Plastic surgery restores form and function through reconstructive procedures, cosmetic enhancements, and body contouring.
Send us all your questions or requests, and our expert team will assist you.
The first few months after treatment are the “danger zone” for recurrence. The body is actively trying to heal, and in keloid patients, this means it is attempting to over-heal. Maintenance is not passive; it is an active phase of treatment.
Patients must be vigilant. The transition from acute surgical recovery to long-term scar management involves a seamless handoff to silicone, pressure, and medication. Consistency during this window often determines the success or failure of the entire intervention.

Once the wound is healed (sutures out, no scabs), pressure therapy begins. For earlobes, this means wearing pressure earrings (clips or magnets) for at least 12 to 18 hours a day. The pressure should be snug but not painful.
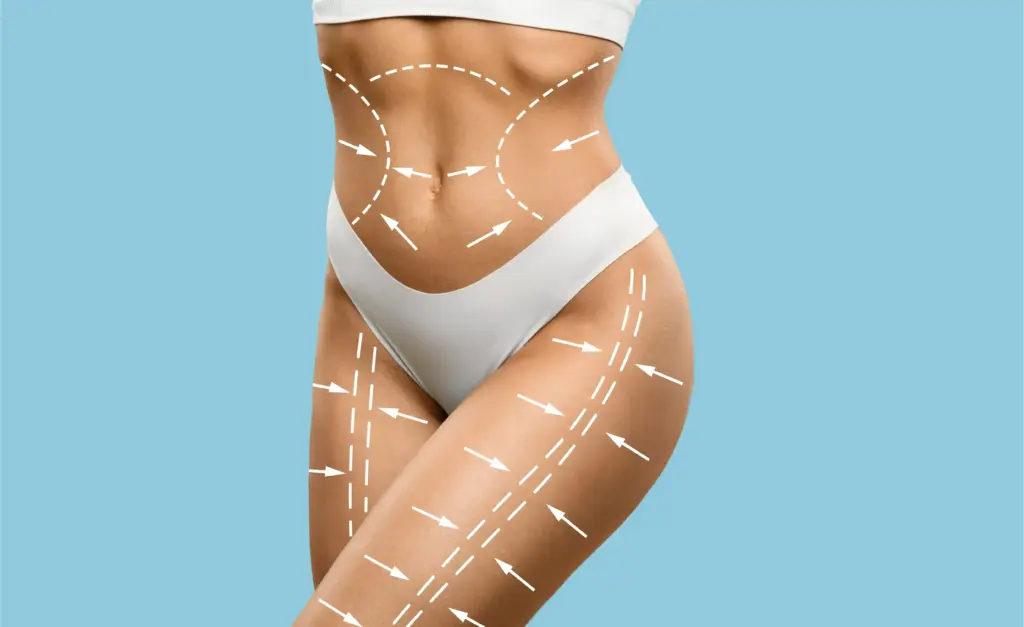
For body scars, tight compression garments are worn. The pressure reduces blood flow to the scar bed, starving the fibroblasts of the oxygen they need to overproduce collagen. This must be continued for 6 to 12 months.

Silicone is the daily maintenance staple. Patients apply silicone gel twice daily or wear silicone sheets for 12-24 hours a day. The sheets also provide some mechanical protection.
The silicone creates a hydrated environment that downregulates scar formation. It also reduces redness and itching. This simple, non-invasive habit is a powerful adjunct to the surgical and medical treatments.
Even after surgery, the surgeon will schedule monthly checks. If the scar shows any sign of thickening, itching, or redness, an injection of steroids or 5-FU is administered immediately.
This “suppressive” approach nips recurrence in the bud. Some protocols involve scheduled injections every 4-6 weeks, regardless of appearance, for the first few months to guarantee suppression of the fibroblast activity.

Vascular lasers (PDL) can be used starting a few weeks after surgery to remove the red color from the scar. By destroying the new blood vessels that are forming to feed the scar, the laser limits the resources available for growth.
Fractional lasers can later be used to blend the scar’s texture with the surrounding skin. These treatments are typically done in a series, spaced 4 to 6 weeks apart, to refine the aesthetic result.
UV radiation causes inflammation in the skin. Inflammation triggers keloids. Therefore, sun protection is a medical necessity, not just for looks. Sun exposure can also cause the scar to turn permanently dark (hyperpigmentation).
Patients must cover the scar with tape, clothing, or high-SPF sunscreen containing zinc or titanium. This protection should be rigorous for at least the first year of healing.


Send us all your questions or requests, and our expert team will assist you.

Once the wound is stable, scar massage helps to break up collagen bundles and keep the tissue pliable. It also helps with desensitization if the nerves are hypersensitive.
Patients are taught to massage the scar firmly in a circular motion for a few minutes daily. This mechanical stress (in a controlled manner) helps align the collagen fibers parallel to the skin, resulting in a flatter, softer scar.
Patients are educated on the “prodromal” symptoms of recurrence. Itching and pain often precede visible growth. If a patient feels the scar becoming itchy or sensitive, they must return to the clinic immediately.
Early detection allows for a quick injection, which can stop the recurrence in its tracks. Waiting until the keloid is visibly large again makes it much harder to treat.
Keloid management is a chronic care model. Follow-up does not end when the stitches come out. Patients are typically followed for at least 1 to 2 years. Recurrence can happen 18 months or more after surgery.
This long-term relationship ensures that the patient has support and access to treatment if the biology of their skin changes or if the scar reactivates.
A common side effect of steroid injections is skin atrophy (divots/thinning) or telangiectasia (spider veins). If this occurs, the injections are paused or diluted.
Fillers can be used to plump up an atrophic dent. Vascular lasers can zap the spider veins. The goal is to balance keloid suppression with the preservation of healthy skin quality.
Successful treatment brings immense relief. Patients often report feeling “lighter” without the pain and itch, and more confident without the visible growth. The end of the active treatment phase marks a return to normalcy.
Integrating the scar—now flat and pale—into one’s self-image is the final step. While the skin will never be perfect, achieving a stable, asymptomatic state is a significant victory in the battle against pathological scarring.


Usually, no. An experienced doctor can diagnose a keloid or hypertrophic scar just by looking at it and feeling it. We only do a biopsy if the scar seems unusual, is bleeding, or we suspect it might be something else, like a skin tumor.
We typically recommend wearing them for at least 6 months to a year, especially at night. If you stop too soon, the blood flow returns, and the keloid can regrow. It requires patience and discipline.
No scar ever disappears completely. The goal is a flat, pale, soft line that is flush with your skin. It will likely always be slightly different in texture or color than your normal skin, but it should not be a raised lump.
We generally advise against tattooing over a keloid scar. The trauma of the tattoo needle can trigger a keloid and cause it to grow again. If you must, wait at least 2 years after it has been stable, and do a small test spot first.
Once the incision is fully healed (usually 4-6 weeks), exercise is fine. However, if the scar is on your chest or shoulder, we may ask you to limit heavy lifting or chest exercises for a few months to avoid stretching the scar while it strengthens.








Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)