inhaling slowly and deeply, and hold your breath for 10 seconds.
COPD cannot be cured or reversed, but treatment can manage symptoms, slow the progression of the disease, and improve quality of life significantly.
A rescue inhaler (usually albuterol) is a fast-acting medication used to quickly open airways during an asthma attack or sudden shortness of breath; it is not for daily control.
No, oxygen is not addictive. Your body needs it to survive, and using it as prescribed simply brings your blood oxygen levels into a healthy range.
You should clean the mask and tube daily with mild soap and water, and clean the humidifier chamber and filters weekly to prevent bacterial growth and infections.

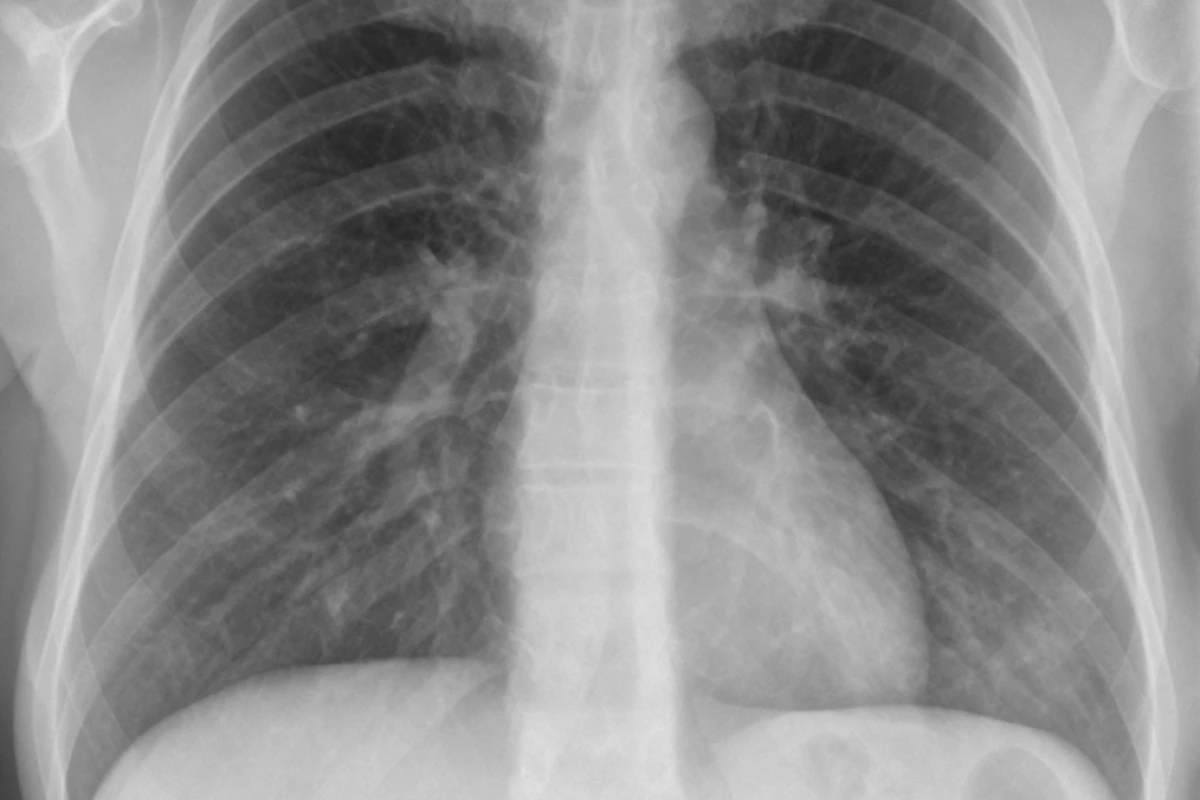
Knowing what a normal chest X-ray looks like is key to spotting health issues early. At Liv Hospital, we use the latest imaging tech and

Review 7 best med for sneezing options. Find quick relief from annoying allergy symptoms and persistent nasal irritation safely. Sneezing and a runny nose can
It’s important to know if a cold can develop into pneumonia. This knowledge helps protect your respiratory health. A common cold might seem mild, but

Using diphenhydramine for sleep requires care. Read this critical guide on proper usage and when to consult a doctor for insomnia. Do you sometimes have

The CSA medical abbreviation has many meanings in healthcare. Each one is important in its own way. Knowing these meanings helps doctors and patients talk

Asthma is a chronic condition that affects millions worldwide. It can be managed with proper care, but severe asthma attacks can be life-threatening. Many wonder:

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)